Translate this page into:
A cross-sectional survey to assess the drug disposal practices of unused and expired medicines among lay public visiting a tertiary care hospital in an urban metropolis
*Corresponding author: Renuka Munshi, Department of Clinical Pharmacology, Topiwala National Medical College and BYL Nair Charitable Hospital, Mumbai, Maharashtra, India. renuka.munshi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Munshi R, Dhiman A, Maurya M. A cross-sectional survey to assess the drug disposal practices of unused and expired medicines among lay public visiting a tertiary care hospital in an urban metropolis. Indian J Physiol Pharmacol 2023;67:29-35.
Abstract
Objectives:
A cross-sectional survey was conducted to evaluate the knowledge, awareness and practice among the lay public regarding storage and disposal of unused and expired medicines.
Materials and Methods:
This was an observational, cross-sectional, single-centre and questionnaire-based survey. After obtaining Institutional Ethics Committee approval, the study was conducted using a pre-validated structured questionnaire distributed among the lay public visiting a tertiary care hospital located in an urban metropolitan city.
Results:
Four hundred of 720 individuals visiting the tertiary care hospital participated in the survey. The results revealed that 75% had never referred to any sources to get the correct information about the proper and safe disposal of medicines and had no knowledge regarding the same. About 12.75% of study participants reported that they were educated regarding the disposal of medicines by their treating physicians (RR: 0.71 [95% CI: 0.51–0.99]) when compared with the other sources of information (18%) with statistically significant contribution made by the physicians (p<0.05). About 67% of the public stored their medicines at room temperature. Majority (83.75%) of the study participants reported that they disposed unused and expired drugs in the dustbin. Only 42.5% of the public knew the detrimental effect of improper drug disposal on human health and our ecosystem. In addition, 80% (320/400) of the participants confirmed that, given the option, they would prefer to return the unused or expired drugs to the pharmacy shops from where the medicines were purchased.
Conclusion:
There is a need to educate drug consumers/general public about safe and proper disposal of unused/ expired medicines. Health-care professionals, governments and policymakers should offer training to educate the general public about Indian regulations for safe disposal of unused/expired medicines.
Keywords
Drug disposal
Expired drugs
Ecosystem
Adverse effects
Public health
INTRODUCTION
The worldwide drug consumption by consumers for the prevention and treatment of medical conditions is increasing daily, and so there is increase in the global spending on medicines. As per data in year 2020, approximately 1.27 trillion U.S. dollars has been spent on medicines and this number is expected to increase to 1.6 trillion by the year 2025.[1] Moreover, according to the World Health Organization (WHO), 50% of patients fail to take their medicines correctly resulting in unnecessary stocking of expired or unused medicines.[2] Patients may not take all the medications as prescribed to them for various reasons, namely experiencing adverse effects in the past, when the dose is increased, feeling better earlier than the number of days the medicine has been prescribed, proximity to the expiry date, and advice by friends and family.[3,4] Thus, it is very common for patients to have unused or expired medicines at their homes that are often not disposed off. These unused and expired medicines if disposed inappropriately may expose the humans, environment and ecological species at risk.[5,6] The lack of awareness about the safe drug disposal practices for unused and expired medicines results in consumers often keeping these drugs beyond the expiry date, giving them to friends and family, rinsing the medicines down the sink or flushing them in the toilet or discarding the medicines in the trash.[3] Very few pharmacies take back expired medications from patients to dispose of them properly. Most of the drug consumers remain unaware of the proper disposal of unused or expired drugs which may disrupt our ecological balance. For instance, vultures exposed to disposed unused or expired non-steroidal anti-inflammatory drugs like diclofenac are at increased risk of renal failure and mortality that can lead to the extinction of these vulture species in South-east Asia.[7] European water fishes exposed to trace levels of Ethinyl estradiol, a component of oral contraceptive pills, have been found to affect the sexual development and feminization process in these fishes.[8] Expired drugs may lose their efficacy and may pose safety and health concerns due to formation of toxic metabolites. Hence, a strict compliance with appropriate drug disposal practices for unused/expired drugs is required.[9] The storage of unused or expired medications may also change their physicochemical properties and unwanted toxic metabolites may be formed, also associated with increased risk of microbial contamination.[10] The inappropriate disposal of medicines in the waterways and drinking water has also gained national and international attention from the public, lawmakers and regulators due to health concerns.[11] The WHO recommends various disposal methods such as incineration, waste encapsulation, inertisation, landfill, sewer, fast-flowing watercourse, burning in open containers and return to donor or manufacturer and transfer for disposal.[12,13] The need of the hour is to minimise the expenses incurred for disposal of waste pharmaceuticals which can be achieved by sorting various pharmaceutical products and following their disposal methods accordingly. There is a need to create awareness about the existing standard guidelines for the disposal of medicines and emphasise its implementation among the public consumers. With this background, we conducted a cross-sectional survey to assess the knowledge and disposal practices followed by general public who consume medicines.
