Translate this page into:
Exploring pain status and flexibility in fibromyalgia patients: Effect of 20 sessions of yoga therapy
*Corresponding author: Renu Bhatia, Department of Physiology, All India Institute of Medical Sciences, New Delhi, Delhi, India. renuaiims28@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar A, Yadav RK, Venkataraman S, Kumar U, Singh A, Deepak KK, et al. Exploring pain status and flexibility in fibromyalgia patients: Effect of 20 sessions of yoga therapy. Indian J Physiol Pharmacol. 2023;67:262-9. doi :10.25259/IJPP_297_2023
Abstract
Objectives:
Fibromyalgia (FM) is a common neurological chronic health problem that causes widespread pain and tenderness (sensitivity to touch) throughout the body. Most often, people with this chronic illness complain of fatigue and sleep deprivation. Besides psychosomatic illness, neurological problems such as depression, anxiety, and memory loss are also reported by patients.
Materials and Methods:
Pain, flexibility, and range of motion in 18 FM patients were assessed before and after 20 sessions of yoga therapy. Subjective assessment of pain was done using a visual analogue scale (VAS) and pain catastrophising scale scores. Tender points were also localised. Objective assessment of pain was done using quantitative sensory testing of the left and right shoulder regions. Flexibility and range of motion were assessed using Schober’s and Sit and Reach tests, respectively, before and after yogic intervention.
Results:
Mean VAS score, age, and body mass index of patients at baseline were 7.05 ± 0.8, age 35.1 ± 8.9 Kg/m2, and 27.8 ± 2.9 kg/m2, respectively. VAS score (3.3 ± 1.3, P < 0.05) was significantly reduced after the intervention; pain catastrophisation was also reduced in the patients after the therapy. Flexibility (Schober’s test scores) and range of motion (Sit and Reach test scores) significantly increased after 20 sessions of regular yoga therapy. Pressure pain threshold at the left shoulder and pressure pain tolerance at the right shoulder were significantly increased after the intervention (P < 0.05).
Conclusion:
Twenty sessions of yoga therapy can relieve pain and improve the flexibility and range of motion of FM patients.
Keywords
Fibromyalgia
Pain
Flexibility
Yoga therapy
Lifestyle intervention
INTRODUCTION
According to the American College of Rheumatology (ACR), fibromyalgia (FM) is a common musculoskeletal and neurological chronic health problem, characterised by widespread pain and tenderness (sensitivity to touch). The pain and tenderness are felt throughout the body, including some specific sites which are known as tender points. Most often, people with this chronic illness complain of tiredness and sleep disturbance.[1] FM is also characterised by psychosomatic symptoms such as headache, memory loss, and cognitive symptoms also known as brain fogging. Some patients also complain about problems with vision, gastrointestinal symptoms, skin diseases, dizziness, nausea, urinary bladder infections, and dysmenorrhea.[2] Diagnosis of the disease is done using the widespread pain index and symptoms severity score which should be for at least 3 months with the presence of at least 11 out of 19 tender points in the patients.[1,3] Disease is 80–85% more frequent in women than in men.[4] FM has varied pathophysiology; the main cause of the disease is still unknown. Only symptomatic relief by a few Food and Drug Administration-approved drugs such as pregabalin, duloxetine, and milnacipran has been reported in the literature.[3] Drug dependence and drug tolerance are common as there is no permanent cure for the disease.
Some alternative interventional strategies such as physical activity, massage therapy; hydropathy, repetitive transcranial magnetic stimulation, transcutaneous electric nerve stimulation, Yoga, and Meditation have been explored for pain relief.[5-8] In 2019, stretching, aerobic, and resistance exercises were recommended by the European Alliance of Associations for Rheumatology as non-invasive treatment strategies for FM patients.[9] Despite a wide range of management strategies, pain relief is not possible. Understanding the pain profile and disability parameters is important to provide better pain management options.
Yoga-based interventions focus on mind and body relaxation through Asanas (Postures), relaxation techniques, and group activities. Pain relief by yoga therapy has been reported by subjective ratings in various chronic pain conditions. However, there is a paucity of literature on objective assessment of pain and flexibility in FM patients before and after yoga therapy. Therefore, the present study was designed to investigate the effect of a 20-session yogic intervention on pain sensitivity, flexibility, and range of motion in FM patients, both subjectively and objectively.
MATERIALS AND METHODS
Ethical approval of the study was granted by the Institute Ethics Committee, All India Institute of Medical Sciences, New Delhi, India (Ethical Approval No. IECPG-611/28.10.2021). The study was an interventional pilot study. Patients were recruited from the outpatient departments of Rheumatology, Physical Medicine and Rehabilitation, Psychiatry, and Orthopaedics.
Informed consent was obtained from all the patients before the onset of the study. Both male and female FM patients aged 21– 50 years diagnosed by ACR, 2010 criteria and have widespread pain manifested for at least 3 months with a minimum of 11 out of 19 specified tender points were included in the study. Pregnant and lactating female patients and patients having alcohol and drug abuse, implants/pacemakers, neurological disorders, chronic systemic illness, traumatic injuries, and patients having chronic pain other than FM pain were excluded from the study.
