Translate this page into:
Alleviating effect of Ficus racemosa in high-fat-high-fructose diet-induced non-alcoholic fatty liver disease
*Corresponding author: Nilay D. Solanki, Department of Pharmacology, Ramanbhai Patel College of Pharmacy, Charotar University of Science and Technology, Changa, Gujarat, India. nivyrx@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Solanki ND, Vadi K, Patel S. Alleviating effect of Ficus racemosa in high-fat-high-fructose diet-induced non-alcoholic fatty liver disease. Indian J Physiol Pharmacol 2021;65(1):12-20.
Abstract
Objectives:
Non-alcoholic fatty liver disease (NAFLD) is one of the chronic liver diseases. Ficus racemosa has been used for many years in the Ayurvedic medicine system and is closely related with the management of metabolic conditions. The study investigated alleviating effects of methanolic extract of F. racemosa (FRM) bark on high-fat-high-fructose (HFHF) diet -induced NAFLD.
Materials and Methods:
HFHF-based model was developed for a period of 10 weeks. In treatment groups, FRM (100 mg/kg, 200 mg/kg, and 400 mg/kg) and atorvastatin (20 mg/kg) were administered for 6 weeks after initiating HFHF diet and continued for another 4 weeks. Liver functions test, lipid profile, serum leptin, and antioxidant parameters and histopathology were evaluated.
Results:
Elevated liver enzymes, lipid markers, and leptin were observed, with significant reduction in antioxidants in disease control rats. FRM treatment significantly improved serum aminotransferase activities, lipid profile, and oxidative changes and brought back to normal. Liver histopathology showed the fatty modifications induced by the HFHF diet, and reduction in fatty changes was observed due to FRM. Significant decline in serum leptin was observed with high-dose FRM.
Conclusion:
FRM showed positive effects in the reversal of NAFLD and different polyphenolic compounds in the plant were responsible for the proven action.
Keywords
Non-alcoholic fatty liver disease
Ficus racemosa
High-fat-high-fructose diet
Aminotransferase
Serum leptin
Histopathology
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD) is a diverse hepatic state caused by irregular fat deposition in hepatocytes with or without inflammation. It embraces a range of liver diseases, include hepatic steatosis, steatohepatitis, fibrosis, cirrhosis, and liver failure.[1] As per the American Association for the Study of Liver Diseases guidelines, NAFLD is histological, which is categorized into two main categories such as fatty liver (simple steatosis) and steatohepatitis (NASH). The first one serves as a benign condition, whereas the development of this condition in the later stage has severe complications such as liver inflammation, hepatocellular injury, fibrosis, cirrhosis, and hepatocellular carcinoma (HCC).[2] NAFLD is associated with metabolic syndromes, such as obesity, type 2 diabetes mellitus (T2DM), hyperlipidemia, and hypertension. It is related to the highest rate of mortality as a consequence of the augmented risk of HCC and cardiovascular diseases.[3]
At present, NAFLD is one of the most popular chronic liver diseases, particularly in developed countries, with a prevalence of 25–30%, which is expected to increase due to unhealthy diet patterns rich in high-carbohydrates and high-fat foods. Intake of saturated fats and trans-fatty acids; lipogenic sugars such as fructose and sucrose and insulin resistance (IR) play a significant role in the pathogenesis of NAFLD.[4,5] NAFLD affects all ages and ethnicities. In the adult population, the prevalence of the disease ranges between 20 and 30% and rises up to 47%.[4,6] The prevalence of NAFLD is growing parallelly with the worldwide increase epidemic of obesity.[7]
Based on the available in vivo studies, the first mechanism based “two-hit” hypothesis for the pathogenesis of NAFLD was considered. As per this hypothesis, accumulations of fat droplets in hepatocytes act as the “first hit,” and further progression leads to activation of inflammatory cascades and development of fibrosis act as a “second hit.”[8] In the development and progression of human NAFLD, multiple parallel factors are involved, which increase the complexity of the disease. Therefore, currently the new “multiple mechanism hit” hypothesis has replaced older “Two-hit” prediction.[9] Accumulation of a high amount of lipids in the liver leads to lipotoxicity and chronic liver inflammation. A higher level of leptin hormone is also observed in patients with obesity and NAFLD, which is generally known as leptin resistance state. Therefore, it may have some role in the pathogenesis of NAFLD.[10]
Increased prevalence and negative pathological outcomes of NAFLD show a monumental economic burden for many countries. Still, up to now, no effective treatment is available for the disease.[11] Lifestyle changes serve as a cornerstone of management for NAFLD and obesity; however, only a couple of patients can achieve adequate weight loss and very few can maintain the body weight for the long term.[7] Today, other primary treatment approaches for NAFLD include anti-obesity drugs, lipid-lowering agents, insulin-sensitizing drugs, antioxidants, surgical interventions, and in the last stage liver injury and liver transplantation. Antidiabetic and hypolipidemic drugs, which improve IR and lower serum lipid level, significantly affect the disease and slow down the progression of symptoms.[12]
Pathogenesis of NAFLD is multifactorial; therefore, none of the monotargeted treatment approaches have provided satisfactory results and due to various side effects, these treatments are not tolerated by patients in the long term.[13] Traditional herbal medicines in various countries have provided a good source of natural substances for the management of chronic disorders, including metabolic syndrome, T2DM, gastrointestinal complications, and hyperlipidemia. At present, the number of researches, which focus on herbal extracts is increasing, and many of these researchers have discovered potent multi-targeted herbal products against NAFLD.[14] Hence, the multipronged therapeutic nature and safety of herbal medicine are essential for their use in treating NAFLD.
Ficus racemosa Linn. (Moraceae), commonly known as cluster Figure (gular), is an evergreen, medium to large-sized tree lacking primary aerial roots. It is widely distributed all over India, Australia (northern), and other parts of Asia.[15] All parts (leaves, fruits, bark, latex, and sap of the root) of this plant are considered medicinally important in mentioned in ancient scriptures of Ayurveda.[16] It has been used for 1000 years in Ayurvedic medicinal system for the treatment of jaundice, diabetes, dysentery, biliary disorders, diarrhea, and inflammatory conditions.[17] A broad range of chemical compounds were isolated from stem bark of this plant such as glycosides; sterols (β-sitosterol, stigmasterol, leucoanthocyanin, α-amyrin acetate, lupeol, and lupeol acetate); flavonoids (naringenin, quercetin, kaempferol, and baicalein); tannins (ellagic acid); and triterpenoids and gluanol acetate.[18,19] An extract of the bark of this plant possessed various pharmacological actions including hypolipidemic, antioxidant, anti-inflammatory, antidiarrheal, antibacterial, and antifungal and is closely related to prevention, treatment, and cure of obesity and diabetes.[20,21]
In some in vivo studies, it has been demonstrated that administration of high-fat-high-fructose diet (HFFD) causes IR, hepatic steatosis, and diminishes the inherent antioxidant defense system which results in excessive generation of reactive oxygen species (ROS) and fatty infiltration. This leads to a reduction of the hepatocyte populace and liver damage in rats.[22,23]
In the context of the information as mentioned above regarding the biological activities of F. racemosa bark, the present study has been performed to evaluate the effect of F. racemosa bark extract in the NAFLD animal model induced by administration of HFHF diet
MATERİALS AND METHODS
Drug and chemicals
Fructose, cholesterol, petroleum ether (60–80°C), and methanol were purchased from Loba Chemie (Mumbai, India). Casein was purchased from Charotar casein company, Nadiad (Gujarat, India). All chemicals and reagent used were AR grade. Vegetable ghee was purchased from the local market. Atorvastatin was a gratis sample from Zydus Cadila Pvt. Ltd. (Gujarat, India). Serum alanine transferase (ALT), aspartate transferase (AST), alkaline phosphate (ALP), and triglyceride (TG) kits were procured from Coral Clinical System, Tulip diagnostic kits Pvt. Ltd., Goa, India. Serum Leptin level was measured using Rat LEP ELISA kit procured from Everon Life Sciences, New Delhi. Total cholesterol (TC) and HDL-cholesterol and LDL cholesterol kits were procured from AUTOSPAN liquid gold cholesterol diagnostic kit, Vadodara (Gujarat, India).
