Translate this page into:
Is clindamycin-modified triple antibiotic paste better than iodoform-based medicament for the treatment of non-vital primary molars using LSTR technique – A randomised clinical trial
*Corresponding author: Neetika Verma, Department of Pediatric and Preventive Dentistry, Faculty of Dental Sciences, SGT Dental College, SGT University, Gurugram, Haryana, India. neetikav95.nv@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Verma N, Gupta A, Garg S, Arya V, Dogra S, Dhankar M. Is clindamycin-modified triple antibiotic paste better than iodoform-based medicament for the treatment of non-vital primary molars using LSTR technique – A randomised clinical trial. Indian J Physiol Pharmacol 2022;66:276-85.
Abstract
Objectives:
The objectives of this study were to evaluate and compare the success rate of local application of iodoform-based obturating material (Pulpotec – [Produits Dentaires S.A., Switzerland]) and clindamycin-modified triple antibiotic paste (ClinM-TAP) in pulp chamber using minimally invasive endodontic treatment of carious primary molars indicated for pulpectomy, for 12 months, using clinical and radiographic parameters.
Materials and Methods:
A randomised clinical trial was conducted in 60 children in the age group of 3–8 years reporting carious primary molars with symptoms of irreversible pulpitis and pulpal involvement clinically, allocated into Group 1 (30) and Group 2 (30). In Group 1, Lesion sterilisation and tissue repair (LSTR) was done using Pulpotec (Produits Dentaires S.A., Switzerland) as medicament and in Group 2, ClinM-TAP (Clindamycin-modified triple antibiotic paste) was used as medicament. Clinical follow-up was done at 3, 6 and 12 months; radiographic follow-up was done at 6 and 12 months. Clinical parameters compared were tenderness on percussion, spontaneous pain, intraoral swelling and sinus/fistula. Radiographic comparison was done based on furcation radiolucency, root resorption and bone regeneration. Both intergroup and intragroup statistical analysis was done using Chi-square test or Fisher exact test, Cochran’s Q Test and Mann–Whitney U-Test for the test of significance. All the statistical tests were performed at 5% significance level.
Results:
The mean age of patients in the study was 5.25 ± 1.3years with 45% males and 55% females. Both groups showed significant improvement in terms of clinical symptoms from baseline to 12 months. On intergroup comparison clinical parameters, TOP was present in 11.2% and 44% of cases at the end of 12 months in Groups 1 and 2, respectively (P < 0 0.05). On intergroup comparison of radiographic parameters, at the end of 12 months, furcation radiolucency was seen in 32% and 73% (P < 0.05) and root resorption was seen in 16% and 30% cases in Group 1 and 2, respectively (P > 0.05). Overall clinical success rate of Group 1 and Group 2 was 88% and 50%, respectively (P < 0.05) and radiographic success rate was 60% and 27%, respectively (P < 0.05).
Conclusion:
LSTR using Pulpotec as a medicament has shown promising results in the present study. It could be a better alternative to conventional endodontic treatment in primary teeth. In the present study, ClinM-TAP has shown poor radiographic success; hence, it should be used with caution.
Keywords
Pulpectomy
Primary teeth
Iodoform
Antibiotics
INTRODUCTION
Dental caries, the most common childhood disease, has a significant impact on public health and economic status globally. A carious primary tooth involving the pulp with periradicular pathology, at times, might not respond favourably to the conventional endodontic therapy.
The typical tortuous root canal morphology of a primary tooth, ramifications and presence of numerous accessory canals compromise the outcome of conventional pulpectomy procedure.[1,2] Extrusion of the obturating material or failure of its resorption leads to irritation of the dental follicle and might lead to ectopic eruption of the successor tooth (20% incidence of palatal eruption/cross-bite) or arrest of the permanent tooth germ. Furthermore, reports have shown that private practitioners prefer extraction of an infected primary tooth over pulpectomy due to difficulty and time required to perform the procedure.[3-5]
A new approach that is less invasive and time efficient could be a better alternative for the paediatric patients as well as the clinician. Lesion sterilisation and tissue repair (LSTR) therapy, proposed by Hoshino[6] allows disinfection of dentinal, pulpal and peri-radicular lesions using placement of a medicament. Moreover, repair by natural defense mechanisms of host is anticipated.[2,6] According to a systematic review, there is no difference in the success rate of LSTR as compared to pulpectomy for the treatment of pulpally involved primary teeth. Whereas some studies have shown that LSTR is better than pulpectomy in teeth with pre-operative root resorption, pulpectomy results were better if roots were intact.[7]
Most commonly, a combination of three broad-spectrum antibiotics, namely, ciprofloxacin, metronidazole and minocycline, known as triple antibiotic paste (TAP), is used for root canal disinfection. Metronidazole acts against obligate anaerobes, which are the most commonly isolated species from infected root canals. Minocycline is a bacteriostatic long-acting antibiotic, potent against a wide range of microorganisms. Ciprofloxacin is added to eradicate Gram-negative species.[8,9]
The previous studies have shown that minocycline results in tooth discoloration. In the present study, clindamycin is chosen to replace minocycline, as it is effective against a wide variety of Gram-positive and Gram-negative anaerobes. When compared to other alternatives, it has fewer side effects and drug interactions and has a longer half-life (2.5 h for Clindamycin, 1.5 h for Erythromycin and 30 min for Amoxicillin).[8,10]
Pulpotec is an iodoform-based radiopaque, non-resorbable filling paste, composed of powder containing iodoform, polyoxymethylene, zinc and liquid containing formaldehyde, dexamethasone acetate, phenol, guaiacol and subsidiary substances. Pulpotec has antiseptic, antibacterial and anti-inflammatory properties. The main component of this paste is iodoform and due to its antiseptic properties, it acts like an antibiotic paste at the root canal orifices. Steroids act as an anti-inflammatory agent and have been shown to manage acute apical symptoms.[11]
There is paucity of the literature regarding the use of this simplified technique and its clinical efficacy. Hypothesis of this study is, LSTR using Pulpotec can be a good alternative to clindamycin-modified triple antibiotic paste (ClinMTAP). The objective of this study is to evaluate and compare the success rate of local application of clindamycin-modified TAP and Pulpotec using LSTR in the primary molars with carious pulpal involvement.
