Translate this page into:
A study to assess anxiety, stress and depression among private medical practitioners during COVID-19 pandemic: An observational study
*Corresponding author: Vishal Malhotra, Department of Community Medicine, GMC Patiala, Punjab, India. doctor.vishal1978@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Goel S, Patra A, Malhotra V, Kaura S. A study to assess anxiety, stress and depression among private medical practitioners during COVID-19 pandemic: An observational study. Indian J Physiol Pharmacol 2022;66:139-45.
Abstract
Objectives:
This study aims to assess the magnitude of anxiety, stress, and depression among private practitioners during the COVID pandemic 2020.
Materials and Methods:
A descriptive, observational and cross-sectional study was done using a semi-structured questionnaire through electronic media in the form of Google Forms. Patient health questionnaire 4 (PHQ-4) and Perceived Stress Scale-10 were incorporated into the questionnaire to assess the psychological status in November 2020.
Results:
A total of 157 private practitioners participated in the study. Males constituted 60%. Participants have mean age (SD) of 44.2 (6.9) years with work experience and a mean (SD) of 16.3 (6.78) years. The anxiety and depression subscales of the PHQ-4 scale showed that 54.7% of the private practitioners have anxiety subscale ≥3 and 28% have depression subscale >3 needing further psychiatric evaluation. Significant predictors of anxiety and depression were female gender, younger and less experienced, and those providing inpatient services in COVID care isolation facilities.
Conclusion:
There is a high prevalence of anxiety, stress, and depression among private practitioners comparable with other countries.
Keywords
Private practitioners
Stress
Anxiety
Depression
INTRODUCTION
The emergence of a new strain of coronavirus and the declaration of the outbreak as an international health emergency by the World Health Organization (WHO in 2020) has created havoc with all healthcare systems across the globe, there has been tremendous pressure on the healthcare workers (HCWs) due to long duration of working hours, lack of PPEs and due to stress of catching the infection and take it to their homes. Private practitioners which used to play a very important role in the healthcare system of India, catering to the majority of patients in the urban areas of the country, are facing additional stresses of huge financial losses due to a drop in patient OPDs to nil initially due to lockdowns and later on when the pandemic picks up then, the anxiety of catching coronavirus and government regulations of mandatory testing before procedures. The private practitioners in private institutions and medical colleges are suffering from significant anxiety, depression, and stress.[1] The psychological impact of novel coronavirus among HCWs has been studied in a number of healthcare facilities across the globe. A study done in Manipal Academy of Health Sciences in India, in Karnataka, has shown that there was high-level stress of 3.7%, while the prevalence rates of healthcare practitioners (HCPs) with depressive symptoms requiring treatment and anxiety symptoms requiring further evaluation were 11.4% and 17.7%, respectively,[1] while a study done in China showed mild-to-moderate depression in 11.4%, anxiety in 22.6% and moderate-to-severe fear in 43– 26% of the HCWs.[2] The current observational, descriptive and cross-sectional study was done to find out the level of anxiety, stress, and depression among private HCPs.
Studies have been done mostly on HCWs working in large COVID care facilities run by either public or large private sector multispecialty and corporate hospitals. However, there is a paucity of data regarding the psychological well-being of the individual private practitioners who are running their small hospitals, clinics, nursing homes, and OPDs, in the first wave of the COVID pandemic in 2020, which need further exploration and evaluation.
Aims and objectives
1) This study aims to assess the magnitude of anxiety, stress, and depression among private practitioners during the COVID pandemic 2020.