Plant materials and plant extraction
The dried bark of F. racemosa Linn. was identified and authenticated by a qualified botanist at J&J College of Science with specimen number stored at the department PCL/ FR/2018. The bark was air-dried under shade, powdered, and defatted with petroleum ether (60–80°C) using Soxhlet apparatus, then extracted with methanol (99%) by successive solvent extraction and the final extracted sample was evaporated to dryness using a rotary evaporator. Dry yield (12.6%) powder (methanolic extract of F. racemosa [FRM]) was used for in vivo study.
Animals and treatment protocol
Adult male Wistar rats weighing 200–250 g were obtained from Zydus Research Centre, Gujarat. The animals were housed in polypropylene cages under standard controlled conditions (temperature: 23 ± 2°C, humidity: 50 ± 5% and 12 h light/dark cycle) and provided with free access to a standard pellet diet and water ad libitum. All experimental studies were conducted in accordance with the Committee for the Purpose of Control and Supervision of Experiments on Animals guidelines and approved by the Institutional Animal Ethics Committee (IAEC), Ramanbhai Patel College of Pharmacy, Changa. (Protocol No.: RPCP/ IAEC/2018-19/R28)
After acclimatization of 1 week, 40 animals were divided into two groups and fed (normal pellet diet; n = 6) or (high-fat diet; n = 34) for 5 consecutive weeks. The composition and preparation of HFHF diet are[20,24,25] mentioned in [Table 1].
| Ingredients | Diet (g/100 g) |
|---|---|
| Powdered NPD* | 37.0 |
| Vegetableghee (44% palmitic acid, 5% stearic acid., 39% oleic acid [monounsaturates], 10% linoleic acid [polyunsaturated]) | 25.0 |
| Casein | 10.0 |
| Fructose | 20.0 |
| Cholesterol | 5.0 |
| Vitamin and mineral mix | 3.0 |
From the starting of the 6th week, disease control animals were further divided into one disease control: Three FRM treated and one standard treated group. Accordingly, six groups of rats were maintained from 6th to 10th weeks as follows:
Group I: Normal – diet-fed rats (n=6)
Group II: DC – HFHF diet-fed rats (n=6)
Group III: FRM-1 – Received HFHF diet and FRM 100 mg/kg; p.o. (n=6)
Group IV: FRM-2 –Receive HFHF diet and FRM 200 mg/kg; p.o. (n=6)
Group V: FRM-2 - Receive HFHF diet and FRM 400 mg/kg; p.o. (n=6)
Group VI: Std - Receive HFHF diet and atorvastatin 20 mg/kg; p.o. (n=6).
Water and diet were provided ad libitum and body weight was recorded at regular time intervals. At the end of 10 weeks, the animals were fasted overnight and after blood collection animal was sacrificed by cervical decapitation for biochemical parameters assessment. Livers were removed for organ weight, oxidative parameters measurement, and histopathological evaluation.
Serum biochemical parameters
Serum leptin ALT, AST, and TG levels were measured as per kit manufacturer’s instruction (Tulip diagnostic kits Pvt. Ltd.). TC and HDL-cholesterol were measured using AUTOSPAN liquid gold cholesterol diagnostic kit and LDL cholesterol was measured using Friedewald’s equation.[26]
Measurement of oxidative markers
Liver tissue was separated from each rat, washed in ice-cold saline (0.9% NaCl), weighed (1 g), and homogenized in chilled phosphate buffer (pH 7.4). The homogenate was centrifuged at 800 rpm and supernatant was separated for measuring reduced glutathione (GSH), malondialdehyde (MDA), superoxide dismutase (SOD), and catalase (CAT).[5,20,27,28]
Histopathological observation
Liver tissues were fixed in 10% formalin solution for 24 h at room temperature. Fixed liver tissue was embedded in paraffin and cut into thin (5 μm) section. The section were stained with hematoxylin and eosin (H & E) dye for histopathological evaluation and observed under a light microscope (×20).
Statistical analysis
The result data represented as mean ± SEM (n = 6). The statistical analysis was carried out by one-way analysis of variance by Dunnett’s multiple comparison tests and t-test. P < 0.05 was considered significant.
RESULTS
Phytochemical screening results
Phytochemical screening of FRM suggested the presence of tannins, flavonoids, steroids, and triterpenoids [Table 2].
| Reagent | Observation | Interference |
|---|---|---|
| Conc. H2SO4 | Reddish brown | Steroids/ |
| Liebermann–Burchard | triterpenoids | |
| test | present | |
| Aq. NaOH | Reddish brown | Flavonoids |
| Mg-HCl | Magenta | present |
| Aq. FeCl3 | Greenish black | Tannins, |
| flavonoids present | ||
| Aq. Lead acetate | White precipitate | Tannins present |
| Ammonia solution | No change | Anthraquinone |
| 5% Aq. KOH | glycosides absent | |
| Picric acid | No precipitation | Alkaloids absent |
| Mayer’s reagent | ||
| Dragendorff’s reagent |
Biochemical estimation results
After 10 weeks of study, liver index was showed significant different for disease control group compared to normal control. FRE, 400 mg/ kg dose showed significant reduction in liver index compared to disease control rats [Figure 1]. After 10 weeks, results observed from biochemical parameters were shown significant (P < 0.05) elevation in ALT [Figure 2a], AST [Figure 2b], Cholesterol [Figure 3a], reduction in HDL [Figure 3b], increase in LDL [Figure 4a], Triglyceride [Figure 4b] and VLDL [Figure 5] levels in disease control group compared to normal control group rats. In FRM treatment group (100, 200, and 400 – mg/kg), reduction in AST and ALT levels was observed significantly, which was reduced in dose, dependent on the manner compared to the disease control group. However, in TG, TC, LDL, and VLDL levels significant (P < 0.05) reduction was observed only in a medium and high dose of FRM (200 and 400 – mg/kg) and standard drug-treated rats, but not in low dose FRM (100 mg/kg) treated rats compared to disease control rats. HDL level was seen to significantly increase in medium and high dose of FRM (200 and 400 – mg/kg) treated rats compared to disease control group. There was a significant increase in the serum leptin level (P < 0.05) in HFHF diet-fed rats compared to normal control rats. While in high dose, FRM treated rats significant (P < 0.05) reduced leptin was observed compared to disease control rats [Figure 6].
