Translate this page into:
Transient receptor potential vanilloid 1 (TRPV1) receptor stimulation by topical capsaicin for the functional assessment of diabetic neuropathy leading to diabetic foot disease
*Corresponding author: Velpandian Deepshidha, Department of Community Medicine, Rajshree Medical Research Institute, Bareilly, Uttar Pradesh, India. deepshidha98@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Deepshidha V, Agrawal VK. Transient receptor potential vanilloid 1 (TRPV1) receptor stimulation by topical capsaicin for the functional assessment of diabetic neuropathy leading to diabetic foot disease. Indian J Physiol Pharmacol 2022;66:286-92.
Abstract
Objectives:
As neuropathy predominates vasculopathy, predicting functional deterioration of autonomic neurovascular dysfunction is essential to reduce diabetic foot ulcers. The present study has evaluated the possibility of stimulating the TRPV1 receptors of the small fibres using topical capsaicin to assess diabetic neuropathy in the dorsum of the foot functionally.
Materials and Methods:
A prospective cross-sectional study was carried out on ten healthy volunteers and 20 diabetic patients after receiving ethical approval. The subjects underwent vascular Doppler analysis after giving written agreement followed by monofilament testing. Then, topical capsaicin was applied to measure the local autonomic neurovascular reaction. With the use of an infrared-based digital instrument that was specially created, the vasodilation and proportional increase in temperature brought on by the application of capsaicin were quantified.
Results:
The percentage change in the local temperature in the control group varied from 0.478 to 3.315 compared to the diabetic group, which varied from 1.862 to −3.932. There is a statistically significant difference in the mean of the two groups (P = 0.006) at a 95% confidence interval.
Conclusion:
This study suggests that TRPV1 receptor stimulation using capsaicin and resultant vasodilation monitored by the increase in local temperature can be used as a quantitative predictor of the early small fibre neuropathy in Distal Symmetric Polyneuropathy before the patient ends up with diabetic foot ulcer.
Keywords
Capsaicin
Diabetic neuropathy
Distal symmetric polyneuropathy
Small fibre neuropathy
TRPV cation channels
INTRODUCTION
India is one of the epicentres of the global diabetes mellitus (DM) pandemic, having 2nd highest number in the world with 69 million as of 2015 (according to IDF Atlas). ICMR– INDIAB[1] collaborative study group reported that the overall prevalence of diabetes and prediabetes in the general population estimated across 15 states of India was found to be 7.3% (95% CI, 7.0–7.5) and 10.3% (10.0–10.6), respectively. Foot disease affects nearly 6% of people with diabetes[2] and includes infection, ulceration or destruction of foot tissues.[3] Foot complications in DM impair the quality of life and pose the highest financial burden among various microvascular and macrovascular complications seen in diabetes.[4]