We screened 29 FM patients fulfilling ACR, 1990 diagnostic criteria; 22 were recruited and enrolled for 20 sessions of a regular yoga regimen. All the patients had moderate-to-high pain (visual analogue scale [VAS] score ≥5). Four patients attended <12 sessions or left the therapy in between; therefore, the baseline and post-yoga data were analysed for 18 FM patients who completed the pain and flexibility assessment after the regular yoga regimen [Figure 1].
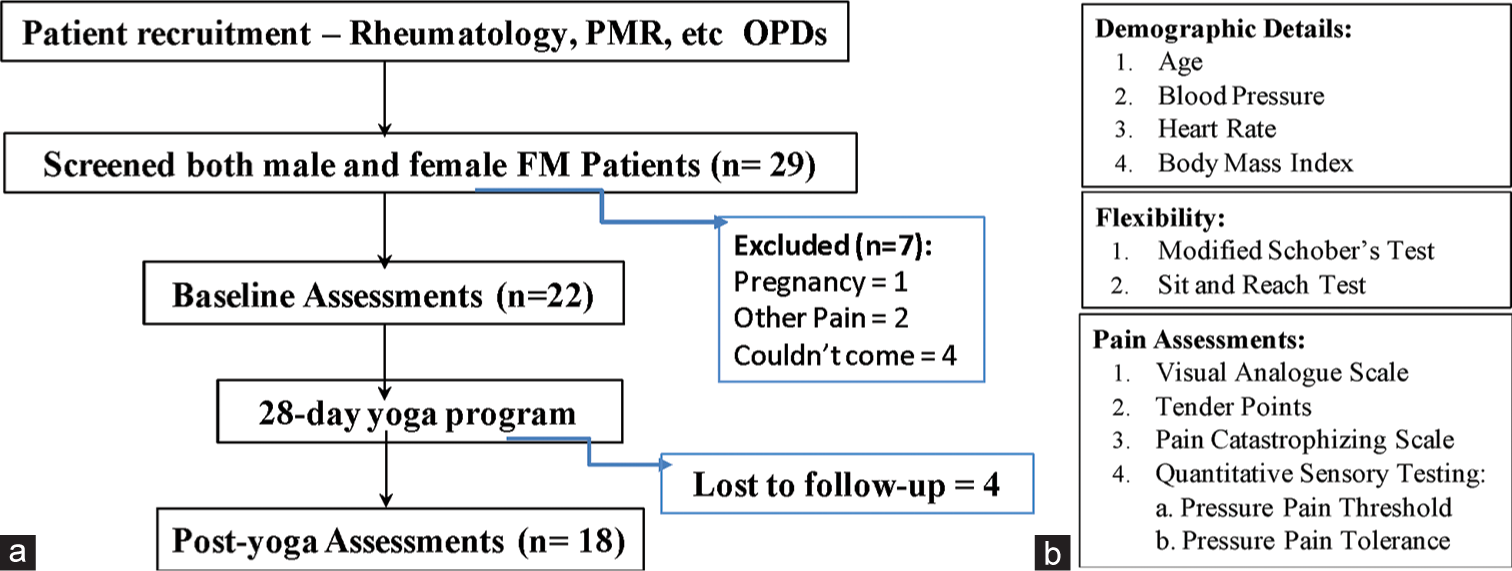
- Study design, (a) Workflow, (b) Parameters assessed at baseline and post-yoga.
Subjective assessment of pain was done using a pain numerical rating scale - VAS and a descriptor-pain catastrophising scale (PCS). Former is the most common pain rating scale with a minimum score of ‘0’ to a maximum score of ‘0.’ Here, ‘0’ indicates - no pain, ‘1’ - minimum experienced pain, ‘5’ - moderate pain, and 10 is the worst possible pain.
PCS is a self-evaluative device to rate pain in clinical and non-clinical settings. It was developed by Sullivan et al. in 1995 to quantify multidimensional components of catastrophe at a descriptive level - rumination, magnification, and helplessness as predictors of the intensity of physical and emotional distress.[10] It is a 13-item descriptor, which has a maximum score of 52 (13 items × 4 maximum score/item). Responses to all 13 items of the PCS questionnaire were noted on the physical copy by the patient or their attendant. The higher the PCS score, the higher the disability and catastrophe associated with chronic pain.[10]
Objective pain assessment was done using quantitative sensory testing (QST) using pressure pain parameters. Both pressure pain threshold (PPT) and pressure pain tolerance were assessed at two different sites of the pain manifestation (left and right shoulders) using a computerised Algometer (Medoc Pvt. Ltd., Israel) [Supplementary Figure 1]. The algometer device comprises - a digital Algomed to apply pressure manually; a response tool attached to the computer system which detects and saves the threshold and tolerance value of the participant in Medoc Main Station software tool and a computerised VAS to rate pain on the numerical rating scale of 0–10, objectively [Figure 2]. Pressures applied were measured in KiloPascals (KPa). For each parameter, there were four trials which were averaged after the tests.