MATERIALS AND METHODS
Study design
The present study was a double blinded randomised parallel clinical trial conducted from August 2020 to August 2021 in the Department of Paediatric and Preventive Dentistry, SGT University, Gurgaon. Ethical clearance was obtained from the Institutional Review Board and was registered prospectively under the Clinical trials registry (CTRI/2020/06/026054).
During 3 months, children in the age group of 3 to 8 years reporting to the department with carious primary molars were screened for symptoms of irreversible pulpitis and pulpal involvement clinically, and those fulfilling the inclusion criteria were taken in the study.
Inclusion criteria
The following criteria were included in the study:
Age group – 3–8 years
Pulpally involved teeth indicated for pulpectomy
Restorable teeth.
Exclusion criteria
The following criteria were excluded from the study:
Patient with history of antibiotic allergy
Patient with any systemic disease
Cystic lesion
Radiographic signs of excessive internal or external resorption
Physiologic root resorption more than 1/3rd of the root length
Pulpal floor perforation.
Sample size estimation
The sample size was estimated to be 42 using G-Power software, where power of study was kept 0.80 and effect size was 0.80. A total of 95 patients were screened, out of which 60 were included in the study to compensate the sample attrition.
Randomisation
All participants were randomised into two groups using a simple randomisation technique. Random numbers were computer generated using Microsoft Excel (two sets of 30 each) by the study statistician. The random number indicating intervention or control was kept in a sealed envelope and the serial number of the participants was written on the top of the envelope. The envelope was opened by the research assistant who then assigned the participants to their respective arms.
Group 1: Pulpotec
Group 2: ClinM-TAP.
Blinding
The study was planned as double blind with a follow-up of 12 months. All the procedures were performed by the principal investigator and patients were evaluated by another blinded investigator (who was unaware of the interventions) during the follow-up visits.
Preparation of TAP
Chemotherapeutic agents to be used are – metronidazole (400 mg), ciprofloxacin (200 mg) and clindamycin (300 mg).
Antibiotic powder comprising ciprofloxacin 14%, metronidazole 43% and clindamycin 43% was prepared. To prepare a 1 mg/mL solution of ClinM-TAP, 100 mg of powder mentioned above was dissolved in 100 mL of sterile water. To obtain a homogenous gel of 1mg/ml, 8 g of methylcellulose powder was added to 100 ml of solution under magnetic stirring for 2 h (Prather BT et al. 2014)[12].
Clinical procedure
Pre-operative periapical radiograph of the selected tooth was taken [Figure 1a]. Anaesthesia for the tooth to be treated was achieved using (2%) lidocaine hydrochloride with adrenaline (1:80,000). After rubber dam application [Figure 1b], access opening was done using a no. 4 round bur. Necrotic pulp was removed thoroughly with a sharp spoon excavator and root canal entry was localised using an explorer [Figure 1c]. Working length was estimated by intraoral periapical X-rays and fixed at -1 mm from the radiographic apex (American Academy of Paediatric Dentistry, 2009) [Figure 1d]. Removal of pulpal debris from the root canals was done using H files and copious irrigation with 1% sodium hypochlorite followed by saline irrigation. Pulp chamber and canals were dried using cotton pellets and paper points. Walls of the access cavity were cleaned with 15% EDTA to improve the patency of dentinal tubules. Group 1, Pulpotec and Group 2, ClinM-TAP were placed on the floor of the pulp chamber and pressed with a damp cotton pellet [Figure 1e]. The cavity was filled with IRM [Figure 1f]. SS crown was given after 1 week if clinical signs and symptoms got resolved [Figures 1g and h].

- Clinical procedure (a) pre-operative radiograph, (b) rubber dam application, (c) access cavity preparation, (d) working length estimation and pulp extirpation, (e) placement of medicament, (f) IRM placement, (g) SS crown placement and (h) post-operative radiograph.