MATERIALS AND METHODS
The Google Forms was created and after pre-testing it, the link to the online questionnaire was circulated through WhatsApp to the private practitioners. A purposive and convenience sampling methodology was used for the selection of the private practitioners of district Patiala. A maximum of three reminders were sent to the private practitioner to fill out the form. The study was conducted in November 2020. The questionnaire consisted of three sections, namely baseline information and patient health questionnaire 4 (PHQ-4) (for generalised anxiety disorder and depression). PHQ-4 total score ranges from 0 to 12, with categories of psychological distress being:
None 0–2
Mild 3–5
Moderate 6–8
Severe 9–12
Anxiety subscale = sum of items 1 and 2 (score range, 0–6)
Depression subscale = sum of items 3 and 4 (score range, 0–6)
On each subscale, a score of 3 or greater is considered positive for screening purposes and Perceived Stress Scale 10 (PSS-10) for stress. Individual scores on the PSS can range from 0 to 40 with higher scores indicating higher perceived stress. Scores ranging from 0 to 13 would be considered low stress. Scores 14–26 would be considered moderate stress and scores from 27 to 40 would be considered high perceived stress. The advantage of the PHQ-4 over the PHQ-9 and GAD-7 is that it is an ultra-brief screener of both anxiety and depression. The target health workforce was fighting a pandemic, so in a limited time and resource setting, this tool was very useful to assess the psychological status of the study participants. It has been recommended that total scores for the PHQ-4 of ≥6, or PHQ-2 or GAD-2 of ≥3 are considered ‘yellow flags’ and a PHQ-4 of ≥9, or PHQ-2 or GAD-2 of ≥5 as ‘red flags.[3,4] Data will be collected anonymously with only one response permitted from each person. Ethical approval was duly taken from the Institutional Ethical Committee and review board before the commencement of the study.
Sample size calculations
Considering an estimated prevalence of depression to be 11.4%, anxiety 17.7% and high stress level to be 3.7.[1]
Absolute precision of 5% at 95% confidence interval.
Using formula: Sample size n = (DEFF*Np[1-p])/ (d2/Z21-α/2*[N-1]+p*[1-p])
Population size (for finite population correction factor or fpc) (N): 1000
Hypothesised % frequency of outcome factor in the population (p): 17.7%±5
Confidence limits as % of 100 (absolute ± %) (d): 6%
Design effect (for cluster surveys-DEFF):
Sample size comes out to be 135, considering 10%, non-response rate
Final sample size would be 150
The data so generated in the form of an Excel spreadsheet from Google Forms were analysed using Microsoft Excel 7 and Epi Info 7 software by CDC.
RESULTS
The demographic characteristics of the participants were as follows: The majority of them were below 45 years of age with a mean (SD) of 44.2 (6.9) years and just 3% were of age 60 years and above. Male constituted 60% and the majority of them are postgraduate and married. Almost 42% of them suffered from one or more comorbidities. Most of them have more than 10 years of work experience with a mean (SD) of 16.3 (6.78) years in their field of specialty [Table 1].
| Variable | Frequency (n=157) | Percentage |
|---|---|---|
| Age | ||
| 25–45 | 101 | 64.33 |
| 46–60 | 51 | 32.48 |
| >60 | 5 | 3.18 |
| Gender | ||
| Male | 93 | 59.24 |
| Female | 64 | 40.76 |
| Education | ||
| Graduate | 33 | 21.02 |
| Post-graduate | 124 | 78.98 |
| Comorbidities | ||
| Present | 66 | 42.04 |
| Absent | 91 | 57.96 |
| Marital status | ||
| Married | 149 | 94.90 |
| Unmarried | 8 | 5.10 |
| Work experience | ||
| <10 years | 18 | 11.46 |
| 10–20 years | 89 | 56.69 |
| >20 years | 50 | 31.85 |
[Table 2 and Figures 1-4] show the mean score and percentage of the PSS-10 [Figure 1] and PHQ-4 among the study participants. The mean (SD) of PHQ among males and females was 3.39 (1.82) and 3.70 (3.034) and the PSS-10 score was 14.3 (3.6) and 15.9 (6.3), respectively. There was a statistically significant difference among the mean PHQ-4 and PSS scores of males and females, where females showed higher levels of anxiety, depression, and stress as compared to their male counterparts in total PSS and PHQ-4 and its subscale.