Study objectives
The objectives of the study are as follows:
To assess the knowledge and understanding of the lay public regarding sources of information for disposal of medicines.
To assess the practice regarding storage and disposal of medicines among the lay public.
MATERIALS AND METHODS
Ethical considerations
The study was commenced after obtaining the approval from the Ethics Committee for Academic Research Projects (ECARP) of our institute (ECARP/89/2018). The study was conducted in accordance with the principles of Good Clinical Practice that has its principle in the Declaration of Helsinki (1964) and Indian Council of Medical Research - National Ethical Guidelines for Biomedical and Health Research Involving Human Participants (2017).
Study design
The study was a cross-sectional and questionnaire-based survey conducted at our tertiary care public hospital located in an urban metropolitan city. The study was conducted over 3 months from August 2018 to October 2018. We included a total of 400 consenting individuals of either gender and above the age of 18 years. The study participants were patients and their relatives visiting our tertiary care hospital in Mumbai, India, that mainly comprised people residing in the vicinity of the hospital.
Validation of the questionnaire
The 20-item questionnaire was evaluated by eight subject experts for its content and relevance to our study objectives. The experts graded each question as ‘very essential’, ‘essential’ or ‘not useful’ with feedback on modifying the questions if not correctly framed or if some important question was missing. Based on their response, the content validity ratio (CVR) was calculated. Only those questions with a content validity score ≥0.75 were incorporated into the questionnaire. The cutoff CVR score was decided based on number of experts agreeing to the questions and total number of expert members.[14]
Sample size calculation
Sample size was calculated using the formula, N=4PQ/d2, where, P=Prevalence, Q=100-P, d= error. The lack of awareness about the drug disposal practices was about 70% in a previous study by Rogowska et al.[15] Assuming precision of 5%, the sample size (n) was estimated to be 336. Adjusting for the 20% dropout rate, the corrected sample size (n) was estimated to be 400.
Study procedure
The structured questionnaire survey tool was validated before its use in the study participants. Individuals who consented to participate in the survey were asked to fill out the questionnaire in the preferred language of their choice after explaining the importance of the study. The validated questionnaire had few questions on their demographic characteristics such as number of members in their family, socioeconomic status using the Kuppuswamy scale, family members suffering from chronic and acute diseases and the system of medicine they followed for the treatment. Few other questions included the types of medicine dosage forms they have been using, storage conditions for the medicines they take and finally about the disposal methods practiced by the study participants.
Statistical analysis
The data collected from study participants were analysed using descriptive statistics expressed as proportions and percentages. Few of the categorical responses were evaluated using Chi-square test at 5% significance level.
RESULTS
We distributed the questionnaire among 720 individuals from the general public of whom 320 either did not respond or returned an incompletely filled questionnaire, thus giving a response rate of almost 80%. Filled questionnaires received from 400 participants who responded were considered for final analysis.