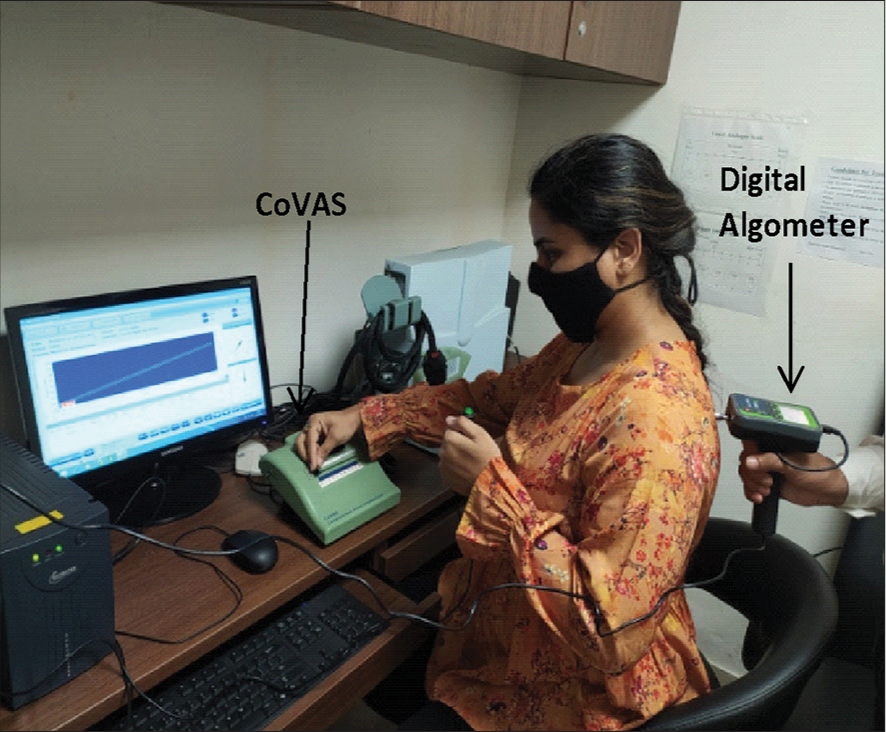
- Quantitative sensory testing for pressure parameters. A digital algometer was used to apply pressure on specific points to record pain using computerised visual analogue scale (CoVAS).
Flexibility and range of motion were measured with Schober’s test and using a Sit and Reach box. Schober’s test was first described by Van Adrichem and Van der Korst; it is the most reliable tool to measure a lumbar range of motion.[11] Participants were asked to stand erect, arms at their sides and feet placed about 15 cm apart; it uses two marks one over the spine connecting two posterior superior iliac spines (PSIS) and the other over 15 cm superior to the first mark. The volunteers were instructed to remove their shoes and expose their back from the gluteal fold to the mid-thoracic spine with left and right PSIS fully exposed. Inferior margins of the volunteer’s PSIS were marked, and a ruler was used to locate and mark a midline point on the sacrum (inferior mark). Then, the final mark (superior mark) was marked on the lumbar spine 15 cm above the midline sacral mark (inferior mark). Then, the examiner demonstrated the proper procedure of forward bending with the arm hanging in front and keeping the knees straight. At the end of the flexion range of motion, the distance between the two marks was noted [Figure 3].
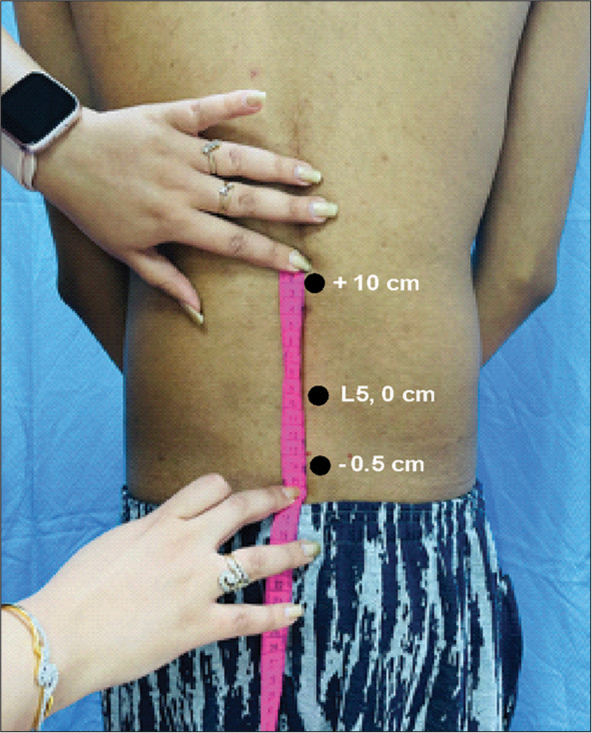
- Schober’s test for lumbar flexion. L5 is marked first and then 15 cm from the −5 cm from L5 is the landmark that is investigated for lumbar flexion (+10 cm).