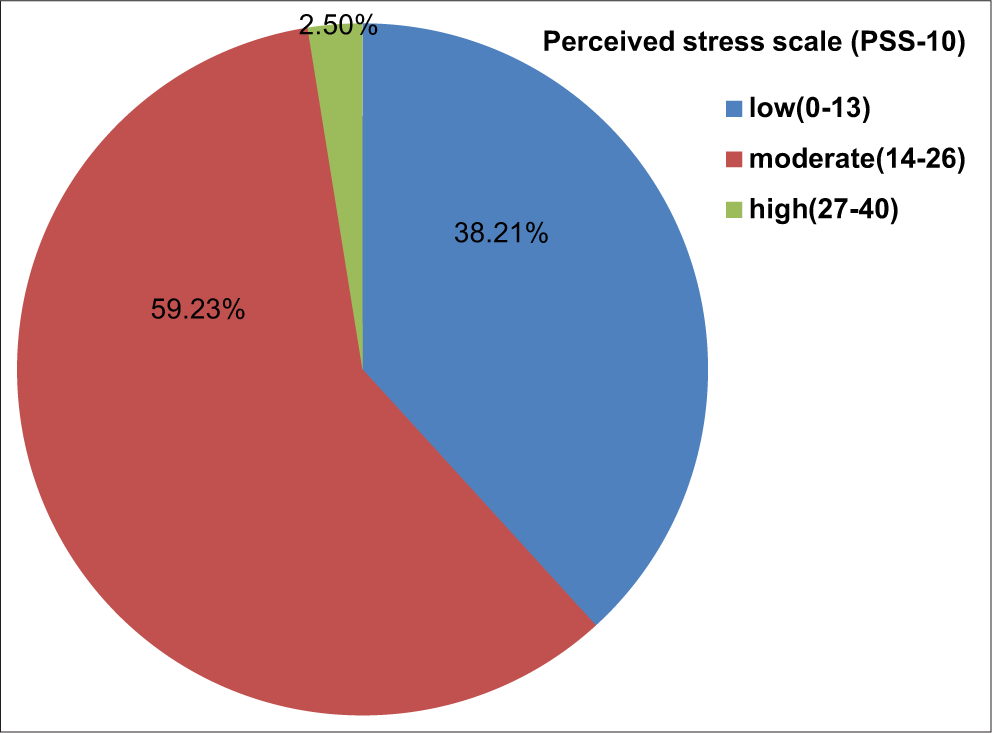
- Severity level of stress among private practitioners.
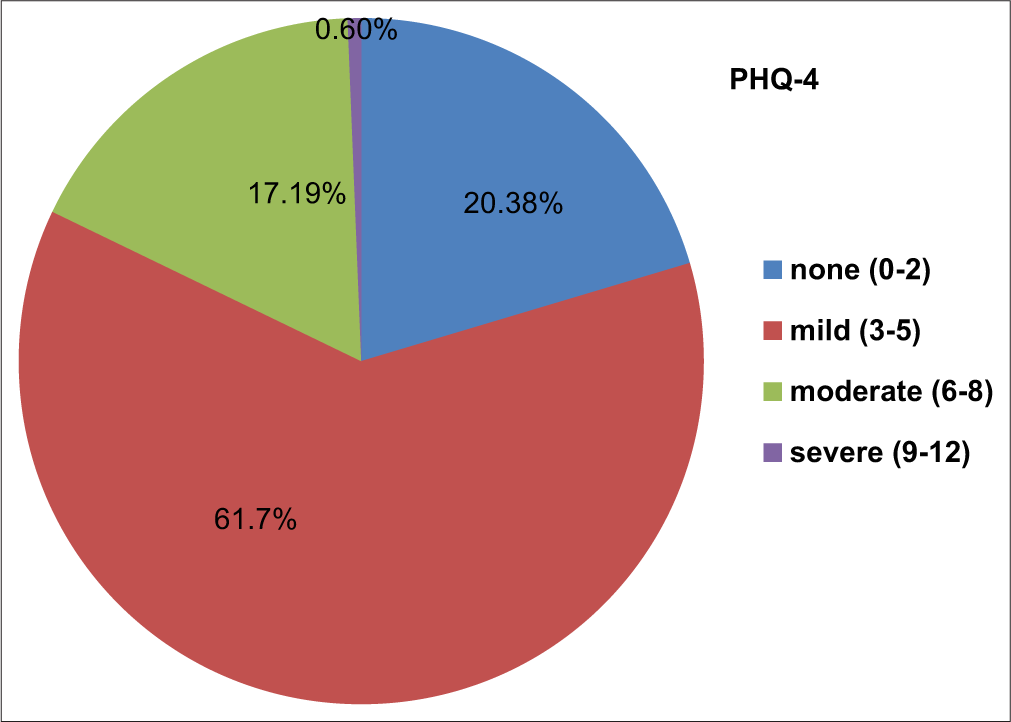
- Severity level of anxiety and depression among private practitioners on PHQ-4 scale.