Demographics
Demographic characteristics are tabulated [Table 1] which include gender, median age, educational status and modified Kuppuswamy scale updated for year 2020[16] distribution among the enrolled study participants (N=400). Furthermore, the proportion of study participants with the nature of their illness [Figure 1] and the formulations of medicines used [Figure 2] are demonstrated in the figures. Almost 61.3% of the study participants preferred allopathic system of medicine for treatment followed by Ayurveda (59%) and Homoeopathy (25%). In addition, 56% of the study participants preferred to take both ayurvedic and allopathic medications, 10% preferred allopathy and homeopathic medicines and only 2% preferred taking ayurvedic and homeopathic medicines for treatment of their illness. Only 3% of study participants agreed to have taken or preferred to opt for medicines from allopathic as well as alternative systems of medicines.
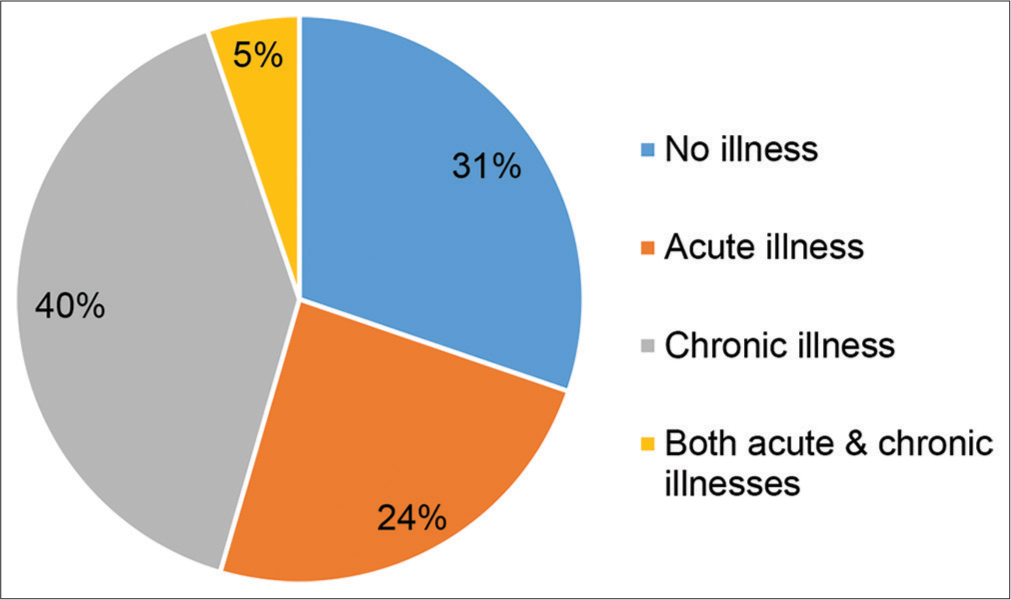
- Distribution of study participants suffering from illnesses (N=400).