The Sit and Reach test is the most common linear flexibility test used for the measurement of extensibility of the hamstrings and lower back (American College of Sports Medicine Sit and Reach Box) [Supplementary Figure 2]. It involves sitting of participant on the floor with legs stretched out without shoes and soles placed flat against the Sit and Reach box. With the palms facing downward and knees extended straight, the subject reached forward along the measuring line as far as possible and the distance was recorded. Furthermore, they did the test in one smooth movement rather than a bouncing or jerking movement. The test was repeated thrice, and values were noted in centimetres and averaged [Figure 3].
Yoga Therapy Protocol: Patients reported to Integral Health and Wellness Clinic, Department of Physiology; in the morning with breakfast at least 2 h before the onset of yoga sessions. Patients were advised to take a healthy diet – ‘Saatvik Aahaar’ which primarily includes green and leafy vegetables and fruits during the intervention. Each session of yoga therapy (5 sessions/week for 4 consecutive weeks; a total of 20 sessions) comprised two sub-sessions: A yoga session (60 min) and a counselling session (30 min). The former consists of Asanas (physical postures), relaxation techniques, and pranayama (breathing exercises) whereas the latter consists of motivation, group discussion, and dietary advice. A maximum of 6 persons at a time are allowed in each session after proper instructions and monitoring their blood pressure and heart rate. Asanas consisted of supine, prone, standing, and sitting postures. All Asanas and restoration techniques were supervised by expert yoga therapists and counsellors throughout the yoga regimen [Annexure 1].
Statistical analysis
Data from both male and female FM patients were pooled and analysed. All the statistical analyses were done using the statistical package for the social sciences (SPSS) 2.1.11 (SPSS Inc., Chicago, USA). Paired t-test was performed to compare the baseline parameters with the post-yoga parameters. Shapiro–Wilk test was done to check the normality of the data. The level of significance was set at 0.05; all the parameters having P < 0.05 were considered significant.
RESULTS
Eighteen FM patients (mean age 35.1 ± 8.9 years) were able to complete the yoga regimen (20 sessions in 28 days); post-yoga assessments were done 4 weeks after the completion of the yoga therapy. The mean body mass index (BMI) of FM patients (n = 18) who have completed regular yoga therapy was 27.8 ± 2.9 kg/m2 and 23.8 ± 2.1 kg/m2 at baseline and post-yoga, respectively. A significant decrease in BMI after 20 sessions of yoga therapy was recorded. Mean systolic and diastolic blood pressure of the patients at baseline were 122.6 ± 15.1 mmHg and 84.05 ± 11.0 mmHg, respectively; we did not find any significant change in blood pressures post-yoga (Post-yoga: Systolic blood pressure = 115.4 ± 9.7 mmHg, diastolic blood pressure = 79.2 ± 6.9 mmHg). No significant change in mean heart rates of the FM patients was recorded after yoga therapy (Baseline: 80.8 ± 11.1 bpm and Post-yoga: 78.1 ± 8.7 bpm). Demographic details of FM patients (n = 18) are given in [Table 1].
| S. No. | Parameters (units) | Baseline | Post-yoga (28 days) |
|---|---|---|---|
| 1. | BMI (kg/m2) | 27.8±2.9 | 23.8±2.1 (#) |
| 2. | Blood pressure (mmHg) | ||
| Systolic | 122.6±15.1 | 115.4±9.7 | |
| Diastolic | 84.05±11.0 | 79.2±6.9 | |
| 3. | Heart rate (beats/min) | 80.8±11.1 | 78.1±8.7 |
Values are represented as mean±standard deviation. Hashtag (#) depicts comparison with baseline:P<0.05 using student’s t-test. BMI: Body mass index
A significant reduction was observed in VAS score (Baseline: 7.05 ± 0.8, Post-yoga: 3.3 ± 1.3; P < 0.01) and tender point counts (Baseline: 15.4 ± 2.9 and Post-yoga: 7.1 ± 4.8; P < 0.01) of the FM patients after 20 sessions of yoga therapy. The mean PCS score was also reduced after the yoga therapy in the FM patients (Baseline: 34.9 ± 2.8 and Post-yoga: 27.8 ± 2.2; P < 0.05) as given in [Figure 4]. PPT at the left shoulder (Baseline: 145.3 ± 78.1 KPa and Post-yoga: 169.9 ± 70.0 KPa; P < 0.05) of FM patients was found significantly elevated after the yoga therapy; but no significant difference was reported in pressure pain tolerance at the left shoulder (Baseline: 232.1 ± 88.9 KPa and Post-yoga: 241.5 ± 76.4 KPa; P > 0.05). No significant change in the PPT at the right shoulder (Baseline: 145.9 ± 75.1 KPa and Post-yoga: 160.1 ± 47.2 KPa; P > 0.05) was found in the FM patients after the therapy; but a significant increase in the pressure pain tolerance at the right shoulder (Baseline: 219.1 ± 94.2 KPa and Post-yoga: 238.2 ± 71.3 KPa; P < 0.05) was recorded after yoga therapy [Figure 5].