Clinical and radiographic follow-up
Patients were followed clinically at 3 months, 6 months and 12 months. Radiographic follow-up was done at 6 months and 12 months [Figures 2 and 3].

- Radiographic follow-up of Group 1, (a) pre-operative radiograph, (b) post-operative radiograph, (c) radiograph at 6 months follow-up and (d) radiograph at 12 months follow-up.

- Radiographic follow-up of Group 2, (a) pre-operative radiograph, (b) post-operative radiograph, (c) radiograph at 6 months follow-up and (d) radiograph at 12 month follow-up.
Statistical analysis
The data collected were entered into Microsoft Excel and then transferred to SPSS version 20. Descriptive and inferential statistics were done. Demographic data were described using descriptive methods. Categorical data were presented in the form of proportion. Both intergroup and intragroup statistical analysis was done using Chi-square test or Fisher exact test, Cochran’s Q Test and Mann–Whitney U-Test for the test of significance. All the statistical tests were performed at 5% significance level.
RESULTS
In the present study, 60 children in the age group of 3–8 years were selected according to inclusion criteria after screening 95 patients. These patients were randomly allocated into Group 1 (30) and Group 2(30). At the end of 12 months, 26 and 25 patients were left and analysed in Groups 1 and 2, respectively [Figure 4]. The mean age of patients in this study was 5.25 ± 1.3 years, out of which 45% were male and 55% were female.

- Consort diagram.
[Table 1] represents comparison of clinical parameters between and within the two groups. There was no significant intergroup difference at 3, 6 and 12 months in cases showing presence of TOP, spontaneous pain and intraoral swelling (P > 0.05). However, significant increase in number of cases showing presence of sinus/fistula was seen in Group 2 when compared to Group 1 at 3 month follow-up (P < 0.05). The intragroup comparison showed significantly better results at 3, 6 and 12 months in terms of all the clinical parameters except for presence of increased number of cases with sinus/fistula in Group 2 at 3 months (P < 0.05). On comparing overall success rate at the end of 12 months, Group 2 showed significantly lower success rate than Group 1 in terms of absence of TOP [Table 1, Figures 5 and 6].
| Clinical parameters | Group 1 (Pulpotec) n(%) | Group 2 (ClinM-TAP) n(%) | P-value |
|---|---|---|---|
| Tender on percussion | |||
| Baseline | 9 (36.0) | 18 (69.2) | 0.02 |
| At 3 months | 2 (8.0) | 7 (26.9) | 0.14 |
| At 6 months | - | 2 (11.8) | 0.09 |
| At 12 months | 1 (4.3) | 2 (15.4) | 0.31 |
| P value | 0.00 | 0.00 | |
| Overall Success | 88.8% | 56% | 0.05 |
| Spontaneous pain | |||
| Baseline | 18 (72.0) | 11 (42.3) | 0.03 |
| At 3 months | 2 (8.0) | 2 (7.7) | 1.00 |
| At 6 months | - | - | - |
| At 12 months | - | - | - |
| P value | 0.00 | 0.00 | |
| Overall success | 92% | 92% | 1.00 |
| Intraoral swelling | |||
| Baseline | 2 (8) | 7 (26.9) | 0.14 |
| At 3 months | - | - | - |
| At 6 months | - | - | - |
| At 12 months | - | - | - |
| P value | 0.00 | 0.00 | |
| Overall success | 100% | 100% | 1.00 |
| Sinus/fistula | |||
| Baseline | 5 (20) | 2 (7.7) | 0.24 |
| At 3 months | - | 5 (19.2) | 0.02 |
| At 6 months | - | - | - |
| At 12 months | - | - | - |
| P value | 0.004 | 0.002 | |
| Overall success | 100% | 80% | 0.1 |
| Chi-square/Fisher exact test/Cochran’s Test |
ClinM-TAP: Clindamycin-modified triple antibiotic paste
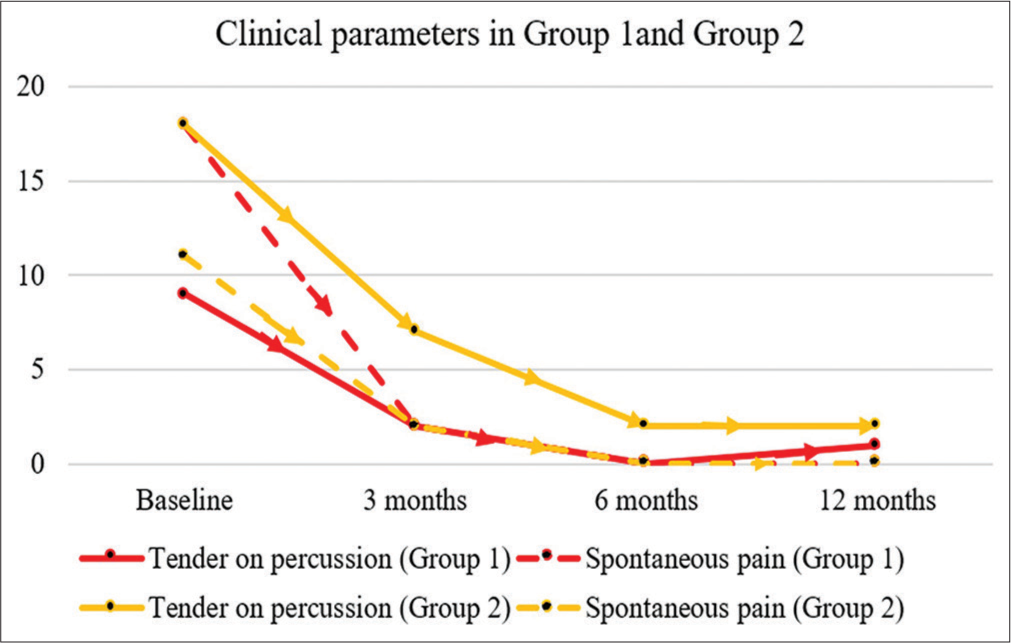
- Line diagram representing clinical parameters in Group 1 and Group 2 at baseline, 3 months, 6 months and 12 months.