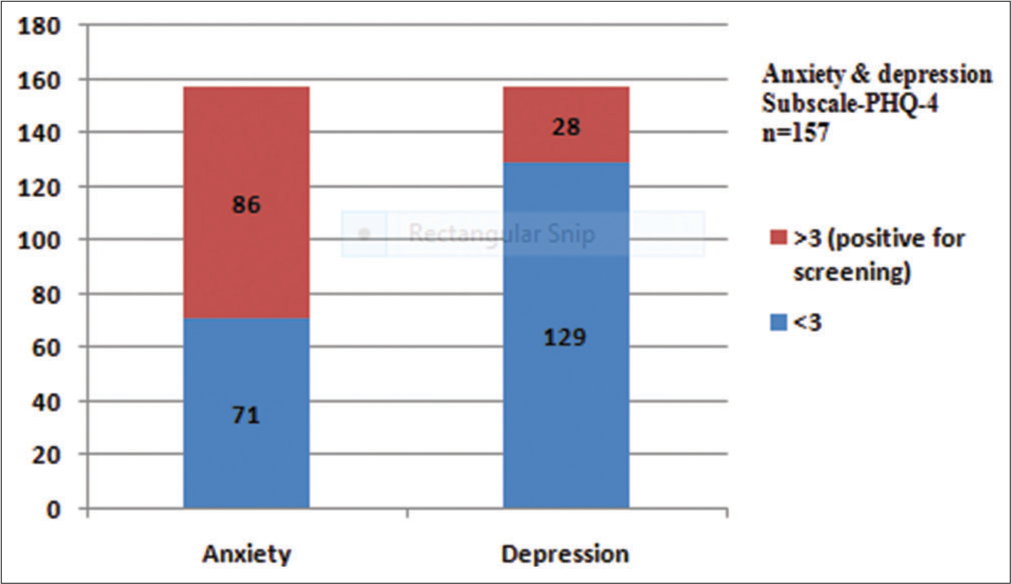
- Anxiety and depression among private practitioners (n=157).
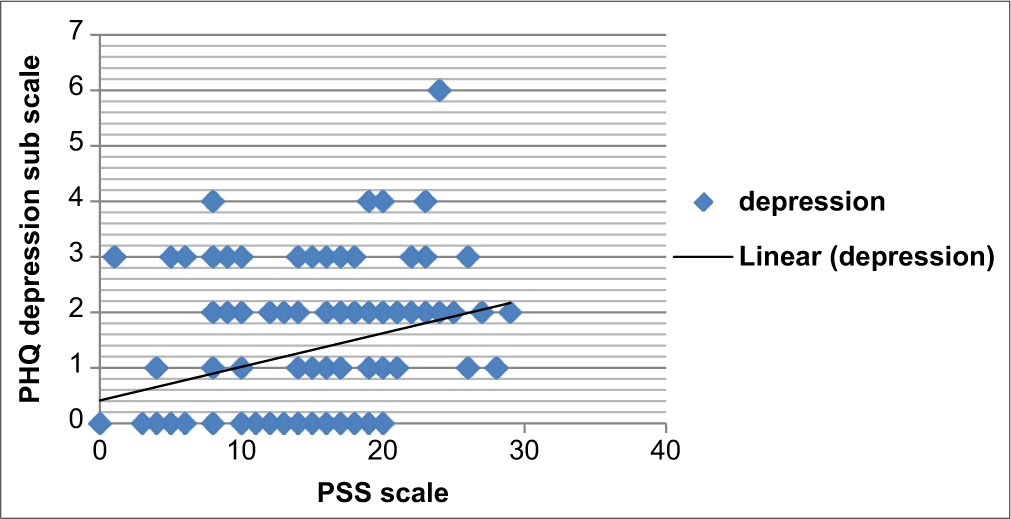
- Correlation between perceived stress and depression among private practitioners.