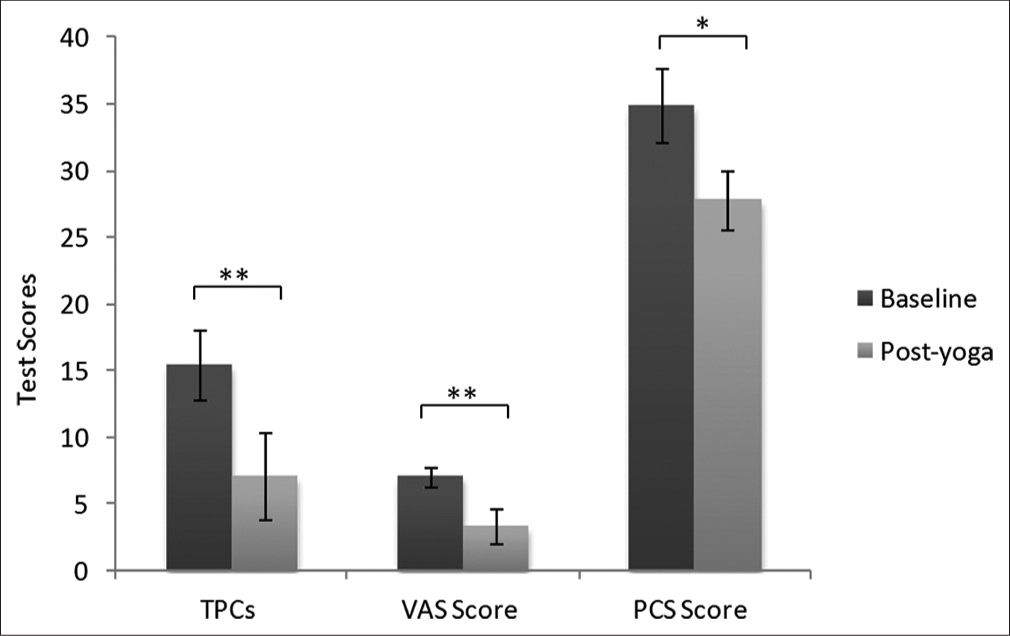
- Pain assessment of fibromyalgia patients at baseline and post-yoga. Data are represented as mean ± standard deviation of the test scores. Visual analogue scale and pain catastrophising scale scores were assessed subjectively whereas tender points were assessed by the clinician.*Depicts significance level (P < 0.05); **Depicts significance level (P < 0.01). Paired t-test was applied in the statistical package for the social sciences software tool for the comparison between 2 time points. TPCs: Tender point counts, VASL Visual analogue scale, PCS: Pain catastrophizing scale.
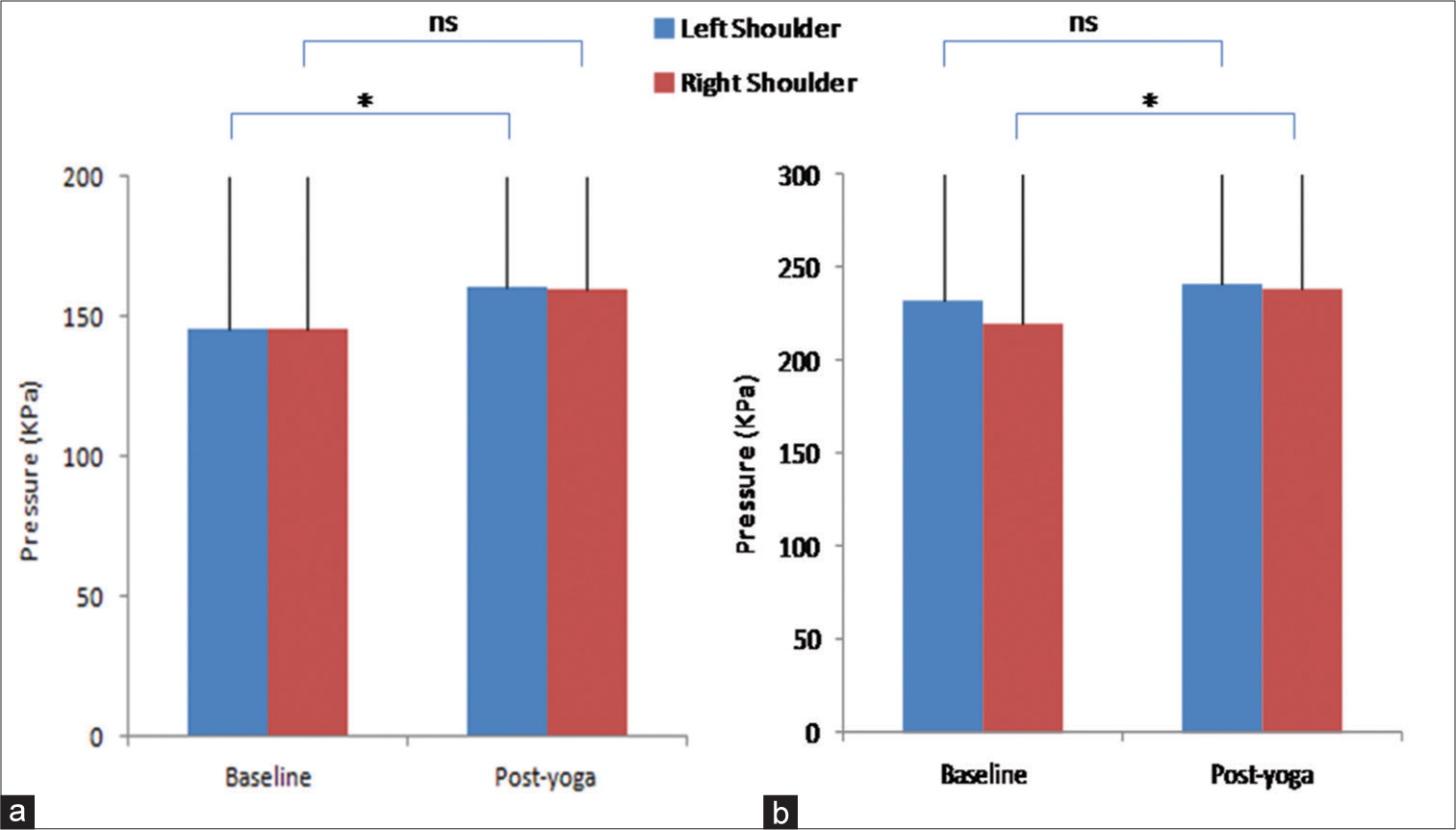
- Assessment of pressure pain parameters using quantitative sensory testing at left and right shoulders at baseline and post-yoga (a) Pressure pain threshold (b) Pressure pain tolerance. Data are represented as mean ± standard deviation of the pressure in Kilopascals. *Depicts significance level (P < 0.05); Paired t-test was used in the statistical package for the social sciences software tool for the comparison between 2 time points. ns: Non-significant.