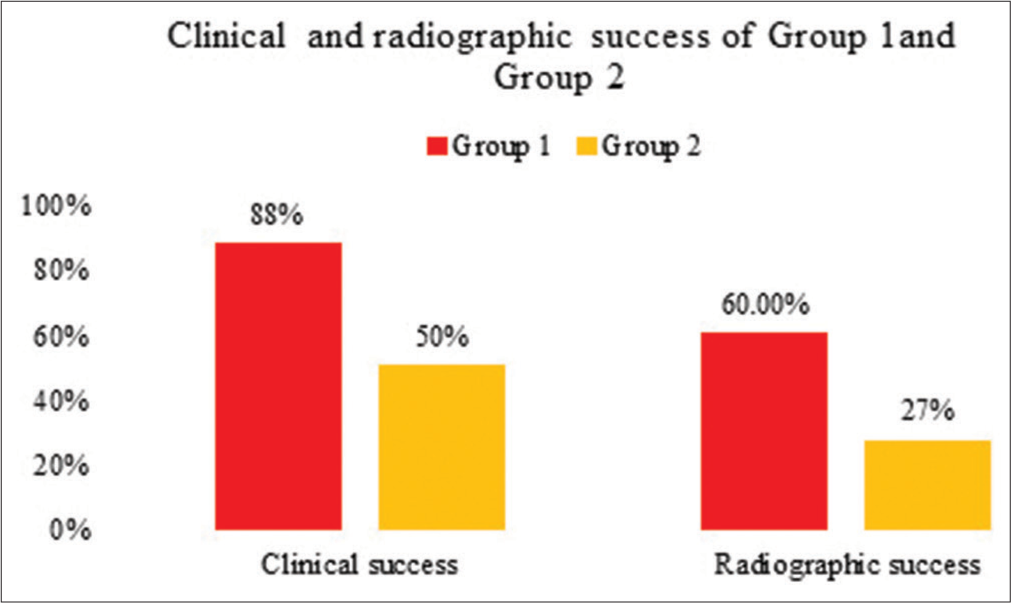
- Graphical representation of clinical and radiographic success rate in Group 1 and Group 2.
Radiographic parameters of Group 1 and 2 are described below:
Root resorption
Group 2 showed significantly higher number of cases showing root resorption compared to Group 1 at 6 month and 12 month interval (P < 0.05). A significant number of teeth showed increase in root resorption within Group 2 at 6 month and 12 months interval (P < 0.05). Teeth with carious involvement on mesial site showed significant relation with mesial root resorption (P < 0.05) [Table 2 and Figure 7].