Overall 61.73% of participants have abnormal PSS-10 scores, and among them, 59.23% have moderate stress and 2.5% have high-stress levels.
| Anxiety and depression scores using PSS and PHQ | Mean±SD | P-value | |
|---|---|---|---|
| Male (93) | Female (64) | ||
| PHQ4 (total) | 3.39±1.822 | 3.7±3.034 | 0.000008329 |
| PHQ-Q1 (feeling nervous, anxious or on edge) | 0.543±0.747 | 0.578±0.708 | |
| PHQ-Q2 (not being able to stop or control worrying) | 1.806±1.227 | 1.56±1.193 | |
| PHQ-Q3 (little interest or pleasure in doing things) | 0.989±1.005 | 0.703±0.937 | |
| PHQ-Q4 (feeling down, depressed or hopeless) | 0.37±0.64 | 0.54±0.711 | |
| PHQ (anxiety and depression) | |||
| PHQ-Q1 and Q2 (anxiety) | 2.34±1.3 | 3.6±1.9 | 0.0008 |
| PHQ-Q3 and Q4 (depression) | 1.36+1.33 | 3.00±1.8 | 0.004 |
| PSS (total) | 14.34+3.6 | 15.93±6.3 | 0.04 |
PSS: Perceived Stress Scale, PHQ: Patient Health Questionnaire
PHQ-4 score was abnormal in 79.6% of the private practitioners, and among them, 61.5% have mild, 17.1% have moderate and 0.6% had severe abnormality in their scores [Figure 2].
The anxiety and depression subscales of the PHQ-4 scale showed that 54.7% of the private practitioners have anxiety subscale ≥3 and 18% have depression subscale >3 needing further psychiatric evaluation [Figure 3].
There was a positive correlation between the perceived stress and depression among the study participants with Pearson’s (r) value of 2.97 [Figure 4].
Univariate analysis of predictors of stress, anxiety, and depression among the study participants clearly depicted that female practitioners have higher stress, anxiety, and depression than male private practitioners, and it was found to be statistically significant in both scales of evaluation. Another significant predictor of perceived stress was the mode of consultation by private practitioners during the first wave of the COVID pandemic, it was seen that those practitioners who were using only telemedicine/telephonic medium for consultation have significantly less stress, anxiety, and depression than those who are providing services either indoor or outpatient (OPD). Private practitioners with more than 20 years of work experience and those who are aged 45 years or older have significantly less stress compared to those who have <20 years of experience and who are younger [Tables 3 and 4].
| Variables | Normal | Mild | Moderate | Severe | Total | P value |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Female | 15 | 20 | 20 | 9 | 64 | 0.00019 |
| Male | 17 | 57 | 18 | 1 | 93 | |
| Age | ||||||
| 25–45 | 24 | 59 | 18 | 0 | 101 | 0.264 |
| >45 | 8 | 38 | 9 | 1 | 55 | |
| Years of experience | ||||||
| <10 years | 5 | 9 | 4 | 0 | 18 | 0.692 |
| 10–20 years | 16 | 59 | 14 | 0 | 89 | |
| >20 years | 11 | 29 | 9 | 1 | 50 | |
| Comorbidities | ||||||
| Present | 18 | 39 | 8 | 1 | 66 | 0.504 |
| Absent | 14 | 58 | 19 | 0 | 91 | |
| Providing COVID care | ||||||
| Yes | 3 | 29 | 6 | 1 | 39 | 0.82 |
| No | 29 | 68 | 21 | 0 | 118 | |
| Modes of consultation | ||||||
| Only OPD | 10 | 34 | 17 | 1 | 62 | 0.0003 |
| Only telemedicine/telephonic | 9 | 11 | 2 | 0 | 22 | |
| Inpatient only | 11 | 13 | 25 | 1 | 49 | |
| Both OPD/inpatient | 2 | 6 | 15 | 2 | 25 | |
| Education | ||||||
| Graduate | 7 | 18 | 8 | 0 | 33 | 0.631 |
| Post-graduate | 25 | 79 | 19 | 1 | 124 |
P-value of <0.05 is significant for gender and modes of consulation
| Variables | Low | Moderate | High | Total | P-value |
|---|---|---|---|---|---|
| Gender* | |||||
| Female | 22 | 30 | 12 | 64 | 0.001608 |
| Male | 38 | 53 | 2 | 93 | |
| Age* | |||||
| 25–45 | 32 | 67 | 2 | 101 | 0.0164 |
| >45 | 28 | 27 | 1 | 56 | |
| Years of experience** | |||||
| <10 years | 6 | 11 | 2 | 19 | 0.00863 |
| 10–20 years | 28 | 60 | 0 | 88 | |
| >20 years | 26 | 22 | 2 | 50 | |
| Comorbidities* | |||||
| Present | 24 | 40 | 2 | 66 | 0.724 |
| Absent | 36 | 53 | 2 | 91 | |
| Providing COVID care* | |||||
| Yes | 18 | 20 | 2 | 40 | 0.56 |
| No | 42 | 73 | 2 | 117 | |
| Modes of consultation** | 0.521 | ||||
| Only OPD | 40 | 20 | 1 | 61 | 0.00001 |
| Only telemedicine/telephonic | 20 | 2 | 0 | 22 | |
| Inpatient only | 16 | 32 | 2 | 49 | |
| Both OPD/inpatient | 7 | 16 | 2 | 25 | |
| Education* | 0.262 | ||||
| Graduate | 17 | 16 | 0 | 33 | |
| Post-graduate | 43 | 77 | 4 | 124 |
*Mann–Whitney U-test, ** Kruskal–Wallis test, P value of <0.05 is significant for Gender, age, years of experience and mode of consultation
In the present study, 70% of the participants get relaxed by talking with their family and friends, more than 50% used online entertainment and physical fitness for relaxation and just 5.7 used alcohol, and 3.8% used antianxiety/ antidepressant drugs [Table 5].
