Translate this page into:
Effect of maternal anemia on breast milk iron status
*Corresponding author: Pauline Anand, Ph.D, Department of Physiology, Father Muller Medical College, Mangalore, Karnataka, India. paulineanand@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Abraham NV, Anand P. Effect of maternal anemia on breast milk iron status. Indian J Physiol Pharmacol 2021;65(1):35-8.
Abstract
Objectives:
Nutritional anemia is highly prevalent in lactating mothers. It is postulated that anemic pregnant women secrete less iron in their breast milk. This study was aimed to compare the iron levels in breast milk samples of anemic and non-anemic lactating pregnant women and to correlate breast milk iron levels with the hemoglobin (Hb) status of anemic and non-anemic mothers.
Materials and Methods:
A case–control study was conducted on 120 pregnant women aged 20–30 years having a normal antenatal history. They were classified into non-anemic and anemic groups based on their Hb status; Group 1: Hb ≥11 g/dl and Group 2: Hb 7–10.9 g/dl, respectively.
Results:
Maternal blood Hb was significantly different between the groups (11.8 ± 0.6 vs. 10.2 ± 0.5 g/dL, P > 0.05). Breast milk iron levels did not vary significantly between the groups (938.8 ± 465.6 vs. 1084.8 ± 440.8 μg/dl). No correlation was observed between maternal Hb levels of anemic lactating mothers and breast milk iron status (r = 0.054, P = 0.424).
Conclusion:
Our research study validates the finding that maternal anemia did not affect breast milk iron concentration during the early post-natal period by showing the optimum iron levels in it. Therefore, exclusive breastfeeding is the ideal nutrition for infants.
Keywords
Maternal anemia
Maternal hemoglobin
Breast milk iron status
INTRODUCTION
Anemia is widely prevalent in India and other developing countries, especially among pregnant women. Nutritional anemia as iron deficiency anemia (IDA) is the most common cause of anemia during pregnancy. About 32 million women[1] especially pregnant women in middle- and low-income countries[2] are globally affected which leads to poor pregnancy outcomes.[3]
Iron supplementation during pregnancy is one of the most widely practiced public health measures, yet little is known about the benefits of supplemental iron to mother, fetus, and also during postnatal life. Nearly 50–80% of mothers suffer from IDA due to dietary insufficiency. As a consequence, there is an increased risk of premature delivery, fetal growth restriction, and perinatal mortality and morbidity.[4,5] Besides this, a low level of hemoglobin (Hb) among infants enhances morbidity from various infections.[6] Therefore, it is a double burden in the society caused by anemic mother and infants.
Furthermore, the World Health Organization and Academy of Pediatrics explicitly recommend that exclusive breastfeeding is the ideal nutrition for infants and is sufficient to support optimal growth for the first 6 months of life.[7,8] However, gaps in knowledge exist regarding the adequacy of providing optimum iron through breast milk in exclusively breastfed babies, especially with maternal anemia.
Few studies have reported that with maternal anemia, breastfed infants may become iron deficient,[7] and few have reported that exclusively breastfed infants should receive iron supplementation from 4 months of age.[8,9] Studies also say that complementary foods should be introduced before 6 months of age in exclusively breastfed infants.[10] On the contrary, a study finding has shown that maternal anemia did not affect breast milk iron concentration during early lactation.[11] Thus, the iron status of exclusively breastfed infants, in relation to iron levels of breast milk, has not been evaluated sufficiently. Moreover, maternal diet and regional variation also contribute to their iron status. Therefore, this study is aimed to assess the effect of maternal iron deficiency or IDA in breast milk iron status.
MATERIALS AND METHODS
A case–control study was conducted in a Medical College Hospital, Mangalore, Karnataka. The experimental protocol was approved by the Human Ethical Committee of the Institute. All study participants were informed of the purpose of this study in their local language before obtaining the signed consent during enrollment.
The sample size was calculated based on iron content of breast milk and with 80% power, 60 pregnant women in each group (anemic and non-anemic mothers) was decided. Thus, 120 pregnant women aged 20–30 years were selected for the study. Eligible women willing to participate were followed up after the delivery of the baby. Socio-demographic, anthropometric, obstetric, and dietary details were collected at recruitment. All women belonged to low socioeconomic status. They were non-vegetarian by diet except one. We included 60 anemic (Hb: 7–10.9 g/dl) and 60 healthy, non-anemic pregnant women (Hb: ≥11 g/dl) with normal antenatal history and an uncomplicated singleton delivery at term gestation at the hospital. Exclusion criteria were preeclampsia, hypertension, heart disease, gestational diabetes, antepartum hemorrhage, and other chronic medical illnesses. The blood Hb estimation was done using an automated cell counter (Beckman coulter analyzer).