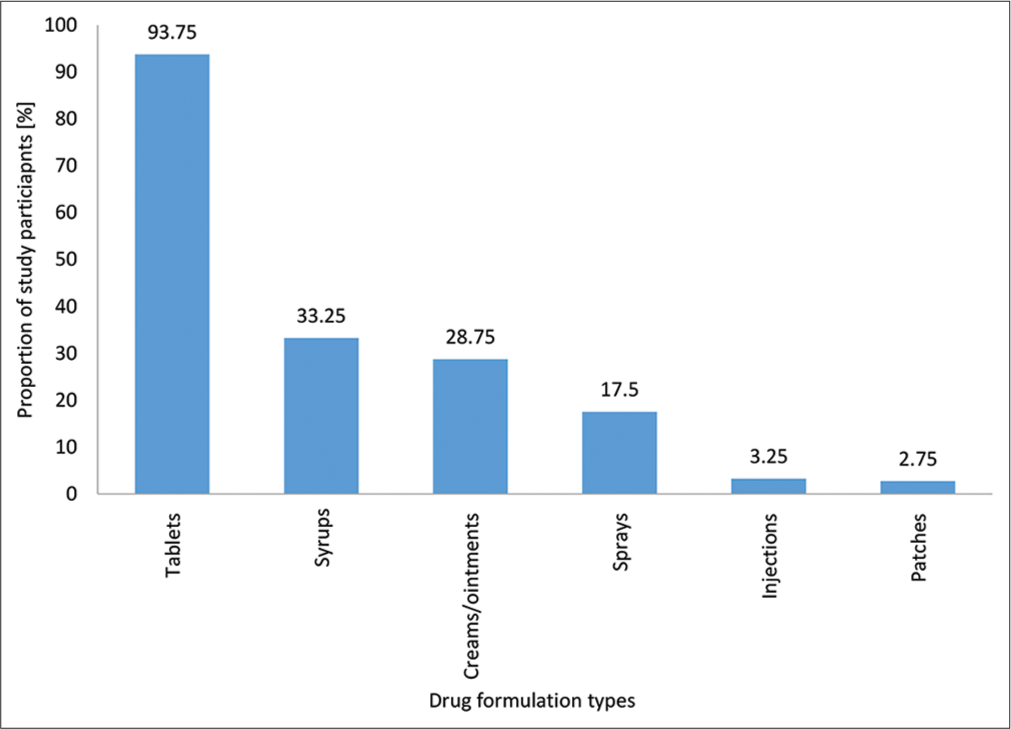
- Different medicine dosage forms used by the study participants at home.
| Demographic characteristics | Proportion of participants n (%) |
|---|---|
| Gender | |
| Males | 253 (63.25) |
| Females | 147 (36.75) |
| Median age in years with range | |
| Males | 35 (18–78) |
| Females | 38 (18–70) |
| Education status | |
| Illiterates | 73 (18.25) |
| 10th-grade pass | 107 (26.75) |
| 12th-grade pass | 73 (18.25) |
| Graduate | 134 (33.5) |
| Postgraduate | 13 (3.25) |
| Kuppuswamy Scale (for socioeconomic status) | |
| I | 37 (9.25) |
| II | 147 (36.75) |
| III | 154 (38.5) |
| IV | 58 (14.5) |
| V | 4 (1) |
| Total number of family members (Median with range) | 5 (2–22) |
| Proportion of participants prescribed antibiotics in past 6 months (%) | 103 (25.75) |
| How frequently the medicines are disposed of at home – Number of study participant responses (%) |
Once a week – 41 (10.2) Once a month – 99 (24.75) Once in 3 months - 46 (11.5) Once in 6 months - 88 (22) Once in a year - 82 (20.5) As soon medicine dose is finished - 45 (11.25) |
Assessment of participant understanding of the sources of information for proper disposal of medicines
About 31.5% (126/400) of the study participants accepted that they frequently used common medicines such as paracetamol, cetirizine and other painkillers on their own without prescriptions from the physicians (self-medication practice). The sources of information regarding disposal of medicines referred to by the study participants are described in detail [Figure 3]. About 12.75% of study participants reported that they were educated regarding the safe disposal of medicines by their treating physicians (Relative Risk (RR): 0.71 [p<0.05, 95% Confidence Interval: 0.51-0.99]) as compared with the other sources of information (18%) and this contribution by the physicians was found to be statistically significant.