| Radiographical parameters | Group 1 (Pulpotec) n(%) | Group 2 (ClinM-TAP) n(%) | P-value |
|---|---|---|---|
| Root Resorption | |||
| At baseline | 0 | 0 | - |
| At 6 months | 4 (17.4) | 8 (47) | 0.04 |
| At 12 months | 4 (17.4) | 8 (53) | 0.05 |
| P value | 2.30 | 0.00 | |
| Overall success | 84% | 70% | 1.00 |
| Furcation radiolucency | |||
| At baseline | |||
| Absent | 22 (88.0) | 24 (92.3) | 0.67 |
| Present | 3 (12.0) | 2 (7.7) | |
| At 6 months | |||
| Favourable | 19 (82.6) | 7 (41.2) | 0.03 |
| Unfavourable | 4 (17.4) | 10 (58.8) | |
| At 12 months | |||
| Favourable | 17 (74) | 7 (46.66) | 0.01 |
| Unfavourable | 6 (26) | 8 (53.33) | |
| P value | 0.00 | 0.00 | |
| Overall success | 68% | 27% | 0.00 |
| Bone regeneration | |||
| At baseline | - | - | - |
| At 6 months | 2 (8.7) | - | - |
| At 12 months | 2 (8.7) | - | - |
| Chi-square/Fisher exact test/Mann–Whitney U-Test | |||
| Site of exposure (Number of teeth) | Site of resorption | ||
| Mesial | Distal | Palatal | |
| Mesial (14) | 4 (28.6) | 0 | 0.04 |
| Distal (27) | 7 (26) | 5 (18.5) | 0.37 |
| Occlusal (10) | 1 | 0 | 0.63 |
Fisher exact test/Chi-square test, TAP: Triple antibiotic paste, ClinM-TAP: Clindamycin-modified triple antibiotic paste
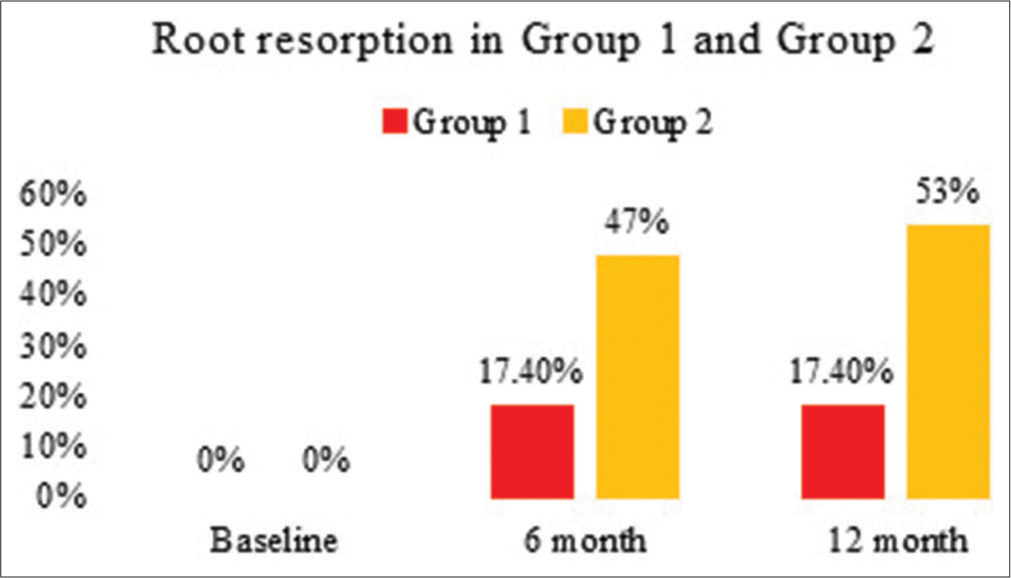
- Graphical representation of cases showing root resorption in Group 1 and Group 2.
Furcation radiolucency
In teeth showing furcation radiolucency, the result was depicted as favourable (absent, decreased or static) and unfavourable (increased). There was no significant intergroup difference at the baseline. At 6 and 12 months interval, Group 1 showed significantly higher number of cases with favourable outcome compared to Group 2 (P < 0.05). There was significant increase in unfavourable outcomes in Group 2 at 6 and 12 month intervals (P < 0.05) [Table 2 and Figure 8].

- Graphical representing of cases showing furcation radiolucency in Group 1 and Group 2.
Bone regeneration
It was observed in two cases in Group 1 at 6 month and 12 month interval [Figure 9].

- Reduction in furcation radiolucency and bone regeneration seen in Group 1, (a) pre-operative radiograph, (b) radiograph at 6 month follow-up and (c) radiograph at 9 month follow-up, (d) radiograph at 12 month follow-up.
Similarly, on comparing the radiographic parameters, significantly lower success rate was observed in Group 2 in terms of absence/decrease in furcation radiolucency.
At 12 months follow-up, clinical success rate of Group 1 and Group 2 was 88% and 50%, respectively (P < 0.05) and radiographic success rate was 60% and 27%, respectively (P < 0.05) [Table 2 and Figure 6].
Patients who presented with clinical signs and symptoms at follow-up visits were treated using pulpectomy followed by obturation with metapex.
DISCUSSION
The present study examined the clinical and radiographic success rate of LSTR using Pulpotec and ClinM-TAP in pulpally involved primary molars. LSTR is easier and quicker to perform, and has been suggested as a potential alternative to replace pulpectomy as it does not require multiple visits to be completed, even for teeth with periapical lesions.[1]
Various studies have been conducted over the years using different techniques and medicaments to find out clinical and radiographic success of LSTR technique in deeply carious primary molars with signs and symptoms of pulpal involvement. Prabhakar et al. (2008)[13] in a study evaluated that the success rate of LSTR was 83% in teeth, in which radicular pulp was removed when compared to the teeth without radicular pulp removal (37%). Hence, in the present study, LSTR with removal of radicular pulp was performed in teeth with signs of irreversible pulpitis or non-vital teeth with/without furcation radiolucency.