Collection of breast milk
2 ml of breast milk sample was collected for analysis of iron status. Breast milk was collected in sterile vials on either day 1, 2, or 3 after delivery because iron content in milk is maximum in the 1st few days of lactation.[10] Manual expression of breast milk was demonstrated to the mother and she was requested to collect the hind milk with the assistance of a trained nurse. After collection of the breast milk, samples were centrifuged and the supernatant was stored at -20°C until analysis. The measurements of iron status were done using a Colorimeter. The assay was done using Automated Chemistry Analyzer Cobas C 311 (Roche diagnostic kit). Ironbound to transferrin was released in an acidic medium (citric acid and sodium ascorbate). This mediated the reduction of ferric ions to ferrous ion. Ferrous ions (Fe II) then reacted with Ferrozine, a bidentate ligand, to form a violet-colored complex. The intensity of the complex formed was directly proportional to the amount of iron present in the sample and was measured photometrically. Values were expressed as μd/l.
Statistical analysis
Descriptive analysis was performed and values were expressed as mean and standard deviations. An independent t-test was done to compare the parameters in control and anemic groups. Pearson’s correlation was done to assess the relationship between maternal Hb levels and their breast milk iron status.
RESULTS
General characteristics of anemic and non-anemic mothers are represented in [Table 1]. Maternal blood Hb was significantly different between the groups (11.8 ± 0.6 vs. 10.2 ± 0.5 g/dL, P > 0.05). Babies of both the groups were delivered at term. The birth weight of babies did not vary between the groups. [Table 2] describes the biochemical parameters. It was seen that breast milk iron levels did not vary significantly between the groups (938.8 ± 465.6 vs. 1084.8 ± 440.8 μg/dl). A significant correlation was seen between maternal Hb levels of non-anemic lactating mothers with their breast milk iron status [r = –0.468, P = 0.03, Figure 1]. No correlation was observed between maternal Hb levels of anemic lactating mothers and breast milk iron status [r = 0.054, P = 0.424, Figure 2].
| Parameters | Non-anemic lactating women (n=60) | Anemic lactating women (n=60) |
|---|---|---|
| Maternal Hb (g/dl) | 11.8±0.6 | 10.2±0.5* |
| Age (years) | 26.0±4.0 | 25.0±4.1 |
| Parity (%) | ||
| Primi | 60 | 53 |
| Multi | 40 | 47 |
| Gestational age at birth (weeks) | 38.3±2.1 | 38.3±1.5 |
| Birth weight (kg) | 2.7±0.5 | 2.9±0.4 |
All values represented as mean±SD. Maternal Hb is significantly different between the non-anemic and anemic lactating women,*P>0.05. Hb: Hemoglobin
| Parameters | Non-anemic lactating women (n=60) | Anemic lactating women (n=60) |
|---|---|---|
| Maternal Hb (g/dl) | 11.8±0.6 | 10.2±0.5* |
| Breast milk iron (µg/dl) | 938.8±465.6 | 1084.8±440.8 |
All values represented as mean±SD. Breast milk iron levels were not significantly different between the two groups. Hb: Hemoglobin
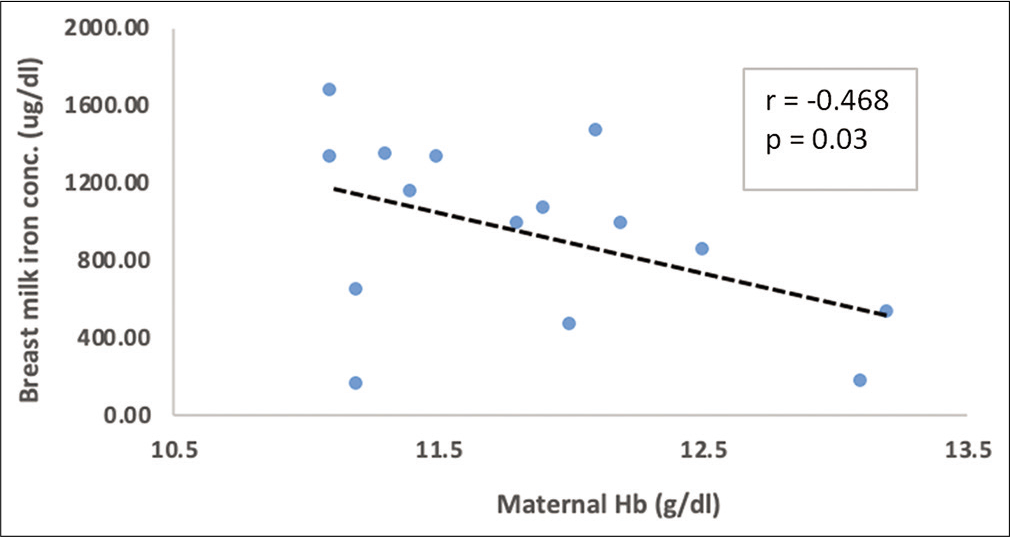
- Correlation between maternal hemoglobin with breast milk iron in non-anemic lactating women.