The most common form of diabetic neuropathy is distal symmetric polyneuropathy (DSPN), accounting for 75%. DSPN is classified into large and small fibre neuropathy.[5] In prediabetics and early stage of type 2 diabetes mellitus (T2DM), both symptomatic and subclinical neuropathy are frequent, with unmyelinated small diameter or lightly myelinated nociceptive and autonomic fibres being predominantly affected.[6] Hence, detection of small fibre neuropathy (SFN) becomes paramount in preventing DSPN. Still, the various tools employed for this purpose fail to detect DSPN in clinical practice due to their shortcomings, including skin punch biopsy, which is invasive and, hence, only employed for research purposes, quantitative sensory testing that is a psychophysical test thus subject to bias and corneal confocal microscopy, that is, expensive, also requiring additional studies to determine its sensitivity and specificity before it can be used in clinical practice. Nerve conduction study is considered the gold standard for detecting DSPN,[7] but it cannot diagnose SFN.[8]
The degenerative process is thought to occur at the cutaneous unmyelinated nerve fibre endings.[9] Hence, topical capsaicin was used in this study as it acts on the TRPV1 receptors in the primary afferent nociceptive A⌧ and C fibres, leading to the influx of calcium ions. This initiates an orthodromic action potential transmitted through the spinal cord to the brain causing pain sensation along with antidromic conduction in the form of a localised axonal reflex, leading to neurogenic inflammation and vasodilation.[10] In vitro studies suggest that TRPV1 channels in vascular endothelial cells modulate the vascular function through Nitric Oxide (NO), Calcitonin Gene-Related Peptide (CGRP), Substance P and IKCa/SKCa channel activation in response to capsaicin.[11] This allows the possibility of using capsaicin-induced neuronal vasodilation as a model to assess the detection of diabetic neuropathy.
Semmes-Weinstein Monofilament (SWM) is easily accessible and the most widely used screening tool for diabetic neuropathy in India. It is a prevalently acceptable standard and, therefore, has been used for the comparative assessment in the present study. It determines the loss of protective sensation using the buckling force of the monofilament. 10 g SWM was used in the present study as widely recommended in practice.[12] Hence, this study aims to assess capsaicin’s ability to predict small fibre neuropathy by quantifying the neurovascular repose resulting in vasodilation and proportional rise in local temperature measured using a surface IR sensor. A specially designed digital IR temperature measuring device has been developed to increase the sensitivity to quantify skin surface temperature in close contact.
MATERIALS AND METHODS
A handheld vascular Doppler (VCOMIN-320, VCOMIN technology Ltd, China) having a probe frequency of 8 MHz was used for the blood flow assessment. Topical capsaicin (Sigma, USA), water-soluble cream (6%w/w), was prepared with the help of a qualified compounding Pharmacist (Dr. RPC Pharmacy, AIIMS). Monofilament 5.07/10 g was procured from M/s Diabetik Foot Care India Pvt Ltd, Chennai.
The surface IR measurement probe has been specially fabricated for this study to measure surface temperature on skin with close contact. It was constructed using an MLX90614 infrared sensor (Melexis, China), having an accuracy of ±0.5°C and a measurement resolution of 0.02°C. The IR sensor was connected to Arduino nano microcontroller board (Arduino, Italy) and was programmed using open-source software with minor source code modifications [Figure 1a]. A container to house the components were 3D printed using Poly Lactic Acid polymer designed through FreeCAD open source (Ver.0.17), 3D designing software. The data obtained showed that the sensor could detect the change in the local temperature after applying capsaicin very accurately. The resultant optimised Digital Infrared Surface Thermal Analyser (DIRSTA) is shown in [Figure 1b].