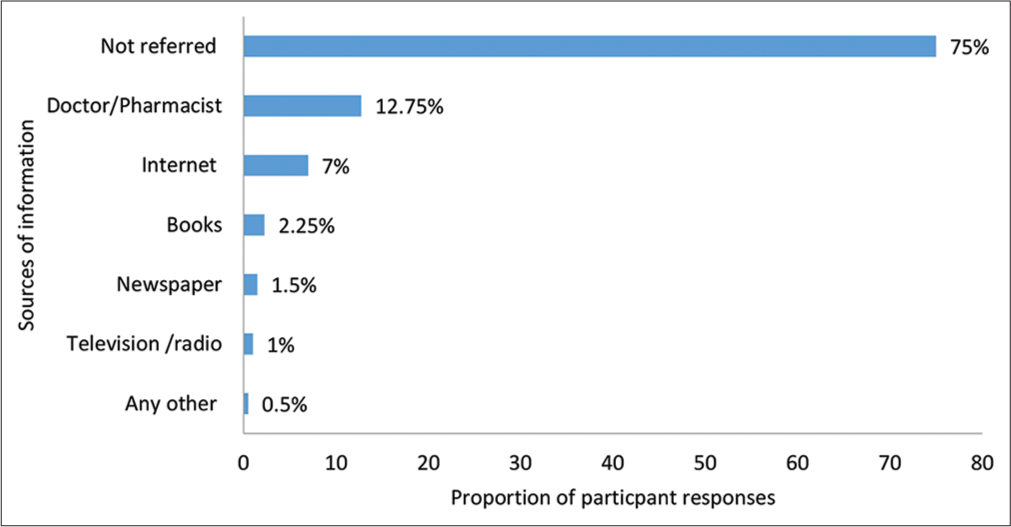
- Sources of information among lay public regarding the disposal of medicines (N=400).
Assessment of participants’ practice about the storage and disposal of medicines
When questioned about their knowledge regarding storage of medicines, 67% (263/400) of the participants reported that they stored medicines at room temperature, 8.5% (34/400) reported that they kept medicines in the refrigerator, 13% (52/400) said that they kept medicines away from the direct sunlight, 7% (28/400) responded that they kept the medicines at room temperature and/or refrigerator while only 0.25% (9/400) responded that they kept the medicines away from exposure to direct sunlight and at room temperature. About handling of spare or expired drugs, 10.3% (41/400) of the study participants said that they dissolved the drugs in water and then discarded the dissolved solution in the sink, 83.75% (335/400) of the participants agreed that they threw the drugs in the dustbin, 2.75% (11/400) flushed the expired drugs in the toilet, 2.75% (11/400) said that they buried the expired drugs in the ground while 0.5% (2/400) practised any one of the above methods to dispose of medicines. When enquired regarding when the medicines were disposed off, the responses received were either following damage (31.25%), on expiry of medicines (68.5%) and immediately after completion of the treatment schedule (11.5%), respectively. When asked about their knowledge regarding antibiotic resistance, only 24.75% (99/400) participants were aware of the concept or had heard of this term. About 42.5% (170/400) of the study participants were aware of the hazards due to improper disposal of medicines while 320/400 (80%) of the study participants said that they would prefer to return the expired medicines to the pharmacy shop from where they had purchased the medicines.