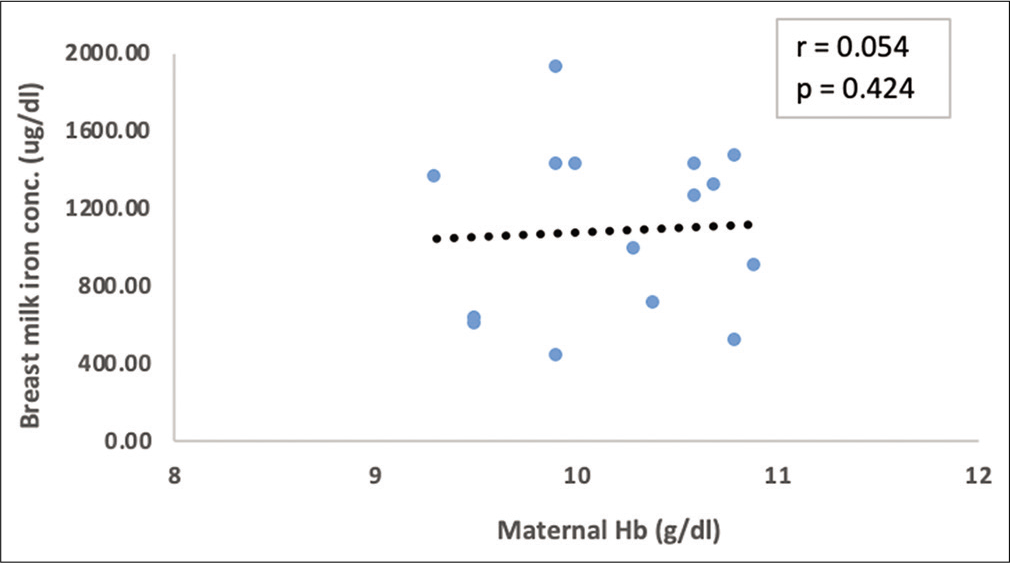
- Correlation between maternal hemoglobin with breast milk iron in anemic lactating women.
DISCUSSION
This study has shown a key finding that maternal anemia did not affect the breast milk iron concentration during early lactation supporting the findings from a similar study.[12] Our finding also helps to understand the association between maternal Hb level and its iron status in breast milk. It will help in creating awareness regarding the importance of maternal nutrition especially in consuming an iron-rich diet both during the antenatal and postnatal periods.
Human milk is a dynamic, bioactive fluid that changes in composition from early to late lactation[12] and it is uniquely suited for the infants in its nutritional composition to promote their survival and healthy development. Nutrients of milk originate by the synthesis in the lactocyte, few are dietary in origin, and some originate from maternal stores.[12] During pregnancy, physiologic iron demands increase substantially to support fetoplacental development and maternal adaptation to pregnancy.
It has been reported that due to maternal anemia, breastfed infants may become iron deficient.[7] A study has also suggested the need to introduce complementary foods before 6 months of age in exclusively breastfed infants to prevent anemia in infants.[10] In our study, although a negative correlation was seen between Hb of non-anemic, lactating mothers with breast milk iron status, larger sample size will probably validate this association positively; as it is known that mothers with normal Hb levels will transfer optimum iron to the infant through breast milk.[13]
Given the physiological and biochemical changes that occur during lactation, maintaining iron homeostasis needs special consideration. It has been documented that the total iron requirements during the lactation period are low.[14] Moreover, there is a substantial increase in the amount of iron in form of increased red cell mass for the mother after delivery, markedly striking a positive iron balance in the mother during lactation. This seems like a well-adapted purpose to meet the requirement for the infant as well as compensating maternal iron stores in preparation for the next pregnancy.[14] In continuation, although iron content in human milk is lower, it is significantly more bioavailable (45%–100%) for the growing infants.[15]
We further explored if breast milk iron levels varied between the non-anemic and anemic lactating mother. There was no significant change in the breast milk iron levels in both the groups, with normal levels of iron in the milk which, implicates that maternal anemia did not affect breast milk iron concentration during the early postnatal period. Therefore, exclusive breastfeeding is the ideal nutrition for infants and is sufficient to support optimal growth for the first 6 months of life.