A significant increase in flexibility was seen by Schober’s test after yogic intervention (Baseline: 2.1 ± 0.8 cm and Post-yoga: 3.9 ± 1.3 cm; P < 0.05). Similar results were found when flexibility and range of motion were measured using Sit and Reach test post-yoga therapy, significant difference in the flexibility (Baseline: 13.7 ± 4.9 cm and Post-yoga: 19.7 ± 5.5 cm; P < 0.01) [Figure 6].
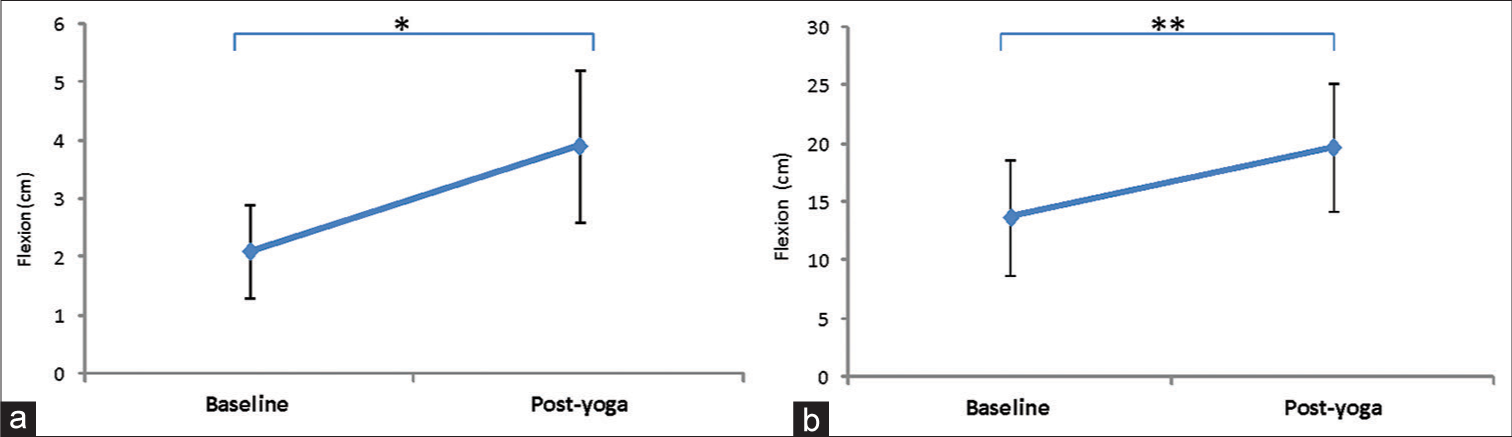
- Measurement of flexibility and range of motion using (a) Schober’s test and (b) Sit and reach test at baseline and post-yoga. Data are represented as mean ± standard deviation of lumbar flexion in centimetres. *Depicts significance level (P < 0.05); **Depicts significance level (P < 0.01). Paired t-test was used in the statistical package for the social sciences software tool for the comparison between 2 time points.
