Translate this page into:
Carbamazepine-induced hypersensitivity pneumonitis in a patient with neuromyelitis optica: A case report
*Corresponding author: Furqan Mohd. Akram Khan, Department of Neurology, Dr. D. Y. Patil Vidyapeeth, Pune; D. Y. Patil Medical College, Hospital & Research Centre, Pune, Maharashtra, India. dr.furqankhan5489@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Khan FM, Dave D, Rohatgi S, Nirhale S, Rao P, Naphade P, et al. Carbamazepine-induced hypersensitivity pneumonitis in a patient with neuromyelitis optica: A case report. Indian J Physiol Pharmacol 2022;66:81-3.
Abstract
A 36-year-old female with serum anti-aquaporin-4 antibody-positive neuromyelitis optica spectrum disorder (NMOSD) on carbamazepine (CBZ) therapy for paroxysmal tonic spasms (PTS) developed Type 1 respiratory failure. High-resolution computed tomography chest showed diffuse ground-glass opacities in both lungs predominantly in bilateral perihilar region sparing subpleural regions and predominantly upper lobes with a smooth interlobular septal thickening. A transbronchial lung biopsy was consistent with hypersensitivity pneumonitis and following withdrawal of the CBZ and treatment with steroids her respiratory symptoms resolved. After stopping CBZ, PTS recurred, which was successfully treated with lacosamide. This is the first described biopsy-proven case of CBZ-induced hypersensitivity pneumonitis in the NMOSD patient.
Keywords
Neuromyelitis optica spectrum disorder
Paroxysmal tonic spasms
Carbamazepine
Hypersensitivity pneumonitis
Lacosamide
INTRODUCTION
In patients of neuromyelitis optica spectrum disorder (NMOSD), paroxysmal tonic spasms (PTS) are common and often disabling, with the incidence varying from 25% to 26.66%.[1] PTS has been defined as a paroxysmal episode of increased muscle tone, abnormal posture, and intense pain in one or more limbs with or without being triggered by movement or sensory stimulation. They can have a negative impact on the quality of life, limit activities of daily living and the rehabilitative process. PTS is caused by the transverse ephaptic transmission of neural activity produced by the transverse lesion in the spinal cord rather than a longitudinal lesion, it is thought that demyelination renders axons hypersensitive to minor insults and subsequent irritation of these axons facilitates ephaptic transmission between demyelinated axons, resulting in PTS.[2] Another hypothesis is that dysfunctional ion channels are involved in facilitating ephaptic transmission which may explain why sodium-channel blockers – such as carbamazepine (CBZ), topiramate, and lacosamide possess higher efficacy than other treatments.[3,4]
CBZ has been one of the most effective drugs in the treatment of PTS. Its use is often limited by the side-effect profile. Lacosamide can be used as an alternative to CBZ, as both have a common pharmacological action to block sodium channels.
There is only one published report of successful treatment of PTS with lacosamide in a patient with NMOSD who developed an adverse drug reaction (ADR) on CBZ.[4]
We report a case of a 36-year-old female NMOSD patient with severe PTS who developed CBZ- induced hypersensitivity pneumonitis, which was successfully treated with lacosamide.
CASE REPORT
A 36-year-old female with serum anti-aquaporin-4 antibody-positive NMOSD developed PTS while recovering from an attack of cervical longitudinally extensive transverse myelitis. The tonic spasms were characterised by flexion of the right fingers, wrist, and elbow and internal rotation of the shoulder. Some of the attacks also involved the right leg. Multiple episodes occurred daily. PTS was painful, with limited activities of daily living and the rehabilitation process. She was initially treated with escalating doses of baclofen, gabapentin, and diazepam without significant improvement. She was started on oral CBZ at a dose of 200 mg twice daily after she was tested negative for HLA-B* 1502. Prompt resolution in PTS was seen within 24 h of starting CBZ.