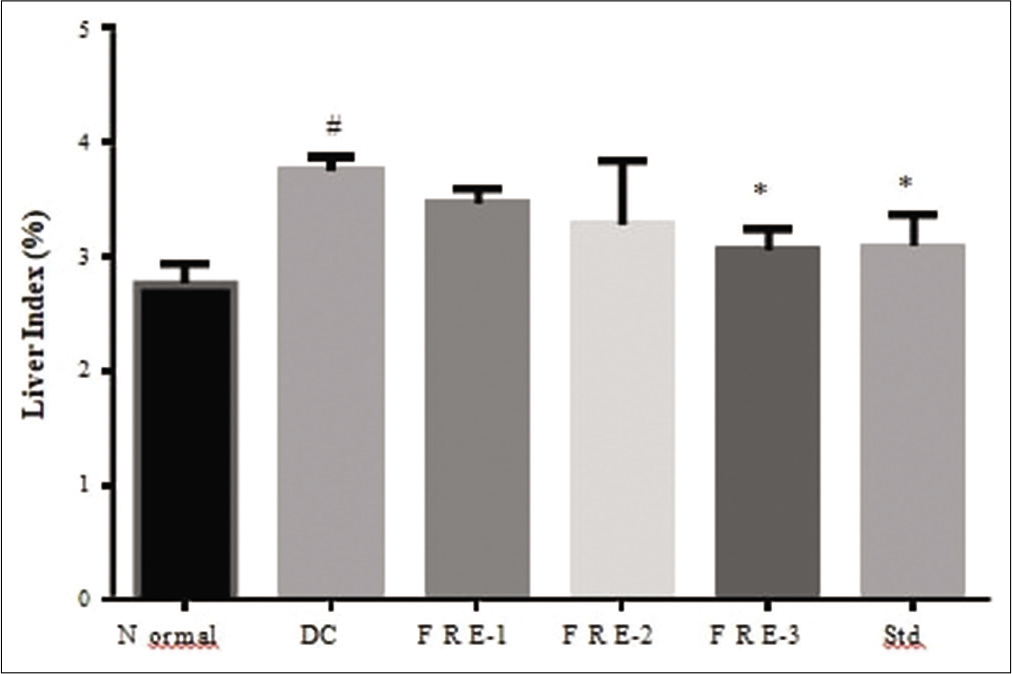
- Effects of methanolic extract of Ficus racemosa (FRM) on liver index (liver-body wt ratio) DC= disease control; FRE-1= 100mg/kg; FRE-2= 200mg/kg; FRE-3= 400mg/kg; Std= 20mg/kg Atorvastatin #Significantly different from normal control group, P < 0.05; *Significantly different from disease control group, P < 0.05.
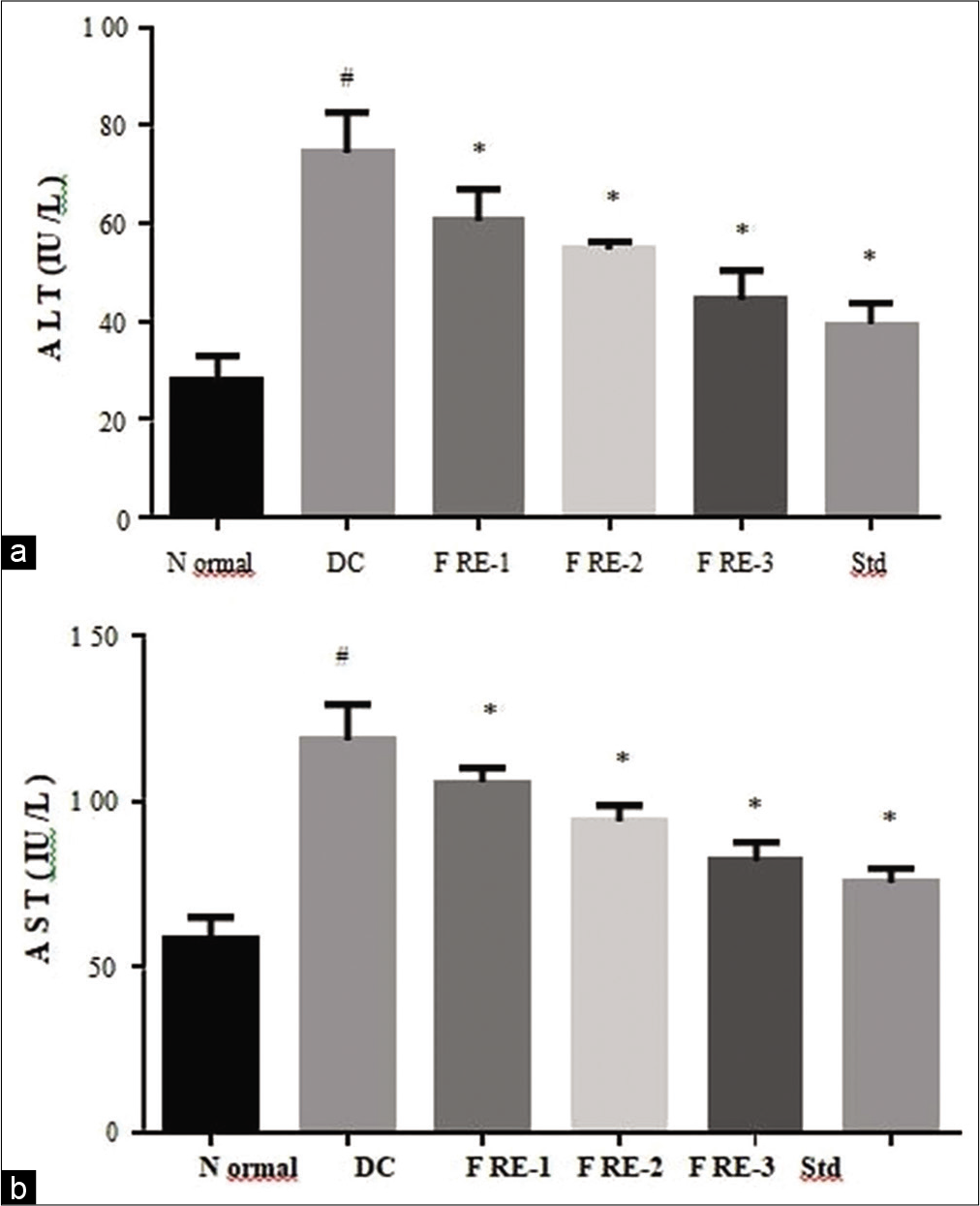
- Effects of methanolic extract of Ficus racemosa (FRE) on serum Aspartate transferase activity (a) and serum Alanine transferase activity (b) DC= disease control; FRE-1= 100mg/kg; FRE-2= 200mg/kg; FRE-3= 400mg/kg; Std= 20mg/kg Atorvastatin #Significantly different from normal control group, P < 0.05; *Significantly different from disease control group, P < 0.05.
