Regular moderate exercise effects on pro-inflammatory cytokines of diabetic rat’s retina and optic nerve
*Corresponding author: Farzam Sheikhzadeh, Department of Animal Biology, Faculty of Natural Sciences, University of Tabriz, Tabriz, Iran. Fsheikhzadeh@tabrizu.ac.ir
-
Received: ,
Accepted: ,
How to cite this article: Khajehnasiri N, Kosari-Nasab M, Hesari FS, Asadollahi L. Regular moderate exercise effects on pro-inflammatory cytokines of diabetic rat’s retina and optic nerve. Indian J Physiol Pharmacol 2021;65(1):45-50.
Abstract
Objectives:
Tissue levels of cytokines represent of inflammation and forewarning of injury. In diabetic patients, these factors increase notably but don’t designate source of them. Retinopathy is one of the complications of diabetes mellitus that probably generates by reason of inflammatory damage in micro vascular or in retinal cells. Exercise decreases blood sugar and diabetic injurious. Investigation of IL-1 and TNF-a in retina in diabetic model rats and exercise effects on them were purposed of this study.
Materials and Methods:
In this experimental study, 40 adult Wistar male rats (250 ± 50 g) were used. They were randomly divided into four groups (n = 10): (1) Sedentary control (SC) group, (2) sedentary diabetic (SD) group, (3) 8-week healthy exercised (8HE) group and (4) 8-week diabetic exercised (8DE) group. A week after induction of diabetes by injection of streptozotocin, 60 min treadmill exercise and 5 days a week with 22 (m/min) speeds were undertaken. All groups were evaluated in terms of retina and optic nerve tissue levels of TNF-α and IL-1 using ELISA.
Results:
Based on the results, TNF- α tissue levels were decreased in the 8HE and increased in the 8DE groups compared to control, respectively. Also, no difference was observed in IL-1 tissue levels between exercised and control groups.
Conclusion:
Long term exercise protocol was useful in healthy rats but don’t decrease of pro-inflammatory retinal complication in diabetes mellitus.
Keywords
Retinopathy
Diabetes mellitus
Tumour necrosis factor-α
Interleukin-1
INTRODUCTION
Diabetic retinopathy is well-known as one of the complications of vascular disease, which is considered as the most important causes of blindness in patients aged between 20 and 74 years old.[1] The previous studies have shown that the prevalence of retinopathy in diabetic patients is associated with the time of onset and duration of disease. Although, approximately 85–90% of diabetic patients are affected by retinopathy,[2] complications such as cataracts, glaucoma and neuropathy can be found in the patients’ eye.[3]
It has been documented that inflammatory factors play an important role in the development of diabetes mellitus.[4] A significant increase in the levels of inflammatory markers in serum has been considered to develop microvascular complications such as retinopathy in patients with diabetes. For example, inflammatory cytokines including abnormalities in the levels of tumour necrosis factor (TNF)-α[5] and interleukin (IL)-1[6] have been found in diabetic patients, showing that these factors may play a pivotal role in the pathogenesis of diabetes.
Indirect evidence indicated that TNF-α may be involved in the retinopathy by increasing the expression of genes associated with inflammatory-coagulation factors and adhesive molecules.[5,7] In addition, IL-1β has been shown to induce cell death in retinal capillaries in the presence of high glucose concentration, while blockade of this cytokine reduced these pathological parameters.[8] These findings are supported by studies showing that IL-1β antagonist and TNF-α inhibitor can decrease the development of retinal complications in diabetic patients.[9] Hence, the factors that can inhibit the release of IL-1β and TNF-α in diabetic patients may be a new therapeutic approach to prevent the development of retinopathy.[3] Recent studies have provided some evidence that regular exercise is able to reduce inflammation in humans and rodents. Moreover, regular exercise has been indicated to prevent the onset and development of the diabetic complications.[10] For example, our recent study showed that regular exercise by reducing the blood glucose levels declined the phosphorylation of the connexin-43 protein in the left ventricle[11] and retina[12] of Type 1 diabetic rats.
Considering the important role of inflammatory factors in the pathogenesis of diabetic vision complications and the efficacious role of regular exercise in reducing and controlling blood glucose levels, we aimed (along with the previous work[11]) to investigate the effect of exercise on inflammatory cytokines such as IL-1 and TNF-α in retinal and perineal tissues in diabetic rats.