She was treated with 1 g of intravenous methylprednisolone for 5 days for an acute attack of NMOSD and was put on a tapering dose of oral prednisolone. She was induced with two infusions of 1-g rituximab given 15 days apart for prophylaxis of NMOSD. Before giving rituximab, latent tuberculosis was ruled out with a negative Quantiferon-TB gold test and her chest radiograph was unremarkable. Over 12 weeks, oral steroids were tapered and stopped. Two weeks after stopping steroids, the patient developed medical research council (MRC) Grade 2 dyspnoea which progressed gradually to MRC Grade 4 over a period of 4 weeks. Along with dyspnoea patient experienced fatigue and malaise without fever, cough, weight loss, or reduced appetite. History was significant for atopic diathesis, recurrent allergic rhinitis was present.
On admission, her peripheral capillary oxygen saturation (SpO2) was 68% breathing room air, respiratory rate was 26/min, heart rate was 112/min, blood pressure was 120/76 mmHg, she was afebrile with a core body temperature of 97.8°F. On auscultation of lungs, fine inspiratory crackles were present. The rest of the examination was normal.
Her arterial blood gas breathing room air showed Type 1 respiratory failure with pH = 7.462, pO2 = 54.3 mmHg, pCO2 = 30.5 mmHg.
The chest radiograph showed bilateral interstitial infiltrates.
High-resolution computed tomography (HRCT) thorax showed diffuse ground-glass opacities in both lungs predominantly in bilateral perihilar region sparing subpleural regions and predominantly upper lobes with smooth interlobular septal thickening [Figure 1].
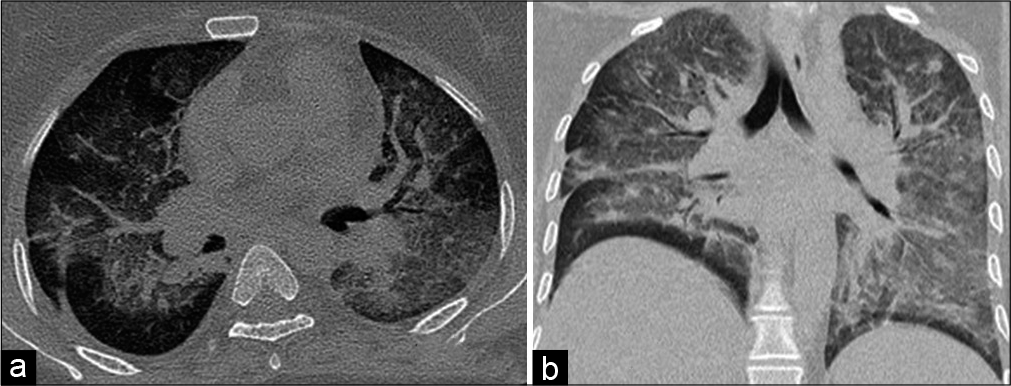
- (a) Axial; (b) coronal HRCT images, showing bilateral diffuse ground glass opacities, predominantly in bilateral perihilar region sparing subpleural regions with smooth interlobular septal thickening.
Results of routine blood analysis were normal including white blood cell and eosinophil counts, there were negative results for vasculitis screening (rheumatoid factor, antinuclear antibody, extractable nuclear antigens, and antiphospholipid antibody) and viral serology: Human immunodeficiency virus, hepatitis B, and hepatitis C. Serum CBZ levels were within normal limits.
The serum erythrocyte sedimentation rate was 20 in the 1st h, while C-reactive protein and procalcitonin levels were within the normal range.
Bronchoscopy with bronchoalveolar lavage and transbronchial biopsies was performed.
No bacteria were seen on Gram-stained preparations of bronchoalveolar lavage fluid (BALF), ZN stain for acid-fast bacilli was negative. CB-NAAT of BALF was negative. Cultures of the BALF and blood were negative. BALF showed 67% lymphocytes, 25% macrophages and 8% neutrophils.
Transbronchial lung biopsy showed interstitial expansion with predominant lymphocytic infiltration and few poorly formed non-caseating granulomas, suggestive of subacute hypersensitivity pneumonitis [Figure 2].