DISCUSSION
Unsafe disposal of unused or expired medicines causes significant environmental hazards and contributes to potential risk of antimicrobial resistance. Our cross-sectional and questionnaire-based survey (N=400) conducted at a tertiary care hospital located in an urban metropolitan city revealed that majority (75%) of public lacked knowledge and awareness regarding the correct information for proper and safe disposal of medicines while only few (12.75%) were educated regarding the same by their treating physicians. Hence, there is a need to conduct public awareness campaigns/programmes for health-care professionals regarding safe disposal of medicines. About 24.8% of the participants/lay public were aware of the term/concept of ‘antibiotic resistance’ while 80% of the participants said that they would prefer to return unused or expiry drugs to the pharmacy which is positive indicator of public adherence to any policies related to safe disposal of medicines. An online literature search of 12 peer-reviewed articles by Tong et al. revealed that the most common method practiced for drug disposal were garbage, toilet or sink. These liquid medicines were rinsed down the sink while the solid tablets/capsules were disposed off in the dust bins.[17] A cross-sectional and questionnaire-based study conducted by AlAzmi et al. to evaluate the patients’ knowledge and attitude towards the disposal of medications in the city of Jeddah, Saudi Arabia, revealed that 73% of the study participants discarded their medications in the trash, 14% preferred to return the medications to a pharmacy, 5% never disposed them and 3% donated the medicines to friends or charity centres. Almost 80% accepted about not receiving any information/advice regarding the safe and proper disposal of medications from healthcare professionals.[18] A cross-sectional survey (N=497) by Alfian et al. from Bandung city, Indonesia also revealed that almost 53% of the study participants were not aware of the fact that improper medication disposal could harm our ecosystem. In addition, 79.5% agreed to fact that they had never received information about proper medication disposal practices.[19] A similar study by Marwa et al. assessed the disposal practice of expired and unused medications at household level among Tanzania population (N=359). The results revealed that 96% kept unused/expired medications in their homes which were supposed to be discarded and disposing of medications practice followed were domestic trashes (75.5%) and pit latrines (15.5%) with 76% aware of the detrimental effect of improper disposal of expired medications to human health and environment.[20] A cross-sectional survey with face-to-face interviews conducted by Bashaar et al. revealed that 83.4% of the interviewees purchased prescription-based medicines while 14.6% purchased medicine over the counter. Majority (95.3%) of the respondents stored medicines at home. About 77.7% of the respondents discarded the expired medicines in household trash. Almost 98% felt that improper disposal of unused and expired medicines can affect the environment and health.[21] A 4-month web-based questionnaire survey by Wajid et al. among adults (N=337) residing in Saudi Arabia revealed the practice of keeping unused medicine as 89.3%. About 65% of participants kept the medicines until they expired; 48.1% threw them away in the household garbage while only 5.4% of the respondents returned the unused/expired medicines to a medical store.[22] Zalpuri et al. study also highlighted that the most common practice of medicines disposal is discarding in the household garbage with only 24.2% being aware of drug take-back system.[23] Manocha et al. in their study from the National Capital Region, New Delhi, showed that 93% of the drug consumers were in favour of a government programme to collect unused and expired medicines from home.[24]
The U.S. FDA provides drug consumers with updates regarding ways as to where and how to dispose of unused medicines. The correct method to dispose of unused/expired drugs (prescription or overt-the-counter drugs) is to return them to the government authorised drug take-back collection sites which may be retail, clinical pharmacy, hospital or at the law enforcement drug collecting facility. If there are no drug take-back sites near the residential locality, then the lay public can either dispose of them in household trash or flush them down the toilet if it is mentioned in the U.S. FDA flush list of drug disposal. Flush in toilet method is mainly for potentially abusive drugs such as opioid and non-opioid-containing drugs. Those to be discarded in household trash need to be first mixed with some unpalatable substance such as dirt/ cat litter/used coffee grounds, placed in a sealed container/ bag after removing all personal details to make it unreadable before throwing the container in the household trash.[25,26] The study participants were educated individually regarding the right methods of safe disposal of medicines following receipt of their questionnaires which gave us an insight into the current practices that they followed. A review article by Kinrys et al. and Mani A et al. has described the negative impact of improper drug disposal on the environment and public health using water contaminated with trace pharmaceuticals highlighting the importance of patient and clinician education about the safe medication disposal methods.[27,28] Anwar et al. reviewed how the improper disposal of unused antibiotics may contribute to the issue of antimicrobial resistance.[29] Barbhuiya NH et al. assessed the antimicrobial ciprofloxacin and ofloxacin levels in waste water, surface water and groundwater in West Bengal region of India and estimated 69 times and 12 times resistance in Escherichia coli and Staphylococcus aureus, respectively, which is a serious health-care concern.[30] Velpandian et al. quantified 28 drugs from surface water and aquifers collected from 48 places (within 40 km) in New Delhi, India, which revealed above permissible limits of active pharmaceutical compounds and antimicrobials in aquifers (>0.1 mcg/L) raising serious concerns about antimicrobial resistance and environmental hazards.[31] Arun et al. also raised similar safety concerns as they could detect significant levels of sulphamethazine and fluoroquinolones in ground water influents from sewage treatment plants in Chennai, India, while tetracyclines and phenols were below detection levels.[32]
However, our study had its limitations, namely our survey focused more on the drug disposal methods for medicines in general and we did not differentiate between allopathic, ayurvedic and homoeopathic medicines. Moreover, the study results reflect the knowledge and perceptions of general public residing in Mumbai, India, and may not be generalisable to the overall Indian population.