MATERIALS AND METHODS
Animals
Forty adult male Wistar rats, weighing 250 ± 50 g, were obtained from the Department of Animal Breeding at the University of Tabriz. The temperature at the breeding environment was 22 ± 2°C and rats were kept at a 12:12 h light-dark cycle (7 am–7 pm) while having free access to food and water. All procedures for the maintenance and use of the experimental rats were conducted based on the guide for the care and use of laboratory animals (NIH Guide for Care and Use of Laboratory Animals, 8th Edition, 2010) and institutional animal care of Shahid Beheshti University of Medical Sciences.
Experimental groups
Animals were randomly divided into four groups (p = 10/group): (1) Sedentary control (SC) group, (2) 8-week healthy exercised (8HE) group, (3) sedentary diabetic (SD) group and (4) 8-week diabetic exercised (8 DE) group. The CONSORT diagram is shown in [Figure 1].
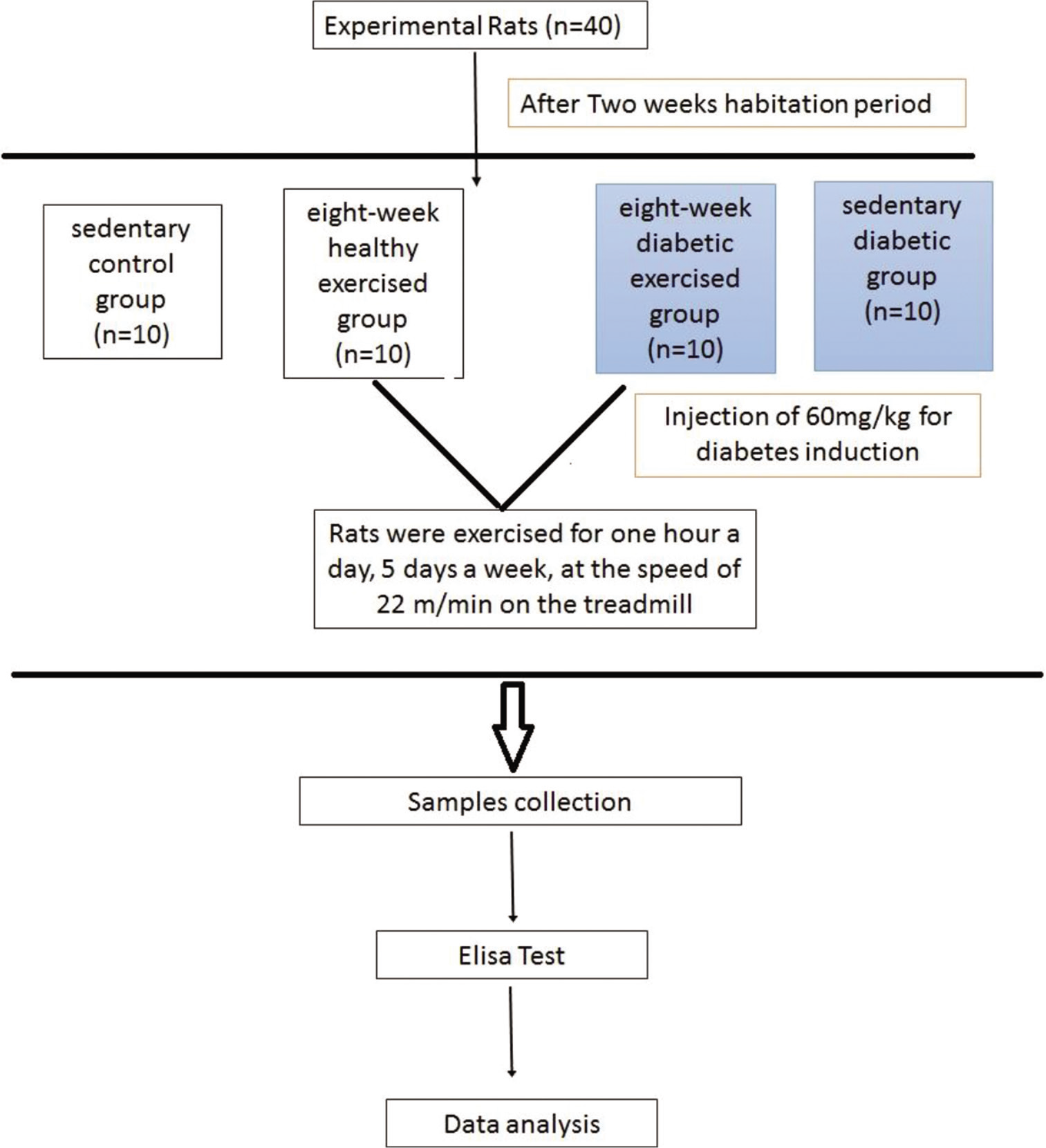
- Consort diagram of research.