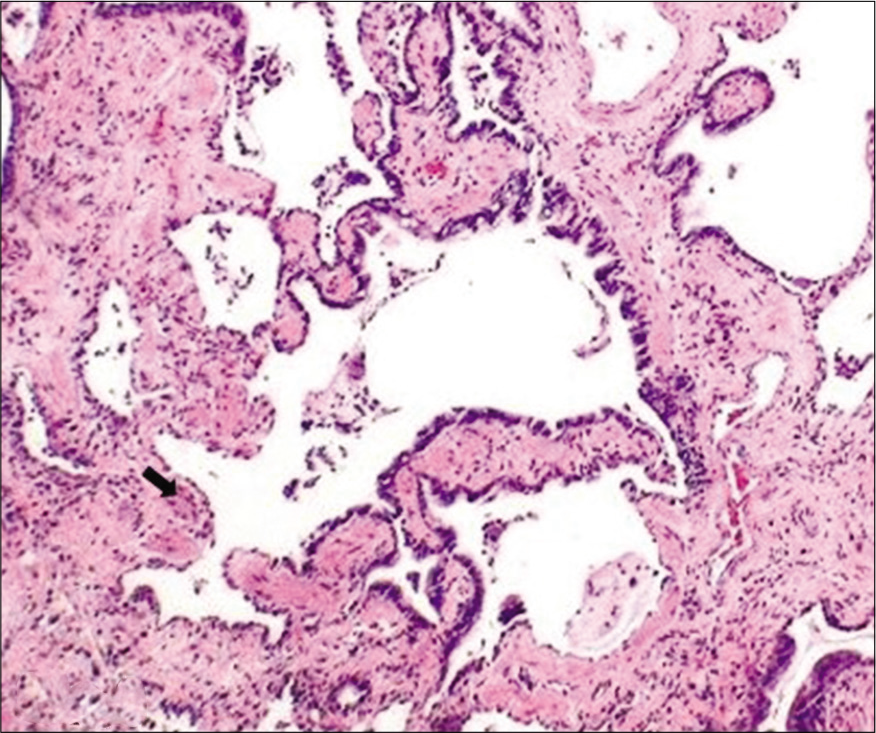
- Intermediate-magnification photomicrograph (haematoxylin and eosin; ×100) demonstrating showing interstitial lymphocytic predominant infiltrates with a non-caseating granulomas (arrow).
Based on the clinical picture, laboratory, radiological and biopsy findings, a diagnosis of hypersensitivity pneumonitis was made. As per Naranjo ADR probability scale, the ADR was probable, and as per WHO-UMC causality scale, the ADR was certain. The severity of ADR was Level 5 on the modified Hartwig and Siegel scale.
CBZ was discontinued and the patient was started on 1-g methylprednisolone for 5 days, followed by 1 mg/kg oral prednisolone tapered gradually over 8 weeks. Complete clinical improvement was seen by the end of 4 weeks. HRCT done at 4 weeks showed near-complete resolution of radiological findings [Figure 3].
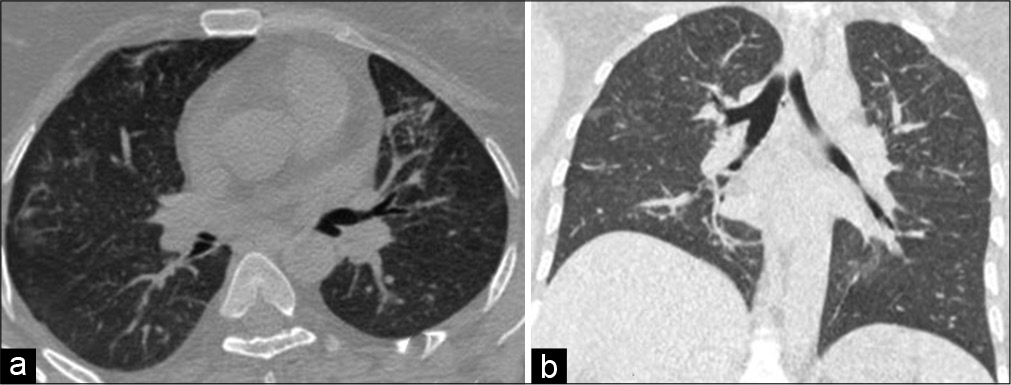
- (a) Axial; (b) coronal HRCT images, after 4 weeks of stopping carbamazepine and steroid therapy, showing near complete resolution of ground glass opacities and septal thickening.