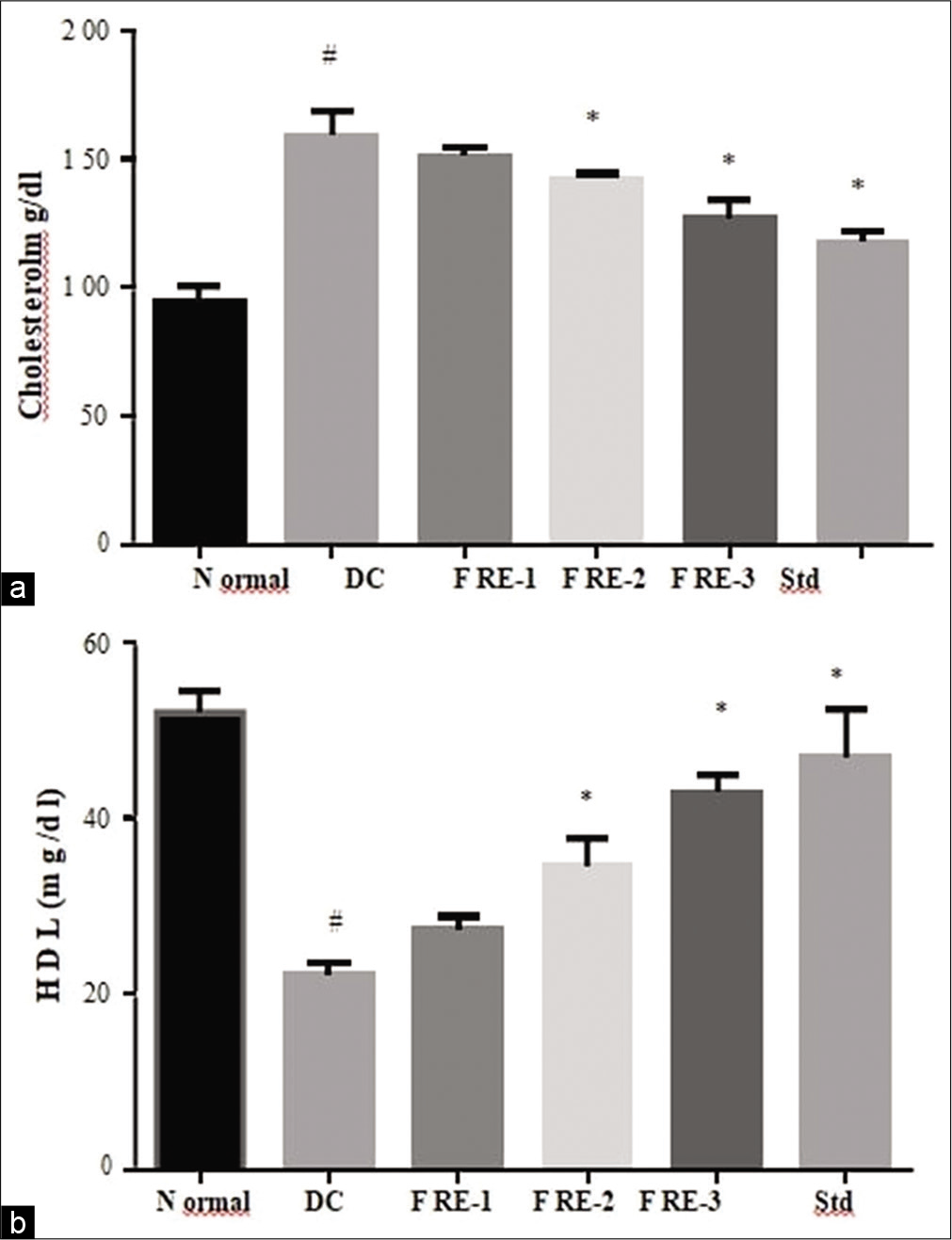
- Effects of methanolic extractof Ficus racemosa (FRM) on serum cholesterol (a) and HDL level (b) DC= disease control; FRE-1= 100mg/kg; FRE-2= 200mg/kg; FRE-3= 400mg/kg; Std= 20mg/kg Atorvastatin #Significantly different from normal control group, P < 0.05; *Significantly different from disease control group, P < 0.05.
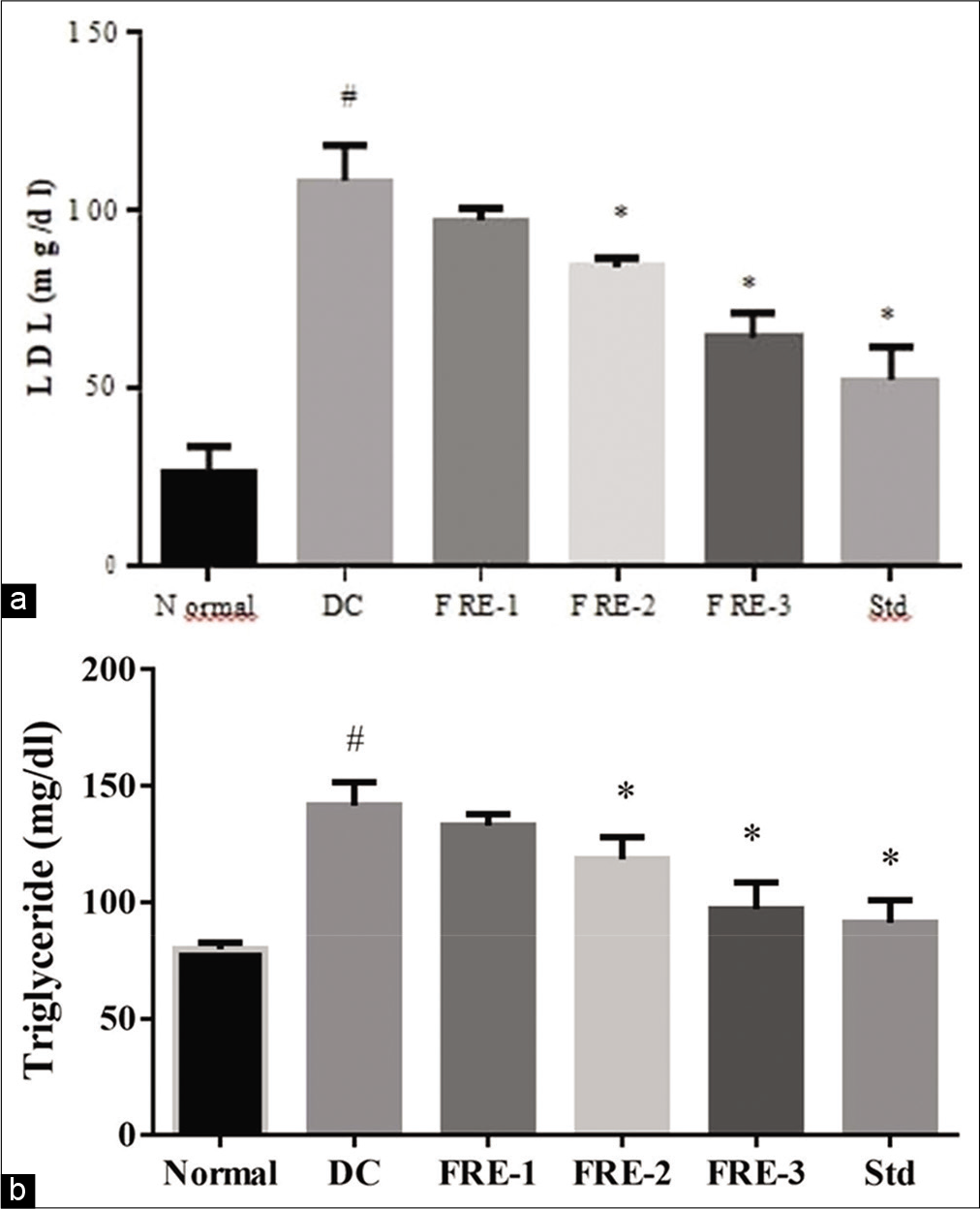
- Effects of methanolic extract of Ficus racemosa (FRM) on serum triglyceride (a) and LDL (b) level DC= disease control; FRE-1= 100mg/kg; FRE-2= 200mg/kg; FRE-3= 400mg/kg; Std= 20mg/kg Atorvastatin #Significantly different from normal control group, P < 0.05; *Significantly different from disease control group, P < 0.05.