Induction of diabetes
Diabetes was induced by an intraperitoneal injection of 60 mg/kg streptozotocin (Sigma Co.)[11] and dissolved in sterile saline. Control rats received only the vehicle.
Exercise protocol
Rats were exercised for 1 h a day, 5 days a week, at the speed of 22 m/min on the treadmill.[11] As a warm-up, the speed of the treadmill was increased from 5 m/min to 22 m/min within the initial 10 min. Furthermore, the speed was gently reduced to 5 m min in the past 10 min, to return them to the initial state. Control group rats were placed on the treadmill as long while the machine was off.
Sample collection
All rats were anesthetised by intraperitoneal injection of ketamine 100 mg/kg and xylazine 5 mg/kg 24 h after finishing the exercise protocol.[11] Eyes were enucleated, the retina and optic nerve were separated and immediately frozen in liquid nitrogen and transferred to the freezer (–80°C) for the measurement of TNF-α and IL-1 proteins.
ELISA
When samples were removed from the –80°C freezer, 600 μL of cold phosphate-buffered saline (ice cold 1%; –18°C) was added to each specimen. Then, homogenised tissue was prepared using a manual homogeniser. Then, the samples were centrifuged using a refrigerated centrifuge (4°C) at 5000 × g for 5 min, and eventually, their supernatant was removed instantly and TNF-α and IL-1 were measured using ELISA kit according to kit instructions.
Data analysis
Normality test was used to see whether the collected data on the TNF-α and IL-1 were normally distributed or not. Oneway ANOVA and the Tukey post hoc test were utilised to compare the difference between groups using SPSS statistical program (version 16). The mean ± SEM were reported in the text and p < 0.05 was considered as the level of significance.
RESULTS
Effect of exercise on IL-1 and TNF-α
As illustrated in [Figure 2], TNF-α level was significantly decreased in 8HE group (p < 0.05) when compared with SC. Moreover, 8-week exercise in diabetic rats resulted in a significant increase in the TNF-α level as compared to SC and SD groups (p < 0.05). However, there were no significant differences in IL-1 levels between experimental groups (p > 0.05) [Figure 3].
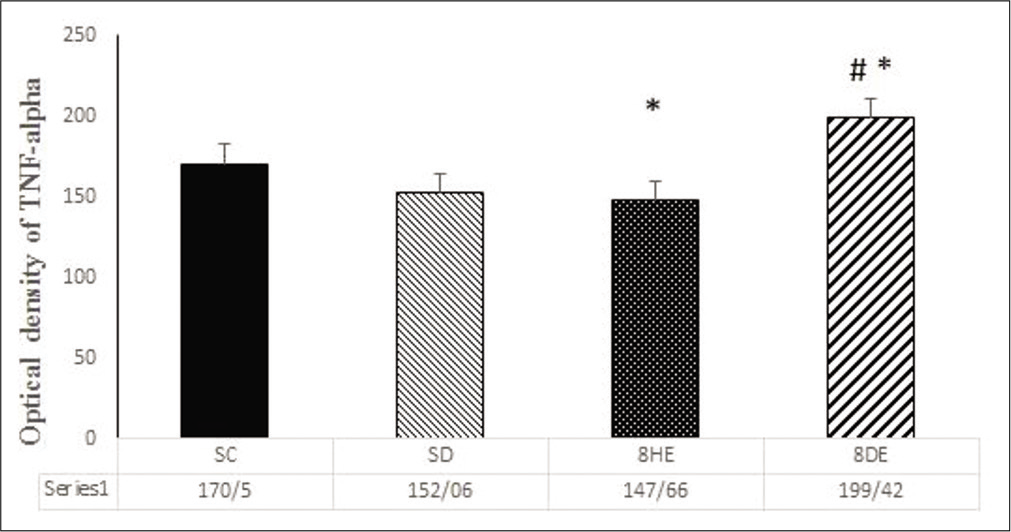
- Optical density of tumour necrosis factor-α. Sedentary control (SC) group, sedentary diabetic (SD) group, 8-week healthy exercised (8HE) group and 8-week diabetic exercised (8DE) group. Data are Mean±SEM, *P<0.05 versus SC group and #P<0.05 versus SD group.