| Modes | Number | % |
|---|---|---|
| Meditation and yoga | 20 | 12.7 |
| Physical fitness | 80 | 51.0 |
| Talking with friends and family | 109 | 69.4 |
| Alcohol | 9 | 5.7 |
| Online entertainment | 87 | 55.4 |
| Antianxiety/antidepressant drugs | 6 | 3.8 |
| Religious support and prayers | 19 | 12.1 |
| Unable to relax | 5 | 3.2 |
DISCUSSION
The prevalence of mental morbidity in our study is reflected by moderate-to-high stress in 61% and anxiety and depression levels requiring further evaluation in 54.7% and 17.8% of the private practitioners, respectively. In a study done by Wen et al. in China, moderate-to-severe anxiety and depression were reported in 22.6% and 11.8% of the HCWs, respectively.[2] A study done in Wuhan, China, by Zhu et al. reported the prevalence rates of stress, depression, and anxiety of 29.8%, 13.5%, and 24.1%, respectively.[5] Another study done in Karnataka and India during the first wave of the COVID pandemic in 2020 reported the prevalence of anxiety and depression of 11.4% and 17.7% among HCWs, respectively.[1] A higher level of anxiety and stress in our study was due to the fact that more than 50% of private practitioners were also worried about the loss of their OPDs due to lockdowns, shortage of staff to run the private clinics due to unwillingness of staff to work in COVID isolation wards and also due to scarcity of PPE kits; however, depression was less severe in our study as more than 50% of private practitioners were providing health services through only outpatient (OPD) and telemedicine/telephonic modes. Findings similar to our study, with the anxiety of 56.65% and depression of 32% among physicians, were reported in the study done by Raj et al. during the lockdown period of the first wave.[6] A multinational study in Singapore has reported lower levels of severe depression (5.3%), moderate-to-severe anxiety (8.7%), and moderate-to-severe stress (2.2%) in the HCWs.[7]
In our study, the majority of the doctors were concerned about the spread of infection to their family members and were also worried due to decreased patient OPDs, shortage of staff, and PPE kits, similar to HCPs in other parts of the world.[8,9]
Risk factor analysis in our study showed that women private practitioners were having a greater degree of anxiety, depression, and stress than their male counterparts and were statistically significant, a similar finding was seen in the study done by Lai et al., where women were at increased odds of developing anxiety and depression.[10] Another study done in the USA by Aiyer et al. has concordance with our study findings.[11] Wilson et al. also reported a similar findings in their study.[1] There was a positive correlation between stress and depression in our study, which showed a positive Pearson’s correlation (R) of 2.97, similar to the finding of a study done in the USA where R-value was even higher at 0.7.[11]
In our study, doctors aged <45 years suffered higher depression than those who were more than 45 years of age, similar findings were seen in the study done in China by Liang et al. (2020) in their cross-sectional analysis done on 59 doctors and nursing staff posted on COVID-19 duty in Guangdong Province in China using self-rating anxiety and depression scales reported that the most of the staffs suffered from clinical symptoms of depression. This study presented findings that medical doctors aged <30 years suffered from higher depression scores when compared to doctors who are aged more than 30 years.[12] A recent study was done in Trinidad and Tobago by Nayak et al. who showed that HCWs were younger exhibited higher stress levels.[13]
Another positive predictor of anxiety and stress in our study was years of experience where more experience doctors with over 20 years of practice have less anxiety and stress than their younger counterparts, this finding was supported by the study done in Sudan by Mahgoub et al. who reported a highly significant correlation between stress levels and years of experience with R-value of −0.137[14]; however, this was a negative predictor in the study done by Wilson et al.[1] In our study, the majority of doctors relieve their stress by talking with their friends and family members, online entertainment, and physical fitness; similar findings were reported by the study done in Karnataka.[1] However, studies done in Sudan and Oman reported that the majority of HCWs turn to religion and prayer as the most common coping mechanism against stress.[14,15]