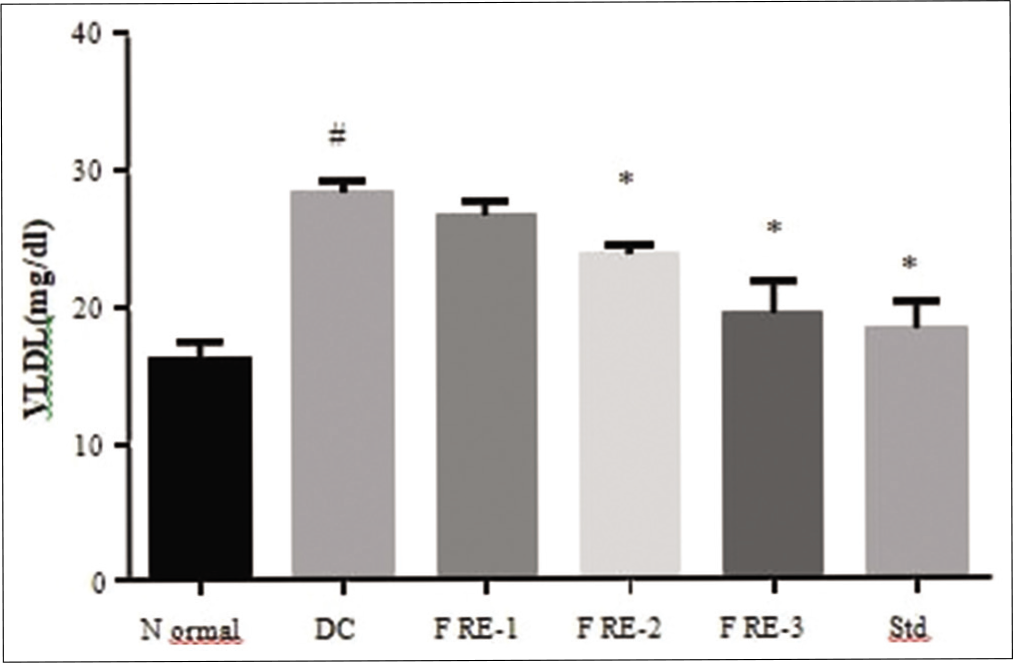
- Effects of methanolic extract of Ficus racemosa (FRM) on serum VLDL level DC= disease control; FRE-1= 100mg/kg; FRE-2= 200mg/kg; FRE-3= 400mg/kg; Std= 20mg/kg Atorvastatin #Significantly different from normal control group, P < 0.05; *Significantly different from disease control group, P < 0.05.
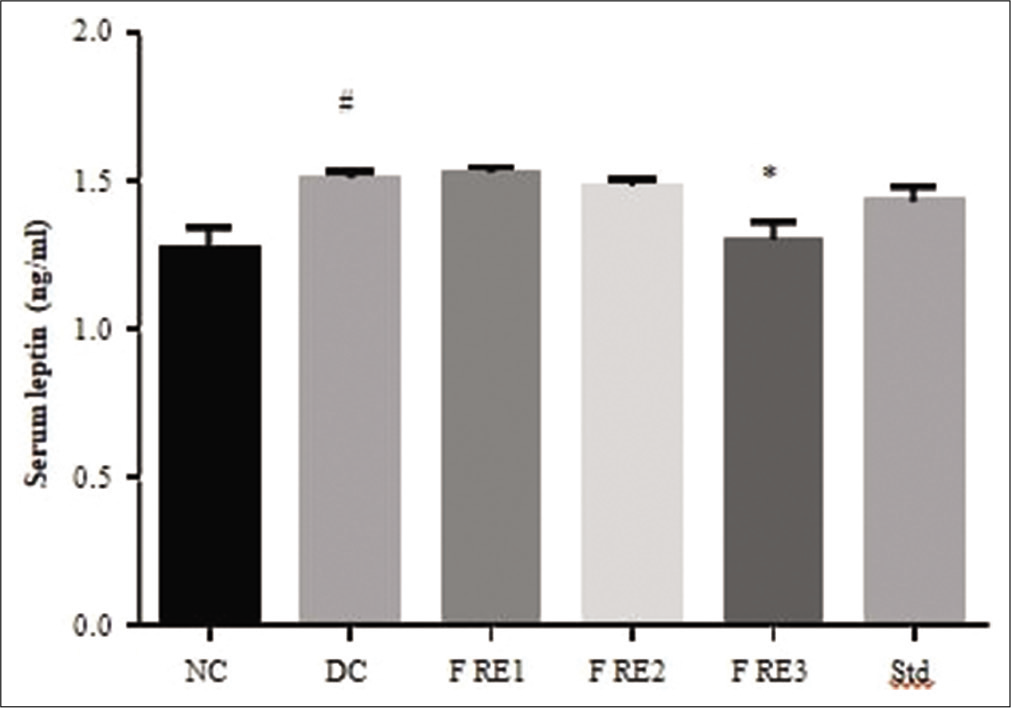
- Effects of methanolic extract of Ficus racemosa (FRM) on serum leptin level DC= disease control; FRE-1= 100mg/kg; FRE-2= 200mg/kg; FRE-3= 400mg/kg; Std= 20mg/kg Atorvastatin #Significantly different from normal control group, P < 0.05; *Significantly different from disease control group, P < 0.05.
Estimation of oxidative markers
HFHF diet-fed rats exhibited higher MDA level [Figure 7a] in liver tissue homogenate compared to normal control group. In FRM treated groups, the reduction in MDA level observed, but it was not statistically significant. 400 mg/kg FRM and atorvastatin treated rats showed significant (P < 0.05) reduction in MDA levels compared to the disease control group. Antioxidant markers such as GSH [Figure 7b], SOD [Figure 8a], and CAT [Figure 8b] activity were observed significantly (P < 0.05) to be reduced in disease control rats liver compared to normal control rats. However, 400 mg/kg FRM and atorvastatin treated rats showed significant (P < 0.05) elevation in GSH, SOD, and CAT enzymes activity compared to the disease control group.
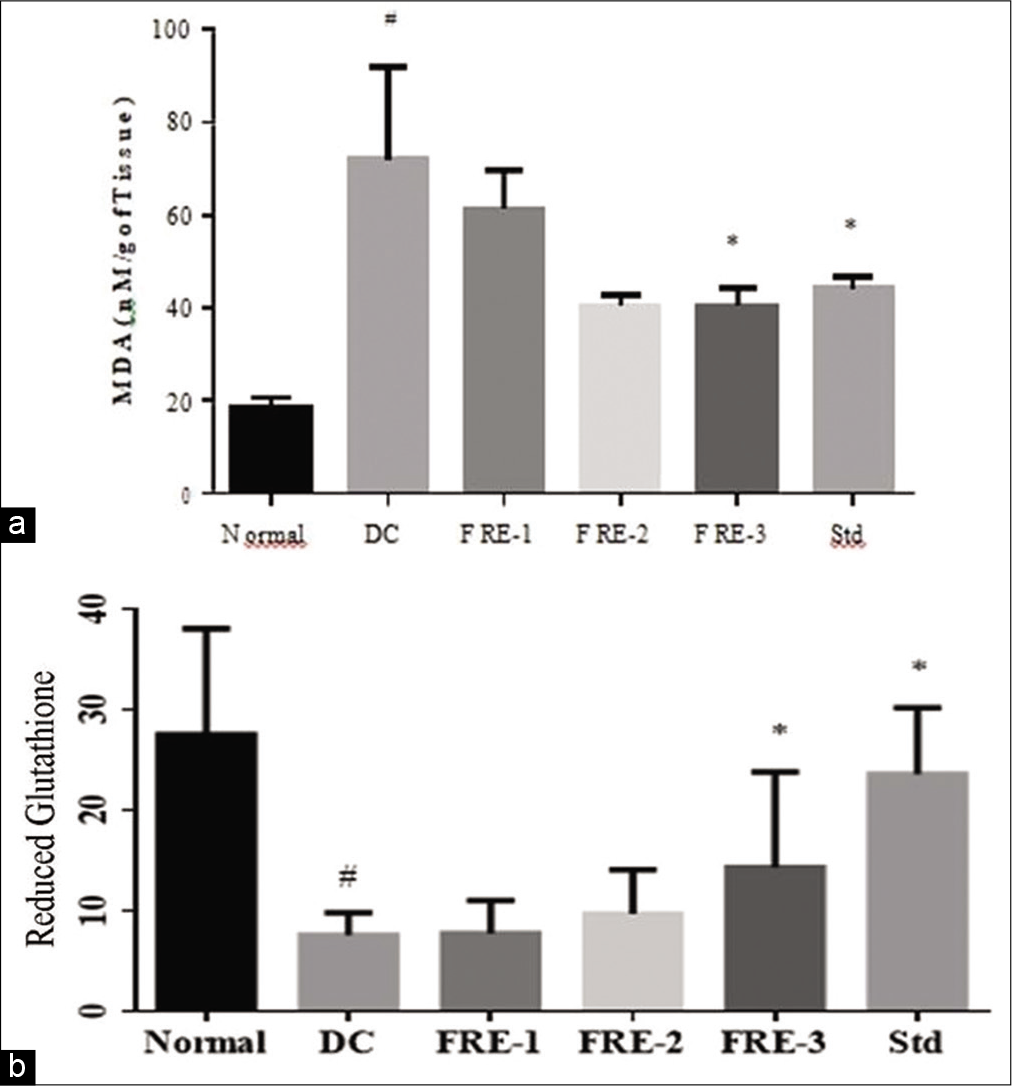
- Effects of methanolic extract of Ficus racemosa (FRM) on Reduced glutathione (a) level in rat liver DC= disease control; FRE-1 = 100 mg/kg; FRE-2 = 200 mg/kg; FRE- 3 = 400 mg/kg; Std = 20 mg/kg Atorvastatin (b) Malondialdehyde #Significantly different from normal control group, P < 0.05; *Significantly different from disease control group, P < 0.05.