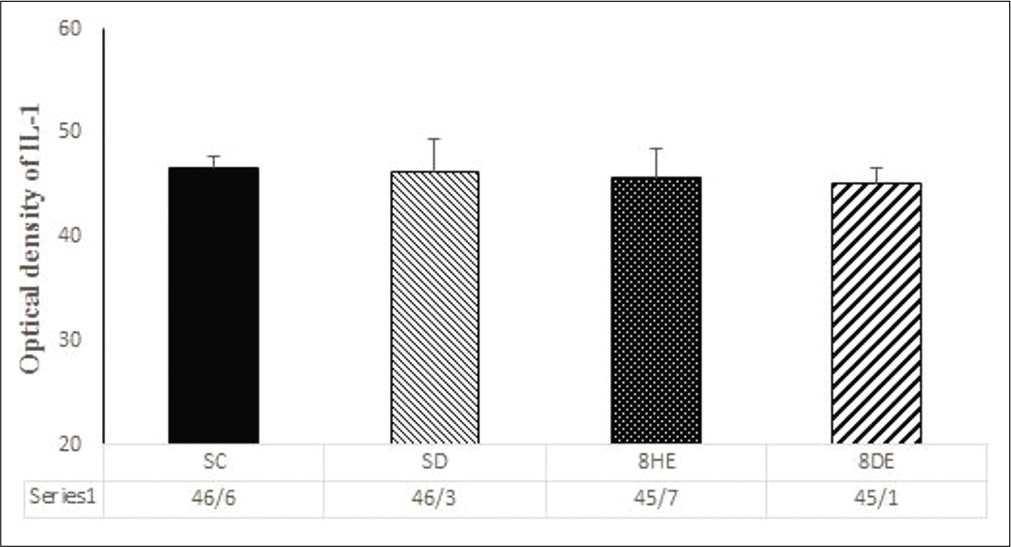
- Optical density of interleukin-1. Sedentary control (SC) group, sedentary diabetic (SD) group, 8-week healthy exercised (8HE) group and 8-week diabetic exercised (8DE) group. Data are Mean±SEM.
DISCUSSION
Our previous results showed[11] that Type-1 diabetes significantly resulted in increased blood glucose in rats, whereas 8-week exercise decreased the blood glucose in diabetic rats. Moreover, a significant reduction was found in healthy exercised rats, while an increase was observed in diabetic exercised rats as compared to SC and SD groups. The mentioned results are in line with findings in 60-day voluntary exercise treatment,[13] but it is in contrast with some other studies that used intensive exercise as a treatment.[14] The reason for this difference could be due to the intensity and duration of exercise. Exercise can reduce the blood glucose levels by increasing the sensitivity of GLUT4 in muscle as well as the insulin receptor substrate.
Inflammation is associated with both acute and chronic hyperglycemia.[15] Several studies have reported controversial data for the serum levels of cytokines in people with diabetes.[16-18] The reasons for these contradictory findings could be the differences in may the duration of diabetes inflammatory-related cells in the immune system release TNF-α as the first inflammatory cytokine following inflammation invoking other cytokines to the place of inflammation.[19,20] IL-1 is one of the main mediators of inflammation and this protein is important in the pathway of apoptosis.[21]
The serum levels of TNF-α and IL-1 increase 2 or 3 times more in chronic diseases such as diabetes than the normal range.[20] Since after 8 weeks induction of Type-1 diabetes in rats (SD group), no significant differences were observed in IL-1 tissue levels, so maybe the observed rise in the serum levels of IL-1 and TNF-α in diabetic patients, in Lysiak study, not have the origin of the retina and optic nerve. Or, maybe 2-month diabetes induction was not sufficient for the alteration of pro-inflammatory cytokine levels in SD rats, and because of the high mortality rate of SD rats, the opportunity to extend the treatment period reduced.