CONCLUSION
Our study sheds light on the current practices of disposal of unused/expired medicines among the general population. The general population was unaware of the hazards of current medicine disposing methods practised by them and there is an urgent need to create awareness among general public regarding the same. The health-care system and the professionals involved need to play an important role in educating the general population regarding safe drug disposal practices. It is also recommended that the government and the policy makers should take a positive step towards initiating and successfully executing drug take-back programmes. Increasing awareness through educational programs about proper drug disposal practices and drafting guidelines for the same is required to prevent future health risks and environmental hazards.
Ethics statement
The Ethics Committee approval was accorded for this study [ECARP/89/2018].
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Global Medicine spending and usage trends: Outlook to 2025 (2021) IQVIA. The IQVIA Institute. Available from: https://www.iqvia.com/insights/the-iqvia-institute/reports/global-medicine-spending-and-usage-trends-outlook-to-2025 [Last accessed on 2022 Dec 08]
- [Google Scholar]
- World Health Organization. Available from: https://www.who.int/activities/promoting-rational-use-ofmedicines#:~:text=Irrational%20use%20of%20medicines%20is,fail%20to%20take%20them%20correctly [Last accessed on 2022 Dec 08]
- [Google Scholar]
- Patient practices and beliefs concerning disposal of medications. J Am Board Fam Med. 2006;19:542-7.
- [CrossRef] [PubMed] [Google Scholar]
- Beyond the medicine cabinet: An analysis of where and why medications accumulate. Environ Int. 2008;34:1157-69.
- [CrossRef] [PubMed] [Google Scholar]
- Risks related to the discharge of pharmaceuticals in the environment: Further research is needed In: Kümmerer K, ed. Pharmaceuticals in the Environment. Berlin, Heidelberg: Springer; 2004. p. :431-7.
- [CrossRef] [Google Scholar]
- Disposal of pharmaceutical waste in households-a European survey In: Kümmerer K, Hempel M, eds. Green and Sustainable Pharmacy. Berlin, Heidelberg: Springer; 2010. p. :165-78.
- [CrossRef] [Google Scholar]
- Diclofenac residues as the cause of vulture population decline in Pakistan. Nature. 2004;427:630-3.
- [CrossRef] [PubMed] [Google Scholar]
- Predicted exposures to steroid estrogens in U.K. rivers correlate with widespread sexual disruption in wild fish populations. Environ Health Perspect. 2006;114(Suppl 1):32-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of bacteriostatic potency of expired oral paediatric antibiotics and implications on infant health. Pan Afr Med J. 2014;19:378.
- [CrossRef] [PubMed] [Google Scholar]
- Unnecessary medicines stored in homes of patients at risk of medication misadventure. J Pharm Pract. 2006;36:16-20.
- [CrossRef] [Google Scholar]
- Dosed Without Prescription: Preventing Pharmaceutical Contamination of Our Nation's Drinking Water United States: Nature Resources Defense Council White Paper; 2009. p. :1-60.
- [Google Scholar]
- Guidelines for Safe Disposal of Unwanted Pharmaceuticals in and after Emergencies. 1999. Geneva: World Health Organization; Available from: https://www.who.int/water/sanitation/health/medicalwaste/unwantpharm.pdf [Last assessed on 2019 Jun 20]
- [Google Scholar]
- World Health Organization. Available from: https://www.who.int/substance_abuse/research_tools/translation/en [Last accessed on 2021 Jan 22]
- [Google Scholar]
- A quantitative approach to content validity. Pers Psychol. 1975;28:563-75.