Several studies have confirmed the efficacy of TAP in LSTR. However, the addition of minocycline causes certain complications such as primary tooth discoloration and discoloration of underlying permanent successor (Rafatjou et al. 2018),[8] demineralisation of radicular dentin and weakening of root structure. In a recent in vitro study conducted by Karczewski et al. (2018)[10] to assess cytotoxicity, antimicrobial efficacy and dentin discoloration of ClinM-TAP, it was concluded that clindamycin could serve as a viable alternative to minocycline in TAP.
In the present study, 1 mg/ml concentration of ClinM-TAP was used in Group 2. According to Algarni et al. (2015),[14] antibiotic paste at a concentration of 1 mg/mL had sufficient antimicrobial action against the most resistant endodontic pathogen – E. faecalis.
Pulpotec is an iodoform-based radio-opaque, non-resorbable material available in the form of powder and liquid. The paste sets quickly after mixing, providing ideal conditions for restoration. It has shown successful results as a pulp medicament for pulpotomy in the primary and permanent teeth as well as intracanal dressing for permanent teeth.[15] Aboujaoude et al. (2015)[16] conducted a study to evaluate the effectiveness of Pulpotec on the primary molars with necrotic pulp and furcation bone loss. In this study, 67.7% of patients showed healing in furcation area. Hence, this technique can be used for treatment of deciduous necrotic teeth. There is lack of sufficient evidence regarding its use in pulpally involved primary teeth requiring pulpectomy. Therefore, in Group 1, we used Pulpotec in the primary molars treated using LSTR.
In the present study, all the teeth included in Group 1 and Group 2 showed clinical signs and symptoms at the baseline indicating the requirement for pulpectomy. On intragroup comparison, Group 1 showed significant clinical success rate of 92%, 100% and 95.7% at 3, 6 and 12 months, respectively, with an overall clinical success rate of 88% at the end of 12 month period. Aboujaoude et al. (2015)[16] reported clinical success rate of 100% for 12 months in necrotic primary teeth treated with Pulpotec after complete pulp extirpation. Agarwal et al. (2011),[17] in a study, used Pulpotec as a medicament in pulpotomised teeth. The clinical success rate at 3 month, 6 month and 12 month was 94%, 95.7% and 95.7%, respectively, which was similar to the results obtained in the present study. Similar results were obtained in the studies conducted by Sunitha et al. (2017),[15] Verma et al. (2019)[18] for using Pulpotec as a pulpotomy agent in the primary molars.
Radiographic evaluation in Group 1 revealed four cases (17.4%) with pathologic root resorption at 6 months follow-up (P > 0.05). This may be attributed to diagnostic errors, or technical failure while performing the treatment chosen. Furcation radiolucency was observed in three cases at the baseline, out of which two showed signs of bone regeneration. A total of 16 cases (60%) showed absence of furcation radiolucency at the end of 12 months. The overall radiographic success rate was 60% at the end of 12 month period. Aboujaoude et al. (2015)[16] showed radiographic success rate of 67%, similar to the present study. Radiographic success rate of Pulpotec reported in pulpotomised teeth ranges from 80% to 100% (Sunitha et al. (2017),[15] Verma et al. (2019)[18]) which is slightly higher than the present study. This could be due to the difference in case inclusion criteria as in our study teeth showing signs of pulpal and periapical involvement requiring pulpectomy were selected.
Intragroup comparison in Group 2 revealed clinical success of 73.2%, 88.2% and 84.6% at 3 months, 6 months and 12 month follow-up, respectively, with overall success rate of 50% at the end of 12-month period. In a 3-month clinical trial in the primary molars, Shankar et al. (2021)[19] compared effectiveness of 1g/ml and 1mg/mL concentrations of TAP containing ciprofloxacin, metronidazole and clindamycin in LSTR. Clinical success rate of 1mg/ml TAP was 84.4% which was similar to the 3-month success rate in the present study. In a study conducted by Prabhakar et al. (2008),[13] radicular pulp removal was done followed by placement of conventional TAP. The clinical success rate of studies using conventional TAP with radicular pulp removal is reported to be around 80%–90% (Prabhakar et al. (2008),[13] Jaya et al. (2012),[20] Duanduan et al. (2013),[21] and Hossain et al. (2020)[22]) which does not support the results obtained in the present study.
Radiographic follow-up in Group 2 showed significant increase in number of cases showing root resorption (30%) and furcation radiolucency (53%) at the end of 12-month period. The overall radiographic success rate was 27%. Shankar et al. (2021)[19] also observed accelerated root resorption in teeth treated using methylcellulose-based ClinM-TAP within 3 months of treatment. These findings are not in accordance with the results obtained in other similar studies using conventional TAP, in which success rate is reported to be 60–100% (Jaya et al. (2012),[20] Duanduan et al. (2013),[21] and Hossain et al. (2020)[22]).