Regular exercise is well-documented method for reduction of blood glucose levels in diabetic patients. Blood glucose has been shown to increase the inflammatory mediator levels some types of exercise were considered to evaluate their effect on the levels of TNF-α and IL-1 cytokines by reducing blood glucose level. As the results of some studies have been shown that regular exercise can reduce blood glucose and then attenuated diabetes complications.[11,12]
The results indicated that the long-term exercise significantly reduced TNF-α levels in the retina and optic nerve tissues as compared to controls. In line with our results, some studies showed that exercise can reduce the TNFα levels.[22,23]
A possible explanation for our results could be the role of IL-6, the previous studies have shown that exercise increases the expression of IL-6 in contracted muscle cell, then IL-6 protein enters the bloodstream and reduces TNF-α levels by increasing the level of TNF-α cytokine inhibitor (STNF-α).[24]
Exercise can provide the reasons for activating the adrenal gland and secretion of epinephrine. Several studies suggest that exercise can reduce TNF-α levels by increasing the epinephrine levels.[24]
Our findings also showed that the combination of diabetes with long-term exercise led to an increase in the TNF-α level compared to the control group [Figure 1].
Since diabetes alone cannot increase the level of TNF-α in the retina and optic nerve tissues and that the exercise could decrease the level of the pro-inflammatory factor in these tissues, it can be argued that the association of diabetes with moderate exercise not only reduced the effects of exercise on the level of TNF-α but also led to an increase its level. Diabetes increases the liver CRP protein by increasing the IL-6 levels and neutrophils amounts.[24] This protein enters the bloodstream and inhibits the production of epithelial nitric oxide synthase,[25] this inhibition decreases nitric oxide and increases endothelin-1 production. Reduction of nitric oxide results in decrease of vascular dilatation. Moreover, evaluation of endothelin-1 increases the vessel contraction leading to increased shear stress and vascular damage.[26,27] Therefore, diabetes increases the shear stress and vascular damage. Exercise has been shown to enhance the shear stress.[28] The previous studies have shown that shear stress leads to progress in the TNF-α and IL-6, pro-inflammatory factors, level. Hence, it may be argued that exercise and diabetes together may increase the shear stress in the retina and optic nerve and then contribute to enhancement of the TNF-α production.
We also found that diabetes induction could not alter the levels of IL-1 in the retina and optic nerve [Figure 2]. This finding is consistent with a number of research that has reported no changes in serum IL-1 levels in healthy and diabetic subjects following exercise.[29]
Overall, the results of the present study showed that diabetes, not effective in the level of pro-inflammatory factors (IL-1 and TNF-α) after 8 weeks. And only, the significant change was detected in the level of TNF-α following 8-week exercise treatment in diabetic rats. Hence, the association of diabetes with this type of exercise protocol may increase the TNF-α level and progresses the shear stress. Consequently, this exercise protocol is not appropriate to reduce the risk of diabetes mellitus and its complications in retina tissue and optic nerve.
CONCLUSION
Long term exercise protocol was useful in healthy rats but don’t decrease of pro-inflammatory retinal complication in diabetes mellitus.
Acknowledgments
This research was carried out with the support of University of Tabriz, Iran.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Diabetic retinopathy. The Epidemiology of Eye Disease. Baltimore 2012:547-69.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for progression to proliferative diabetic retinopathy in the EURODIAB prospective complications study. Diabetologia. 2001;44:2203-9.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond). 2015;2:17.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammation, stress, and diabetes. J Clin Invest. 2005;115:1111-9.
- [CrossRef] [PubMed] [Google Scholar]
- TNF-alpha mediated apoptosis plays an important role in the development of early diabetic retinopathy and long-term histopathological alterations. Mol Vis. 2009;15:1418-28.