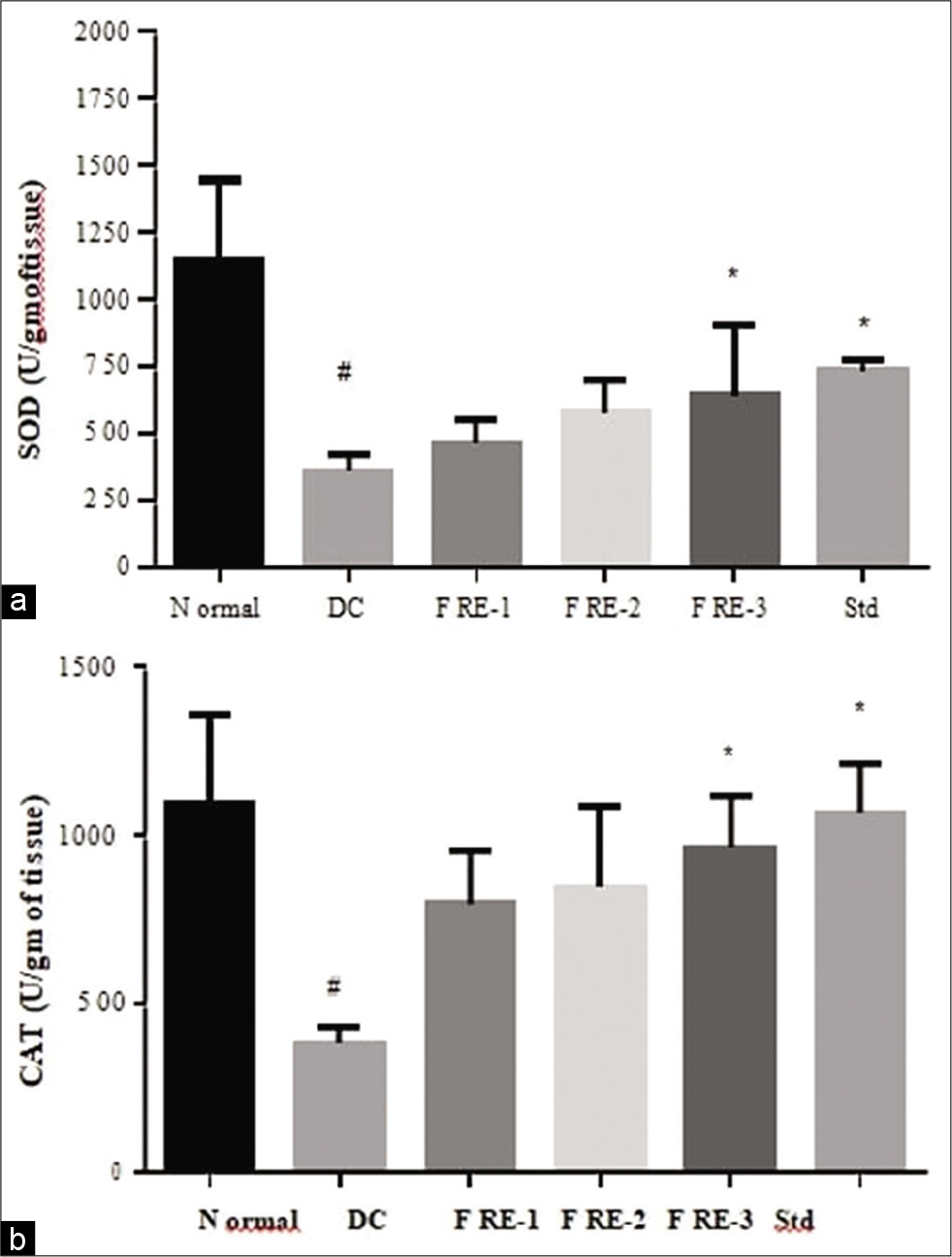
- Effects of methanolic extract of Ficus racemosa (FRM) on Superoxide Dismutase (a) and Catalase (b) level in rat liver DC= disease control; FRE-1= 100mg/kg; FRE-2= 200mg/kg; FRE- 3= 400mg/kg; Std= 20mg/kg Atorvastatin #Significantly different from normal control group, P < 0.05; *Significantly different from disease control group, P < 0.05.
Histopathology assessment in liver tissue
Histology of control group livers [Figure 9a] appeared to be normal. In contrast, the liver from HFHF diet-fed rats [Figure 9b] showed fatty changes in the hepatocyte with macro- and micro-vesicular fat droplets. The liver section of low and moderate dose FRM treatment [Figure 9c and d] showed lesser microvacuoles disposition compared to the disease control group and high dose FRM [Figure 9e] and standard treated rats [Figure 9f] significantly preserved normal hepatic morphology.
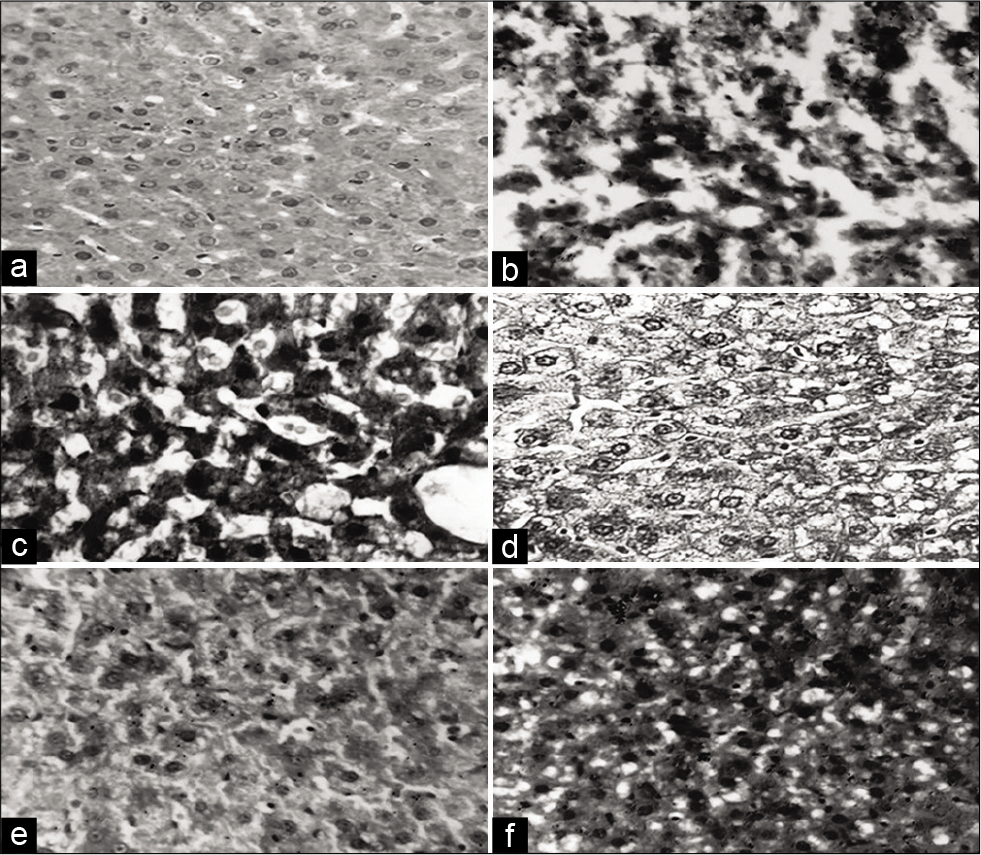
- Photomicrograhs of liver sections (H & E staining, 20X). Liver section of (a) Normal control, (b) Disease control, (c) FRE 100mg/kg (d) FRE 200mg/kg (e) FRE 400mg/kg (f) Atorvastatin 20mg/kg.