There are a few limitations of our study, first, it was an online survey of the participants and it is not possible to make a diagnosis of the participants who were screened positive in the survey, so the exact prevalence of mental morbidity cannot be predicted and will vary, but the use of standardised tools in the study would give close estimates. Another limitation is that the study was done only among private practitioners who used various modes of consultation which include on line and telephonic consultation and so study results cannot be reflective of those public HCWs who are working is high patient load, in inpatient government COVID healthcare facilities that cater to the maximum patient load in the first wave of COVID pandemic.
This study did not control factors such as comorbidities, preexisting anxiety, depression, and alcohol intake that might have influenced the anxiety, stress, and depression scores. The study was done only during a pandemic and not before, so it’s difficult to say whether these psychological factors are due to the pandemic or pre-existing.
CONCLUSION
The prevalence of mental morbidity in our study is reflected by moderate-to-high stress in the majority of HCP. More than half of them have anxiety and almost one-fourth of them have depression, requiring further evaluation. Since private practitioners still cater to 70% of the patients, particularly in urban settings in India, it is of utmost importance that a comprehensive and proactive strategy should be formulated both at the government level and also at individual institution levels to provide free counselling and screening sessions to cater to the psychological and mental health needs of healthcare providers so that quality of healthcare services provided by them can be maintained.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Prevalence and predictors of stress, anxiety, and depression among healthcare workers managing COVID-19 pandemic in India: A nationwide observational study. Indian J Psychol Med. 2020;42:353-8.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological status of medical workforce during the COVIS-19 pandemic: A cross-sectional study. Psychiatry Res. 2020;288:11236.
- [CrossRef] [PubMed] [Google Scholar]
- An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics. 2009;50:613-21.
- [CrossRef] [PubMed] [Google Scholar]
- A 4-item measure of depression and anxiety: Validation and standardization of the patient health questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122:86-95.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 in Wuhan: Immediate psychological impact on 5062 health workers. EClinicMedicine. 2020;24:100443.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological impact of the COVID-19 pandemic n healthcare workers in India: An observational study. J Family Med Prim Care. 2020;9:5921-6.
- [CrossRef] [PubMed] [Google Scholar]
- A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559-65.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med Sci Monit. 2020;26:e924171.
- [CrossRef] [Google Scholar]
- Critical supply shortages the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382:e41.
- [CrossRef] [PubMed] [Google Scholar]
- Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976.
- [CrossRef] [PubMed] [Google Scholar]
- Mental health impact of COVID-19 on healthcare workers in the USA: A cross-sectional web-based survey. J Depress Anxiety. 2020;9:373.
- [Google Scholar]
- Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID19. J Psychosom Res. 2020;133:11012.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and factors associated with depression, anxiety and stress among healthcare workers of Trinidad and Tobago during COVID-19 pandemic: A cross-sectional study. BMJ Open. 2021;11:e044397.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological effects of the COVID-19 pandemic: Perceived stress, anxiety, work-family imbalance, and coping strategies among health care professionals in Khartoum state hospitals, Sudan, 2021. Brain Behav. 2021;11:e2318.
- [CrossRef] [PubMed] [Google Scholar]
- The mental health of health care workers in Oman during the COVID-19 pandemic. Int J Soc Psychiatry. 2021;67:90-5.
- [CrossRef] [PubMed] [Google Scholar]