- [Google Scholar]
- Interleukin-1 (IL-1) family of cytokines: Role in Type 2 diabetes. Clin Chim Acta. 2012;413:1163-70.
- [CrossRef] [PubMed] [Google Scholar]
- Tumor necrosis factor-alpha in diabetic plasma increases the activity of core 2 GlcNAc-T and adherence of human leukocytes to retinal endothelial cells: Significance of core 2 GlcNAc-T in diabetic retinopathy. Diabetes. 2004;53:2968-76.
- [CrossRef] [PubMed] [Google Scholar]
- Role of interleukin-1 beta in the pathogenesis of diabetic retinopathy. Br J Ophthalmol. 2004;88:1343-7.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetic retinopathy: Vascular and inflammatory disease. J Diabetes Res. 2015;2015:582060.
- [CrossRef] [PubMed] [Google Scholar]
- Physical activity, exercise and diabetes. Can J Diabetes. 2013;37:359-60.
- [CrossRef] [PubMed] [Google Scholar]
- Attenuation of phosphorylated connexin-43 protein levels in diabetic rat heart by regular moderate exercise. Arch Iran Med. 2014;17:569-73.
- [Google Scholar]
- Phosphorylated connexin 43 protein levels attenuation in the retina of adult diabetic male rats, by regular moderate exercise. World Appl Sci J. 2013;28:2211-6.
- [CrossRef] [Google Scholar]
- Effects of voluntary exercise on heart function in streptozotocin (STZ)-induced diabetic rat. Int J Diabetes Metab. 2007;15:32-7.
- [Google Scholar]
- Effects of hyperosmotic shrinking on ventricular myocyte shortening and intracellular Ca2+ in streptozotocin-induced diabetic rats. Pflugers Arch. 2002;444:446-51.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: Role of oxidative stress. Circulation. 2002;106:2067-72.
- [CrossRef] [PubMed] [Google Scholar]
- Cytokine profile of peripheral blood in Type 2 diabetes mellitus patients with diabetic retinopathy. Ann Clin Lab Sci. 2008;38:361-7.
- [Google Scholar]
- Serum levels of cytokines and adipokines in patients with non-alcoholic steatohepatitis and Type 2 diabetes mellitus. Int J Bioflux Soc. 2011;8:77-84.
- [Google Scholar]
- Changes in the levels of cytokines in both diabetic/non-diabetic Type I children living in a moderate altitude area in Saudi Arabia. High Alt Med Biol. 2014;15:380-7.
- [CrossRef] [PubMed] [Google Scholar]
- Signaling in innate immunity and inflammation. Cold Spring Harb Perspect Biol. 2012;4:a006049.
- [CrossRef] [PubMed] [Google Scholar]
- The role of tumor necrosis factor-alpha and interleukin-1 in the mammalian testis and their involvement in testicular torsion and autoimmune orchitis. Reprod Biol Endocrinol. 2004;2:9.
- [CrossRef] [PubMed] [Google Scholar]
- The role of inflammatory and anti-inflammatory cytokines in the pathogenesis of human tegumentary leishmaniasis. Cytokine. 2014;66:127-32.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of aerobic exercise training on plasma levels of tumor necrosis factor alpha in patients with heart failure. Am J Cardiol. 2001;88:805-8.
- [CrossRef] [Google Scholar]
- Effect of aerobic exercise on serum concentration of apelin, TNFalpha and insulin in obese women. Iran J Basic Med Sci. 2012;15:1196-201.
- [Google Scholar]
- The anti-inflammatory effect of exercise. J Appl Physiol 1985. 2005;98:1154-62.
- [CrossRef] [PubMed] [Google Scholar]
- Role of TNF-α in vascular dysfunction. Clin Sci (Lond). 2009;116:219-30.
- [CrossRef] [PubMed] [Google Scholar]
- Endothelial dysfunction in diabetes mellitus: Molecular mechanisms and clinical implications. Rev Endocr Metab Disord. 2010;11:61-74.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular effects of exercise: Role of endothelial shear stress. J Am Coll Cardiol. 1996;28:1652-60.
- [CrossRef] [Google Scholar]
- The effect of regular training on plasma cytokines response in healthy and diabetic rats. Saudi Med J. 2009;30:1390-4.
- [Google Scholar]