Nutritional counseling of pregnant women during their routine antenatal visits would have positively influenced the women of this study. Moreover, there are regulating factors which maintain the concentrations of iron in milk such as genetic variation, health, and diet. There could be a possibility of the upregulation of iron absorption in maternal anemia which has influenced the breast milk iron level.[16]
Studies have reported increased cord erythropoietin levels in pregnant women with low Hb levels, suggesting induced fetal erythropoiesis in maternal anemia. Hence, there is a possibility of maintaining the optimum iron level in breast milk due to the enhanced effect of erythropoiesis on iron absorption.[17]
Moreover, the level of maternal Hb does not influence fetal Hb concentration; unless the mother suffers from severe anemia,[18,19] and the women in our study have shown to have moderate anemia. There is a requisite to quantify the range of maternal iron deficiency, which stars to affect the iron content in milk, in which the protective mechanisms would fail to achieve appropriate Hb synthesis in the early postnatal period.
CONCLUSION
Our research study corroborates the finding that maternal moderate anemia did not affect breast milk iron concentration during the early postnatal period by showing the optimum iron levels in it.
Acknowledgment
We thank Priyanka S Bannikoppa Ph.D., for her valuable inputs in supervising different aspects of the study including statistics and manuscript preparation. We also thank the obstetricians who helped in monitoring of the subjects. We acknowledge and are thankful to all the study subjects for their participation who made this study possible.
Declaration of patient consent
Institutional Review Board permission was obtained for the study.
Financial support and sponsorship
This study was funded by Indian Council of Medical Research for Short term student project.
Conflicts of interest
The authors declare that there is no conflict of interest.
References
- Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995-2011: A systematic analysis of population-representative data. Lancet Glob Health. 2013;1:e16-25.
- [CrossRef] [Google Scholar]
- Anaemia in low-income and middle-income countries. Lancet. 2011;378:2123-35.
- [CrossRef] [Google Scholar]
- World Bank, Disease Control Priorities Project, editors. Disease Control Priorities in Developing Countries. (2nd ed). New York, Washington, DC: Oxford University Press, World Bank; 2006. p. :1401.
- [CrossRef] [Google Scholar]
- Anemia, iron and pregnancy outcome. J Nutr. 2000;130(Suppl 2S):443S-7S.
- [CrossRef] [PubMed] [Google Scholar]
- Experiences and challenges in industrialized countries: Control of iron deficiency in industrialized countries. J Nutr. 2002;132(Suppl 4):820S-4S.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for the Use of Iron Supplements to Prevent and Treat Iron Deficiency Anemia.
- [Google Scholar]
- The Optimal Duration of Exclusive Breastfeeding: Report of the Expert Consultation 2001.
- [Google Scholar]
- Breastfeeding and the use of human milk. Pediatrics. 1997;100:1035-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anemias of inadequate production In: Behrman RE, Kliegman R, Jenson HB, eds. Nelson Textbook of Pediatrics (17th ed). Philadelphia, PA: Saunders; 2004. p. :1606-17.
- [Google Scholar]
- Effects of age of introduction of complementary foods on iron status of breast-fed infants in Honduras. Am J Clin Nutr. 1998;67:878-84.
- [CrossRef] [PubMed] [Google Scholar]
- Iron and lactoferrin in milk of anemic mothers given iron supplements. Nutr Res. 1995;15:681-90.
- [CrossRef] [Google Scholar]
- Human milk composition: Nutrients and bioactive factors. Pediatr Clin North Am. 2013;60:49-74.
- [CrossRef] [PubMed] [Google Scholar]
- Mother's iron status, breastmilk iron and lactoferrin-are they related? Eur J Clin Nutr. 2006;60:903-8.
- [CrossRef] [PubMed] [Google Scholar]
- Erythrocyte incorporation of ingested 58Fe by 56-day-old breast-fed and formula-fed infants. Pediatr Res. 1993;33:573-6.
- [CrossRef] [PubMed] [Google Scholar]
- Iron absorption in relation to iron status. Model proposed to express results to food iron absorption measurements. Scand J Haematol. 1981;27:201-8.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of maternal anemia and iron deficiency on fetal erythropoiesis: Comparison between serum erythropoietin, hemoglobin and ferritin levels in mothers and newborns. J Matern Fetal Neonatal Med. 2002;11:329-32.
- [CrossRef] [PubMed] [Google Scholar]
- Cord blood haemoglobin, iron and ferritin status in maternal anaemia. Acta Paediatr Scand. 1983;72:545-8.
- [CrossRef] [PubMed] [Google Scholar]
- Fetal iron status in maternal anemia. Acta Paediatr. 1996;85:1327-30.
- [CrossRef] [PubMed] [Google Scholar]