- [CrossRef] [Google Scholar]
- Pharmaceutical household waste practices: Preliminary findings from a case study in Poland. Environ Manage. 2019;64:97-106.
- [CrossRef] [PubMed] [Google Scholar]
- Modified Kuppuswamy scale for socioeconomic status of the Indian family-update based on New CPI (IW) series from September 2020. J Family Med Prim Care. 2021;10:2048-9.
- [CrossRef] [PubMed] [Google Scholar]
- Disposal practices for unused medications around the world. Environ Int. 2011;37:292-8.
- [CrossRef] [PubMed] [Google Scholar]
- Patients' knowledge and attitude toward the disposal of medications. J Pharm (Cairo). 2017;2017:8516741.
- [CrossRef] [PubMed] [Google Scholar]
- Lack of awareness of the impact of improperly disposed of medications and associated factors: A cross-sectional survey in Indonesian households. Front Pharmacol. 2021;12:630434.
- [CrossRef] [PubMed] [Google Scholar]
- Disposal practices of expired and unused medications among households in Mwanza, Tanzania. PLoS One. 2021;16:e0246418.
- [CrossRef] [PubMed] [Google Scholar]
- Disposal practices of unused and expired pharmaceuticals among general public in Kabul. BMC Public Health. 2017;17:45.
- [CrossRef] [Google Scholar]
- Prevalence and practice of unused and expired medicine-a community-based study among Saudi adults in Riyadh, Saudi Arabia. Biomed Res Int. 2020;2020:6539251.
- [CrossRef] [PubMed] [Google Scholar]
- Disposal practices and awareness of medicine waste management among general population of Delhi-National Capital Region, India. J Appl Pharm Sci. 2022;12:78-83.
- [Google Scholar]
- Current disposal practices of unused and expired medicines among general public in Delhi and National Capital Region, India. Curr Drug Saf. 2020;15:13-9.
- [CrossRef] [PubMed] [Google Scholar]
- U.S. FDA-Where and How to Dispose of Unused Medicines. 2021. Available from: https://www.fda.gov/consumers/consumer-updates/where-and-how-dispose-unused-medicines [Last accessed on 2022 Feb 1]
- [Google Scholar]
- U.S. FDA-Disposal of Unused Medicines: What You Should Know. 2020. Available from: https://www.fda.gov/drugs/safe-disposal-medicines/disposal-unused-medicines-what-you-should-know [Last accessed on 2022 Feb 1]
- [Google Scholar]
- Medication disposal practices: Increasing patient and clinician education on safe methods. J Int Med Res. 2018;46:927-39.
- [CrossRef] [PubMed] [Google Scholar]
- The persisting environmental problem of disposal of expired and unused medicines. J Mahatma Gandhi Inst Med Sci. 2019;24:13-6.
- [CrossRef] [Google Scholar]
- Improper disposal of unused antibiotics: An often overlooked driver of antimicrobial resistance. Expert Rev Anti Infect Ther. 2020;18:697-9.
- [CrossRef] [PubMed] [Google Scholar]
- Determination of antimicrobial concentration and associated risk in water sources in West Bengal state of India. Environ Monit Assess. 2021;193:77.
- [CrossRef] [PubMed] [Google Scholar]
- Un-segregated waste disposal: An alarming threat of antimicrobials in surface and ground water sources in Delhi. Environ Sci Pollut Res Int. 2018;25:29518-28.
- [CrossRef] [PubMed] [Google Scholar]
- Antibiotics in sewage treatment plants, receiving water bodies and groundwater of Chennai city and the suburb, South India: Occurrence, removal efficiencies, and risk assessment. Sci Total Environ. 2022;851(Pt 2):158195.
- [CrossRef] [PubMed] [Google Scholar]