The poor success rate of ClinM-TAP used in the present study could be due to replacement of minocycline. Minocycline belongs to class of tetracycline, is bacteriostatic in nature and prevents release of endotoxins (Torabinejad et al. 2003).[23] These endotoxins may act as irritants and can lead to inflammatory root resorption. Tetracyclines inhibit mammalian collagenases and clastic cells, hence preventing tissue breakdown and anti-resorptive action (Mohammadi and Abbott. 2009).[24] On the other hand, in a study conducted by Naal et al. (2008),[25] they found that locally applied clindamycin significantly inhibited osteoblastic proliferation at the lowest concentration of 500 mg/ml. This could be the reason for poor bone healing in the furcation area in teeth treated with ClinM-TAP in Group 2. Another reason could be microleakage around GIC used directly over gel-based TAP as interim restoration for 1 week before SS crown placement. As in other studies, paste like consistency of TAP was used and it was sealed using resin-based restorations or restored immediately with SS crowns (Nakornchai et al. (2010)[26] and Raslan et al. (2017)[27]).
In the present study, 16% and 30% of cases in Group 1 and Group 2, respectively, showed pathologic root resorption. In this study, 28% of the cases showing mesial site of caries involvement showed only mesial root resorption (P < 0.05). This could be attributed to the fact that mesial pulp horns are higher and underwent early exposure and degenerative changes (Vieira-Andrade et al., 2012).[28] Histologic studies are needed to find the exact explanation for the higher rate of mesial root resorption in mesial side caries compared to distal and occlusal.
In the present study, the overall clinical and radiographic success rate of Group 1 was significantly better than that of Group 2. In both the groups, clinical success rate was more than radiographic success. This difference was significantly higher in Group 2. This was also observed in other studies using TAP in LSTR (Duanduan et al. (2013),[29] Hossain et al. (2020)[30] Doneria et al. (2017),[31] Grewal et al. (2018)[32]) [Table 3]. No radiographic pathology was associated with the primary or underlying permanent tooth germ.
| Authors | Material and method | Conclusion |
|---|---|---|
| Nakornchai et al. (2010)[26] | LSTR (TAP-1:1:1) versus Pulpectomy | Supports LSTR as an alternative to pulpectomy |
| Pinky et al. (2011)[9] | LSTR using TAP versus Ornidazole-modified TAP | Clinical success was more than radiographic success |
| Jaya et al. (2012)[20] | LSTR using TAP versus Tinidazole-modified TAP | Around 50–60% success rate in teeth with periradicular lesion |
| Aboujaoude et al.(2015)[16] | Pulpectomy+Pulpotec placed in chamber | Bone healing in necrotic primary molars presenting furcation bone lesion |
| Raslan et al. (2017)[27] | Group 1-TAP, Group 2 – Clindamycin-modified TAP | Supports clindamycin as an alternative to minocycline |
| Doneria et al. (2017)[31] | Group A – ZnO-OO, Group B-modified 3Mix-MP (Ornidazole, Cefaclor, Ciprofloxacin) paste, Group C-Vitapex | Modified 3Mix-MP antibiotic treatment can be a substitute of conventional root canal treatment in the primary molars |
| Grewal et al. (2018)[32] | LSTR (metronidazole, ciprofloxacin, cefaclor) versus. Pupectomy | LSTR for treatment of deciduous teeth with poor prognosis to maintain them for short duration |
| Rafatjou et al. (2019)[8] | In vitro study using TAP versus clindamycin-modified TAP | Clindamycin as an alternative to Minocycline in TAP |
| Coll et al. (2020)[7] | Systematic review and meta-analysis | Pulpectomy performed better in teeth without pre-operative resorption and LSTR better in teeth with root resorption |
| Shankar et al. (2021)[19] | Img/ml versus 1g/ml (ciprofloxacin, clindamycin, metronidazole) | Similar success rate in both groups |
LSTR: Lesion sterilisation and tissue repair, TAP: Triple antibiotic paste
Limitations
Due to COVID19, number of patients visiting the hospital decreased. Hence, we calculated the minimum possible sample size required for the study.
There was no calibrated method used for radiographic measurements.
Association of site of exposure and site of root resorption could have been done.
CONCLUSION
LSTR using pulpotec as a medicament has shown promising results in the present study. It could be a better alternative to conventional endodontic treatment in the primary teeth. In the present study, ClinM-TAP has shown poor radiographic success. More studies are required with larger sample size to check the efficacy of Pulpotec and to find out suitable components and concentrations of TAP for better clinical and radiographic outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Endodontic treatment of primary teeth using a combination of antibacterial drugs. Int Endod J. 2004;37:132-8.
- [CrossRef] [PubMed] [Google Scholar]
- Success rates of a mixture of ciprofloxacin, metronidazole, and minocycline antibiotics used in the non-instrumentation endodontic treatment of mandibular primary molars with carious pulpal involvement. Int J Paediatr Dent. 2012;22:217-27.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of pulpectomies using ZOE and KRI paste in primary molars: A retrospective study. Pediatr Dent. 1993;15:403-7.
- [Google Scholar]
- Ectopic eruption of permanent incisors after predecessor pulpectomy: Five cases. Gen Dent. 2011;59:e162-7.
- [Google Scholar]
- Predicting pulpectomy success and its relationship to exfoliation and succedaneous dentition. Pediatr Dent. 1996;18:57-63.