Overall 400 mg/kg was considered as optimum dose of F. racemosa for the treatment of NAFLD.
DISCUSSION
Herbal medicines are blooming rapidly as an alternative to primary healthcare, even in developed countries. Due to its multi-targeted therapeutic nature, the effectiveness of many hepatoprotective herbal plants was wildly explored in NAFLD condition.[29] The present study was the first to investigate the effectiveness of FRM bark in in vivo NAFLD condition. NAFLD is a multifactorial disease; therefore, the development of ideal animal model for NAFLD that would mimic the natural history and metabolic characteristics of human disease condition is challenging. Evidence suggests that dietary models are more closely reflected in the NAFLD condition compared to other animal models for NAFLD.[30,31] Along with the previous result of over-nutrition and sedentary lifestyle, recent evidence suggests that diet high in fructose also increases the risk development of NAFLD.[32] A combination of high-fat and high-fructose diet increases delivery of fatty acids through portal circulation and increase de novo lipogenesis.[33] This leads to the accumulation of fat in the liver and increases the vulnerability to further events such as oxidative stress and steatohepatitis, although the progression of hepatic steatosis to steatohepatitis required lengthy feeding period.[34] Our aim was to investigate the efficacy of the plant extract in the initial phase of the NAFLD spectrum. Research suggests that a high-calorie diet leads to body weight gain and elevation liver index (liver/body weight ratio) due to accumulation of fat pads mostly in the abdominal area.[35] The same was seen in the HFHF diet-fed groups in this study. It is reported that FRM treatment produces a reduction in body fat disposition in a moderate manner and similar results were observed in the present study. The liver size was also seen to be increased in HFHF fed rats while significant reduction was seen in high dose of FRM and standard treated group. Admission of HFHF diet is associated with hepatocellular damage and microvesicular steatosis. Elevated hepatic marker enzymes (ALT and AST) suggest chances of presence of hepatic cell damage. The increased level of these enzymes was seen in the disease control group. Treatment with different doses of FRM significantly prevents the increased activity of these enzymes. FRM conserves cell integrity and prevents cell damage in the liver to maintain the survival of functionally active cells. This result is comparable with the research reported by Faiyaz and Asna (2010) who observed the hepatoprotective activity of FRM in CCl4- treated rats.[36] This effect could be due to the presence of bergenin in FRM, which is reported to show notable hepatoprotective action. Fat accumulation, mainly hepatic TG filtration, is considered the first step in the development of a disease, even though the mechanism of NAFLD is still under exploration and this fat accumulation in the liver results from dysregulation of TGs and FFAs.[37] As mentioned earlier, fructose is a lipogenic compound; it plays a role in the elevation of hepatic TGs level through generating substrates for DNL.[33] In the present study, treatment with HFHF for 10 weeks produces significantly elevation TGs, TC, and LDL and reduction in HDL level. The amount of these serum lipid markers was found significantly reversed in FRM treated group comparable to that of the standard treated group.
Lipid dysregulation in HFHF diet fed rats was connected to the induction of oxidative stress in hepatocytes which favors a disease progression. Hypothesis for progressive cycle for NAFLD progression suggests the involvement of ROS formation, metabolic disease, and inflammation.[32] ROS-induced oxidative stress produces MDA as a byproduct. Results of the current study showed increased level of MDA and diminished levels of GSH, SOD, and CAT in HFHF-diet-fed rats liver tissue homogenate. GSH, CAT, and SOD enzymes protect liver from free radicals and reflect detoxification activity of the liver. Decreased level of GSH was found in the disease control group, which is relatable with other study results of impaired antioxidant defense activity of fructose-fed rats.[38] Treatment with antioxidants was reported to improve NAFLD conditions. Plant’s phenolic compounds play a great role as primary free-radical terminators (antioxidants). The phytochemical screening test found the presence of phenolic compounds (mainly tannins and flavonoids) in FRM, and this evidence is also supported by a phytochemical screening article of F. racemosa. A high dose of FRM treated rats showed enhanced antioxidant defense activity significantly compared to disease control group.
Higher level of leptin in serum was observed in the disease control rats. Studies suggest that leptin resistance may have a functional role to play in the pathogenesis of NAFLD.[10,39] Leptin is the main hormone, which is secreted from adipose tissue, and elevation in leptin level shows an excess amount of fat in the liver and intestine of animals.[40] Fructose ingestion also plays a role in leptin resistance.[41] Leptin resistance leads to higher leptin level in the serum, which may result in IR and development of NAFLD.[39] Improvement in serum leptin level prevents hepatic steatosis in animal models by affecting both lipid and glucose metabolism.[25] This result was observed in rats treated with high dose FRM. Thus, we hypothesized that constituents present in FRM might have a role in the reduction of the increased levels of leptin in the serum. Histopathological studies showed that HFHF diet induces fat droplets accumulation in hepatocytes with macrovesicular and microvesicular fatty changes, which is the same as expressed in other studies.[35,42] It is possible that increased liver weight in also associated with higher number of fat vacuoles in the hepatocytes. Research finding of Poudya et al. (2010) also supported these fatty changes in the liver by admission of high carbohydrate and high-fat-diet in the rats. These histological changes are corelatable with elevated lipid and liver function markers.[43] Improvement in hepatic architect is considered as a major sign of positive improvement in NAFLD. This was observed in high dose FRM treated groups, which is explained by reduced level of lipids and TG levels in the serum. In earlier study, F. racemosa had suggested improvements in functional and structural markers in diabetic neuropathy model.[44]
CONCLUSION
This study indicated the preventing effect of F. racemosa bark against HFHF diet-induced NAFLD possibly through a combination of antidiabetic, antioxidant, and hypolipidemic effects. These results rationalized its use in NAFLD conditions. Further, active phytoconstituents isolation from the extract for experimental in vivo and clinical studies is required to establish the mechanism(s) responsible for pharmacological action.
Limitation
Phytoconstituents isolation from the F. racemosa Linn. was challenging task and Yield of bio fractions was major challenge for in vivo efficacy experiments.
Future recommendations
As such no specific treatment option is available for NAFLD; further clinical studies will be required to establish the mechanism(s) responsible for pharmacological action of active constituents of F. racemosa Linn.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
This study was financially supported by Ramanbhai Patel College of Pharmacy, Charotar University of Science and Technology, Changa.
Conflicts of interest
There are no conflicts of interest.
References
- Traditional uses, medicinal properties, and phytopharmacology of Ficus racemosa: A review. Pharm Biol. 2010;48:672-81.