DISCUSSION
FM is a psychosomatic disease of the middle-aged population, predominantly women, with symptoms such as severe musculoskeletal pain along with morning stiffness, fatigue, anxiety, depression, and sleep problems. Specific tender points are present at 19 locations on the body surface from neck to toe in the patients.[3] Hyperalgesia and allodynia in FM patients have been shown to result from an increased sensitivity in central pain modulation mechanisms, referred to as central sensitisation.[12] Descending pain-inhibiting pathways from the brain stem, utilising neurotransmitters, has also been shown to be deficient in patients with chronic pain. This reduced inhibition of pain in combination with the increased input of pain signals is considered to cause sensitivity to touch, i.e., tenderness at specific sites in the patients.[12-14] Studies show that the tenderness at the peculiar tender points is due to allodynia and hyperalgesia associated with peripheral and central sensitisation of patients due to intense nociception.[15]
Yoga is a non-invasive lifestyle management strategy for many chronic pain conditions. In our previous study, Arya et al. have shown that regular yoga therapy relieves chronic low back pain and stress and improves quality of life better than the standard care.[16] Some of the tender points in the FM patients coincide with the pain sites of chronic low back pain patients. 20 sessions of supervised yoga therapy were administered to FM patients (n = 18); VAS score = 7.05 ± 0.8.
FM pain is severe pain (VAS score ranges from 5 to 8) when compared to other chronic pain conditions;[17,18] Pain catastrophising is also very significant due to other related symptoms which, thus, correlates with poor quality of life in patients.[19] FM patients have shown a significant reduction in the tender point counts, VAS score, and PCS score of the FM patients after the yoga therapy; similar results were found in other studies too.[6,20-23] Pressure pain parameters (both threshold and tolerance) are generally lower in FM patients when compared to healthy controls due to central sensitisation. A site-specific analysis revealed the lowest PPTs being localised at the trapezius muscle region, anterior cervical area, and the region around the second rib.[24,25] PPTs were significantly lower in healthy females than in healthy males (P < 0.01).[24] Regular 4 weeks of yoga therapy can improve PPT and pressure pain tolerance parameters at left and right shoulders, respectively. We reported that yoga-based regimens could modulate the PPTs of FM patients, which has been reported by other studies as well.[22] Objective evidence for the modulation of pain sensitivity, more specifically hyperalgesia and allodynia in FM patients after yoga therapy is one of the vital novelties of our study; as all other available kinds of literature cover mostly subjective parameters for pain status. We have assessed pain by QST and flexibility parameters using Schober’s test and Sit and Reach test which have not been reported earlier after yoga therapy sessions in FM patients.
A significant improvement in flexibility and range of motion in FM patients after 20 sessions of supervised yoga therapy was noted. Yoga not only modulates our minds but also increases the musculoskeletal activity of patients. Objective evidence that medical yoga therapy relieves chronic low back pain and stress and improves the quality of life better than standard care was recently explored.[16] Moreover, chronic low back pain patients have restricted movement along their lumbar axis; yoga can enhance the flexibility and range of movement.[16] Chronic pain leads to cortical plasticity due to alteration in the corticomotor excitability of the patients, which is further because of continuous inhibition of the movement of painful areas of the body. Yoga improves the corticomotor pathway and consequently modulates musculoskeletal activity by modulating pain inhibition pathways.[16,26,27]
Considering the impact of age-old yogic methods on human health and fitness, it is suggested that yoga is beneficial for many diseases and disabilities. However, to date, only a few studies are available that have objectively assessed the effect of yoga-based therapy in FM patients; In the present preliminary study, we have assessed the pain status and musculoskeletal activity of FM patients both subjectively and objectively. The study could be implemented in a larger number of patients and the assessment parameters can be compared with healthy controls for objective evidence of beneficial effects of yoga. Group activities are better for patient compliance and prevention of lost-to-follow-up (40%). We suggest that yoga therapy could be beneficial for the management of FM syndrome.
CONCLUSION
A 20-session long regular yoga regimen can provide pain relief and improve flexibility and range of motion in the Indian cohort of FM patients. Yoga therapy can be implemented on a day-to-day basis for the management of FM pain and its related symptoms.
Limitations and future perspectives
The present study is a preliminary attempt to investigate the effect of 4 weeks of regular yoga therapy on subjective and objective parameters of pain experience and flexibility parameters. We have chosen a cohort of both genders but the disease is more common in females. More studies with larger sample sizes can be designed with objective parameters to support the role of yoga therapy in such disorders.
Availability of data and materials
None of the individual’s data has been disclosed in the study. Datasets can be made available on special requests.
Acknowledgements
We would like to acknowledge all the participants of our study for their valuable cooperation. Our sincere acknowledgment to all the members of Pain Research and TMS Laboratory and Department of Physiology, AIIMS New Delhi, India. We thank Ms. Shikha Prajapat and Ms. Varsha for delivering yoga therapy sessions to the patients.