Within 2 days of stopping CBZ severe, frequent PTS recurred.
Alternative sodium-channel blocking agents such as oxcarbazepine, phenytoin and lamotrigine were felt to be contraindicated because of a shared risk of hypersensitivity. She, therefore, was given lacosamide 200mg intravenous followed by oral lacosamide 100 mg 12 hourly and within 24 h, the PTS were markedly improved and subsequently ceased after increasing the dose of lacosamide to 200 mg 12 hourly.
DISCUSSION
CBZ -induced interstitial pneumonitis is a rare but well-described complication,[5-9] in most of the reported cases patients had asthma with or without eosinophilia which could likely be a part of atopic diathesis. The mechanism of lung injury is believed to be an immune-mediated hypersensitivity response.[10] This may partially explain the rarity of the condition in NMOSD, as this patient population is on immunosuppressant regimens, in this case, the onset of symptoms was after 2 weeks of stopping prednisolone.
Lacosamide can be used as an alternative for CBZ, as both have a common pharmacological action to block sodium channels, thereby making neurons less excitable and blocking ephaptic transmission which is believed to cause PTS. A. Baheerathan et al. reported successful treatment of PTS with lacosamide in a patient of NMOSD who developed Stevens-Johnson syndrome with toxic epidermal necrolysis on CBZ.[4]
CONCLUSION
In conclusion, CBZ therapy should be considered as a cause of hypersensitivity pneumonitis in the NMOSD population, presenting with respiratory distress, since CBZ withdrawal is the only effective treatment for further reducing lung injury and should be used with caution in patients with a history of atopic diathesis despite negative HLA-B* 1502 state. Lacosamide can be used as an alternative for the treatment of PTS in patients not tolerating or in whom CBZ is contraindicated.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Neuromyelitis optica: Association with paroxysmal painful tonic spasms. Neurología. 2016;31:511-5.
- [CrossRef] [Google Scholar]
- Spinal movement disorders in neuromyelitis optica: An under-recognized phenomenon. Mov Disord Clin Pract. 2016;3:596-602.
- [CrossRef] [PubMed] [Google Scholar]
- Successful treatment of paroxysmal tonic spasms with topiramate in a patient with neuromyelitis optica. Mult Scler Relat Disord. 2015;4:457-9.
- [CrossRef] [PubMed] [Google Scholar]
- Neuromyelitis optica spectrum disorder related tonic spasms responsive to lacosamide. Mult Scler Relat Disord. 2017;13:73-4.
- [CrossRef] [PubMed] [Google Scholar]
- Acute hypersensitivity pneumonitis associated with carbamazepine therapy. Chest. 1978;74:463-4.
- [CrossRef] [Google Scholar]
- Acute eosinophilic pneumonia due to hypersensitivity to carbamazepine. Rev Mal Respir. 1998;15:797-9.
- [Google Scholar]
- Carbamazepine-induced pneumonitis definitively diagnosed by accidental readministration. Nihon Kokyuki Gakkai Zasshi. 2005;43:150-4.
- [Google Scholar]
- Carbamazepine-induced interstitial pneumonitis in a lung transplant patient. Respir Med. 2006;100:1660-2.
- [CrossRef] [PubMed] [Google Scholar]
- Activation of drug-specific CD4+ and CD8+ T cells in individuals allergic to sulphonamides, phenytoin, and carbamazepine. J Immunol. 1995;155:462-72.
- [Google Scholar]