- [Google Scholar]
- Evaluation of the antimicrobial efficacy of two combinations of drugs on bacteria taken from infected primary teeth (in vitro) Eur Arch Paediatr Dent. 2019;20:609-15.
- [CrossRef] [PubMed] [Google Scholar]
- Endodontic treatment of necrosed primary teeth using two different combinations of antibacterial drugs: An in vivo study. J Indian Soc Pedod Prev Dent. 2011;29:121-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clindamycin-modified triple antibiotic nanofibers: A stain-free antimicrobial intracanal drug delivery system. J Endod. 2018;44:155-62.
- [CrossRef] [PubMed] [Google Scholar]
- Four years of clinical experience with the efficacy of Pulpotec® as a root canal dressing for the management and control of odontogenic pain: A prospective randomized clinical trial. Oral Health Dent Manag. 2013;12:279-83.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of two combinations of triple antibiotic paste used in endodontic regeneration on root microhardness and chemical structure of radicular dentine. J Oral Sci. 2014;56:245-51.
- [CrossRef] [PubMed] [Google Scholar]
- Endodontic treatment of primary teeth using combination of antibacterial drugs: An in vivo study. J Indian Soc Pedod Prev Dent. 2008;26:S5-10.
- [Google Scholar]
- Inhibitory effect of gels loaded with a low concentration of antibiotics against biofilm formation by Enterococcus faecalis and Porphyromonas gingivalis. J Oral Sci. 2015;57:213-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and radiographic evaluation of four different pulpotomy agents in primary molars: A longitudinal study. Int J Clin Pediatr Dent. 2017;10:240-4.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of a modified pulpotec endodontic approach on necrotic primary molars: A one-year follow-up. Eur J Paediatr Dent. 2015;16:111-4.
- [Google Scholar]
- A comparative evaluation of noninstrumentation endodontic techniques with conventional ZOE pulpectomy in primary molars: An in vivo study. World J Dent. 2011;2:187-92.
- [CrossRef] [Google Scholar]
- Comparative evaluation of success of pulpotomy in primary molars treated with formocresol, pulpotec and biodentine-6 month follow up study. Int J Appl Dent Sci. 2019;5:77-82.
- [Google Scholar]
- Comparison of modified triple antibiotic paste in two concentrations for lesion sterilization and tissue repair in primary molars: An in vivo interventional randomized clinical trial. Int J Clin Pediatr Dent. 2021;14:388-92.
- [CrossRef] [PubMed] [Google Scholar]
- In vivo evaluation of lesion sterilization and tissue repair in primary teeth pulp therapy using two antibiotic drug combinations. J Clin Pediatr Dent. 2012;37:189-91.
- [CrossRef] [PubMed] [Google Scholar]
- Retrospective study of pulpectomy with Vitapex and LSTR with three antibiotics combination (3mix) for non vital pulp treatment in primary teeth. CMU J Nat Sci. 2013;12:131-9.
- [CrossRef] [Google Scholar]
- Evaluation of LSTR 3 mix MP therapy for healing of periapical pathosis of nonvital teeth. TAJ J Teach Assoc. 2020;33:76-84.
- [CrossRef] [Google Scholar]
- The antimicrobial effect of MTAD: An in vitro investigation. J Endod. 2003;29:400-3.
- [CrossRef] [PubMed] [Google Scholar]
- On the local applications of antibiotics and antibiotic-based agents in endodontics and dental traumatology. Int Endod J. 2009;42:555-67.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of clindamycin on human osteoblasts in vitro. Arch Orthop Trauma Surg. 2008;128:317-23.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical evaluation of 3Mix and Vitapex as treatment options for pulpally involved primary molars. Int J Paediatr Dent. 2010;20:214-21.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of antibiotic mix in non-instrumentation endodontic treatment of necrotic primary molars. Eur J Paediatr Dent Dec. 2017;18:285-90.
- [Google Scholar]
- Inflammatory root resorption in primary molars: Prevalence and associated factors. Braz Oral Res. 2012;26:335-40.
- [CrossRef] [PubMed] [Google Scholar]
- Resorption as an inflammatory process. Approach to the pathogenesis of dental and periodontal resorption. RCOE. 2005;10:545-56.
- [CrossRef] [Google Scholar]
- Caries color, extent, and preoperative pain as predictors of pulp status in primary teeth. Clin Cosmet Investig Dent. 2020;12:263-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative evaluation of clinical and radiological success of zinc oxide-ozonated oil, modified 3Mix-MP antibiotic paste, and Vitapex as treatment options in primary molars requiring pulpectomy: An in vivo study. J Indian Soc Pedod Prev Dent. 2017;35:346-52.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of resorption rate of primary teeth treated with alternative lesion sterilisation and tissue repair and conventional endodontic treatment: An in vivo randomized clinical trial. J Indian Soc Pedod Prev Dent. 2018;36:262-7.
- [CrossRef] [PubMed] [Google Scholar]