- [CrossRef] [PubMed] [Google Scholar]
- Hepatoprotective effects of Ficus racemosa stem bark against carbon tetrachloride-induced hepatic damage in albino rats. Pharm Biol. 2010;48:210-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pharmacognostical studies on Ficus racemosa stem bark. Pharmacogn J. 2011;319:19-24.
- [CrossRef] [Google Scholar]
- Probiotic mixture improves fatty liver disease by virtue of its action on lipid profiles, leptin, and inflammatory biomarkers. BMC Complement Altern Med. 2017;17:43.
- [CrossRef] [PubMed] [Google Scholar]
- Taurine modulates antioxidant potential and controls lipid peroxidation in the aorta of high fructose-fed rats. J Biochem Mol Biol Biophys. 2002;6:129-33.
- [CrossRef] [PubMed] [Google Scholar]
- Combination of high-fat/high-fructose diet and low-dose streptozotocin to model long-term Type-2 diabetes complications. Sci Rep. 2018;8:424.
- [CrossRef] [PubMed] [Google Scholar]
- Non-alcoholic fatty liver disease: An expanded review. World J Hepatol. 2017;9:715-32.
- [CrossRef] [PubMed] [Google Scholar]
- Molecular pathways in non-alcoholic fatty liver disease. Clin Exp Gastroenterol. 2014;7:221-39.
- [CrossRef] [PubMed] [Google Scholar]
- The adipokines in the pathogenesis and treatment of non-alcoholic fatty liver disease. Hippokratia. 2016;20:259-63.
- [Google Scholar]
- Quantitative determination of serum triglycerides by the use of enzymes. Clin Chem. 1973;19:476-82.
- [CrossRef] [PubMed] [Google Scholar]
- The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD) Metabolism. 2016;65:1038-48.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American association for the study of liver diseases. Hepatology. 2018;67:328-57.
- [CrossRef] [PubMed] [Google Scholar]
- Cissus quadrangularis stem alleviates insulin resistance, oxidative injury and fatty liver disease in rats fed high fat plus fructose diet. Food Chem Toxicol. 2010;48:2021-9.
- [CrossRef] [PubMed] [Google Scholar]
- Non-alcoholic fatty liver disease (NAFLD) models in drug discovery. Expert Opin Drug Discov. 2018;13:193-205.
- [CrossRef] [PubMed] [Google Scholar]
- A role of Ficus species in the management of diabetes mellitus: A review. J Ethnopharmacol. 2018;215:210-32.
- [CrossRef] [PubMed] [Google Scholar]
- An evaluation of the protective role of Ficus racemosa Linn in streptozotocin-induced diabetic neuropathy with neurodegeneration. Indian J Pharmacol. 2015;47:610-5.
- [CrossRef] [PubMed] [Google Scholar]
- Animal models of NAFLD from the pathologist's point of view. Biochim Biophys Acta Mol Basis Dis. 2019;1865:929-42.
- [CrossRef] [PubMed] [Google Scholar]
- A review of hyperlipidemia and medicinal plants. Int J Pharm Sci Biomed Sci. 2013;2:219-37. Available from: http://www.sciepub.com/reference/96405 [Last accessed on 2021 Feb 02]
- [Google Scholar]
- Effect of metformin on ballooning degeneration in non-alcoholic steatohepatitis (NASH): When to use metformin in nonalcoholic fatty liver disease (NAFLD) Adv Ther. 2014;31:30-43.
- [CrossRef] [PubMed] [Google Scholar]
- New trends on obesity and NAFLD in Asia. J Hepatol. 2017;67:862-73.
- [CrossRef] [PubMed] [Google Scholar]
- Increased diacylglycerols characterize hepatic lipid changes in progression of human nonalcoholic fatty liver disease; comparison to a murine model. PLoS One. 2011;6:e22775.
- [CrossRef] [PubMed] [Google Scholar]
- The degree of hepatic steatosis associates with impaired cardiac and autonomic function. J Hepatol. 2019;70:1203-13.
- [CrossRef] [PubMed] [Google Scholar]
- Traditional medicinal herbs for the management of diabetes and its complications: An evidence-based review. Int J Pharmacol. 2015;11:874-87.
- [CrossRef] [Google Scholar]
- Herbal medicines for the treatment of non-alcoholic steatohepatitis: Current scenario and future prospects. Evid Based Complement Alternat Med. 2014;2014:648308.
- [CrossRef] [PubMed] [Google Scholar]
- Fructose and sugar: A major mediator of non-alcoholic fatty liver disease. J Hepatol. 2018;68:1063-75.
- [CrossRef] [PubMed] [Google Scholar]
- Study of prevalence of nonalcoholic fatty liver disease (NAFLD) in Type 2 diabetes patients in India (SPRINT) J Assoc Physicians India. 2014;62:651-2.
- [Google Scholar]
- A novel animal model of metabolic syndrome with non-alcoholic fatty liver disease and skin inflammation. Pharm Biol. 2015;53:1110-7.
- [CrossRef] [PubMed] [Google Scholar]
- Leptin is essential for the hepatic fibrogenic response to chronic liver injury. J Hepatol. 2002;37:206-13.
- [CrossRef] [Google Scholar]
- Histologic and metabolic derangement in high-fat, high-fructose, and combination diet animal models. Sci World J. 2015;2015:306326.
- [CrossRef] [PubMed] [Google Scholar]
- Non-alcoholic fatty liver disease: The hepatic consequence of obesity and the metabolic syndrome. Proc Nutr Soc. 2010;69:211-20.
- [CrossRef] [PubMed] [Google Scholar]
- Nutrition and physical activity in non-alcoholic fatty liver disease. J Diabetes Res. 2016;2016:4597246.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical epidemiology and disease burden of non-alcoholic fatty liver disease. World J Gastroenterol. 2017;23:8263-76.
- [CrossRef] [PubMed] [Google Scholar]
- Pathophysiology of non alcoholic fatty liver disease. Int J Mol Sci. 2016;17:2082.
- [CrossRef] [PubMed] [Google Scholar]
- Orexin activation counteracts decreases in nonexercise activity thermogenesis (NEAT) caused by high-fat diet. Physiol Behav. 2017;176:139-48.
- [CrossRef] [PubMed] [Google Scholar]
- Leptin in non-alcoholic fatty liver disease: A narrative review. Metabolism. 2015;64:60-78.
- [CrossRef] [PubMed] [Google Scholar]
- Olive leaf extract attenuates cardiac, hepatic, and metabolic changes in high carbohydrate-, high fat-fed rats. J Nutr. 2010;140:946-53.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of phytochemical profile and antidiabetic activity of Ficus racemosa (Linn) stem bark in rats. Indian Drugs. 2017;54:49-54.
- [Google Scholar]
- Toll-like receptor 4 is involved in the development of fructose-induced hepatic steatosis in mice. Hepatology. 2009;50:1094-104.
- [CrossRef] [PubMed] [Google Scholar]
- Antidiabetic effect of Ficus racemosa Linn, stem bark in high-fat diet and low-dose streptozotocin-induced Type 2 diabetic rats: A mechanistic study. Food Chem. 2012;132:186-93.
- [CrossRef] [PubMed] [Google Scholar]
- Phytochemistry, pharmacology, toxicology, and clinical trial of Ficus racemosa. Pharmacogn Rev. 2015;9:73-80.
- [CrossRef] [PubMed] [Google Scholar]
- Genistein can ameliorate hepatic inflammatory reaction in non-alcoholic steatohepatitis rats. Biomed Pharmacother. 2019;111:1290-6.
- [CrossRef] [PubMed] [Google Scholar]
- Protective role of Ficus racemosa in diabetes induced neuropathy: Structural and functional evidences. Indian Drugs. 2017;54:58-60.
- [Google Scholar]