Ethical approval
The author(s) declare that they have taken the ethical approval by the Institute Ethics Committee, All India Institute of Medical Sciences, New Delhi, India (Ethical Approval No. IECPG-611/28.10.2021).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
DST SATYAM.
References
- The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken). 2010;62:600-10.
- [CrossRef] [PubMed] [Google Scholar]
- Fibromyalgia: Pathogenesis, mechanisms, diagnosis and treatment options update. Int J Mol Sci. 2021;22:3891.
- [CrossRef] [PubMed] [Google Scholar]
- 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum. 2016;46:319-29.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38:19-28.
- [CrossRef] [PubMed] [Google Scholar]
- Repetitive transcranial magnetic stimulation of the prefrontal cortex for fibromyalgia syndrome: A randomised controlled trial with 6-months follow up. Adv Rheumatol. 2020;60:34.
- [CrossRef] [PubMed] [Google Scholar]
- A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain. 2010;151:530-9.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized trial of tai chi for fibromyalgia. N Engl J Med. 2010;363:743-54.
- [CrossRef] [PubMed] [Google Scholar]
- Resistance exercise training for fibromyalgia. Cochrane Database Syst Rev. 2013;2013:CD010884.
- [CrossRef] [Google Scholar]
- EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76:318-28.
- [CrossRef] [PubMed] [Google Scholar]
- Bishop SR, Pivik J. The pain catastrophizing scale: Development and validation. Psychol Assess. 1995;7:524-32.
- [CrossRef] [Google Scholar]
- Assessment of the flexibility of the lumbar spine. A pilot study in children and adolescents. Scand J Rheumatol. 1973;2:87-91.
- [CrossRef] [PubMed] [Google Scholar]
- Endogenous opioidergic dysregulation of pain in fibromyalgia: A PET and fMRI study. Pain. 2016;157:2217-25.
- [CrossRef] [PubMed] [Google Scholar]
- Potency of descending pain modulatory system is linked with peripheral sensory dysfunction in fibromyalgia: An exploratory study. Medicine (Baltimore). 2019;98:e13477.
- [CrossRef] [PubMed] [Google Scholar]
- The relation between tender points and fibromyalgia symptom variables: Evidence that fibromyalgia is not a discrete disorder in the clinic. Ann Rheum Dis. 1997;56:268-71.
- [CrossRef] [PubMed] [Google Scholar]
- Objective evidence for chronic back pain relief by Medical Yoga therapy. Front Pain Res (Lausanne). 2022;3:1060685.
- [CrossRef] [PubMed] [Google Scholar]
- The American college of rheumatology 1990 criteria for the classification of fibromyalgia. Report of the multicenter criteria committee. Arthritis Rheum. 1990;33:160-72.
- [CrossRef] [PubMed] [Google Scholar]
- The comparison of the biological rhythms of patients with fibromyalgia syndrome with biological rhythms of healthy controls. Med Sci Monit. 2020;26:e920462.
- [CrossRef] [Google Scholar]
- The role of pain catastrophizing and anxiety levels on quality of life in fibromyalgia compared with healthy women. Intern Med. 2019;9:313.
- [CrossRef] [Google Scholar]
- Follow-up of yoga of awareness for fibromyalgia: Results at 3 months and replication in the wait-list group. Clin J Pain. 2012;28:804-13.
- [CrossRef] [PubMed] [Google Scholar]
- An 8-week yoga intervention is associated with improvements in pain, psychological functioning and mindfulness, and changes in cortisol levels in women with fibromyalgia. J Pain Res. 2011;4:189-201.
- [CrossRef] [PubMed] [Google Scholar]
- Mindful Yoga pilot study shows modulation of abnormal pain processing in fibromyalgia patients. Int J Yoga Therap. 2016;26:93-100.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of a daily yoga program for women with fibromyalgia. Int J Yoga. 2019;12:206-17.
- [CrossRef] [PubMed] [Google Scholar]
- Pressure pain thresholds of tender point sites in patients with fibromyalgia and in healthy controls. Eur J Pain. 2004;8:111-7.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between fibromyalgia and pressure pain threshold in patients with dyspareunia. Pain Res Manag. 2015;20:137-40.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of yoga on cortical inhibition in healthy individuals: A pilot study using Transcranial Magnetic Stimulation. Brain Stimul. 2018;11:1401-3.
- [CrossRef] [PubMed] [Google Scholar]
- Advancement in non pharmacological treatment strategies for the management of fibromyalgia syndrome. Int J Sci Res. 2023;12:5-8.
- [Google Scholar]
ANNEXURE
| Standing postures | Tadasana, Ardh Chakarasana, Samkonasana, etc. |
| Sitting postures | Shithil Dandasana, Ardh Ushtrasana, Shashankasana, etc. |
| Prone postures | Makarasana, Bhujungasana, Shalabhasana, etc. |
| Supine postures | Supt-pawanmutasana, Viparitakarani, Setubandhasana, etc. |
| Relaxation postures | Shavasana |
SUPPLEMENTARY FIGURES

- Algomed device for quantitative sensory testing.
- Sit and reach the box.