- (a) Circuit diagram for Developed Digital Infrared Surface Thermal Analyser (DIRSTA) and (b) DIRSTA prototype.
Study protocol was approved by the Institute Standing Human Ethics Committee (IEC) and was conducted as per the ICMR National Ethical Guidelines for Biomedical and Health Research Involving Human Participants and in accordance with the inclusion and exclusion criteria. Written informed consent was taken from the participants before conducting the study.
Process of informed consent
The participant and patient information sheets were prepared, and the subjects were detailed about the study. Any related queries were addressed, and a consent form was signed before their enrolment for the study.
Development and standardisation of the method of analysis
A preliminary study was conducted using ten volunteers after getting permission from the IEC to standardise the methodology and assess the effectiveness of the dosage of capsaicin and the working of DIRSTA. Low doses of capsaicin (0.1–4%) elicited a detectable change in local temperature when applied to the upper limb but failed to bring about a significant difference in the temperature when applied over an area of 1 cm × 1 cm on the dorsolateral aspect of the foot. The safety of a higher dosage of capsaicin, up to 8%, has already been established in clinical settings.[13] Hence, 6% (w/w) capsaicin was used for the present study as it gave a positive response. The study plan is shown in [Figure 2].

- Study plan.
Clinical assessment of the developed method by comparing it with the standard monofilament test
From the preliminary study, the optimum condition for the assessment of maximum vascular response was obtained.
Sample size
Based on inclusion and exclusion criteria, healthy (n = 10) and diabetic (n = 20) adult subjects willing to consent to this study were selected from the medicine OPD.
Inclusion criteria and exclusion criteria
Healthy subjects with no chronic ailment, non-alcoholic and non-diabetic were selected, and their prior medical history was assessed, following which they were included in the control group. Patients suffering form Type 1 or T2DM > 8 years and exhibiting symptoms of DSPN were included in the diabetic group.
Those with ailments and undergoing drug therapy known to affect vascular tone were excluded from the study. Patients with other known neuropathy causes such as vasculitis, amyloidosis, toxic neuropathy, AIDS, hepatitis B and C, smoking, renal failure and alcohol abuse were excluded from the study. Diabetic patients found to have symptomatic lumbosacral spine disease, infected foot ulcers, history of chronic pain or neurological and/or musculoskeletal abnormalities, pregnancy, lactating mothers, any other severe comorbid condition, peripheral vascular disease, infectious disease and those who refused to participate in the study were excluded from the study.
Assessment protocol
The study subjects were asked to lie down in the supine position. The area for capsaicin application was cleaned using a 70% alcohol swab and allowed to dry. Then, a square area of 1 × 1 cm was drawn using a non-toxic marker on both feet at some distance away from the little toe on the dorsolateral side using the procedure established by Linde and Srbely.[14] The marked area was assessed for the local temperature (Taken as the 0 min. reading) with the help of DIRSTA.
Immediately after taking the initial temperature reading, 6% capsaicin cream (0.6 mg in 10 mg) was applied as a thin film within the marked area of 1 cm2 with the help of a calibrated applicator in one foot, while the other foot served as the control [Figure 3]. It was left undisturbed for 15 min and then wiped out. After that, the change in temperature at the application site was recorded successively every 15 min at 30, 45 and 60 min, respectively [Figure 4]. An additional 75 and 90 min reading was required in the diabetic group due to the delayed response observed.

- Site of application of capsaicin corresponding to the area innervated by the sural nerve.

- Measuring vasodilation-induced change in surface temperature using the DIRSTA before and after capsaicin application.
All participants underwent vascular Doppler testing used to measure the ankle-brachial pressure index (ABPI) to exclude peripheral arterial disease and a 10 g SWM test to ensure their neuronal health. ABPI was measured as per the technique suggested by Stanford medicine.[15] Monofilament testing was done at ten sites per foot, nine on the plantar side and one on the dorsum of the foot, as shown in [Figure 5].

- Sites for monofilament testing.
Statistical analysis
Capsaicin-induced maximum increase in surface temperature was calculated in terms of pharmacodynamic effect (Emax) and the given time of assessment (Tmax). The Emax of all healthy volunteers was pooled in one group – the ‘Control group’ and the Emax of all diabetic patients was pooled in the 2nd group – the ‘Diabetic group’ and values were reflected as Mean ± SEM. To assess the statistical significance between two-time points (Control and Diabetic), unpaired Student ‘t’ was used and the value of P < 0.05 has been considered significant. Sigma plot 11 software was used for testing the significance.
RESULTS
Thirty subjects participated in this study, ten of whom were healthy volunteers, including six females and four males with a mean age of 34.4 years (range 21–50 years) and 20 diabetic patients, including 12 males and eight females with a mean age of 56.95 years (range 40–68 year). The HbA1C of 15 out of the 20 diabetic patients was found to be ranging from 5.7 to 13.2, with an average of 9.94 mg/dL. All 20 diabetic patients reported symptoms of DSPN, mainly small fibre neuropathy and had been living with diabetes for over 8 years.
All ten healthy volunteers underwent vascular Doppler exhibiting an ABPI within the range of >0.9 and <1.3 and responded to monofilament testing in all the ten sites examined in both feet.
In the diabetic group, 16 of the 20 patients underwent vascular Doppler testing. Five out of those 16 showed some degree of arterial obstruction with an ABPI of <0.9. However, none severe enough to have an ABPI of <0.5. Of the five that showed some degree of arterial obstruction, one had diabetic foot and a non-reactive monofilament test. All 20 diabetic patients underwent monofilament testing, of which three had decreased or no response to the SWM, and further, two of those three had diabetic foot ulcers.
When treated with topical capsaicin, the percentage change in the temperature in the control group varied from 0.478 to 3.315 and in the diabetic group from 1.862 to −3.932 [Figure 6]. At a 95% confidence interval, there is a statistically significant difference in the mean Emax of C-fibre stimulation using capsaicin in healthy versus diabetic subjects (P = 0.006).
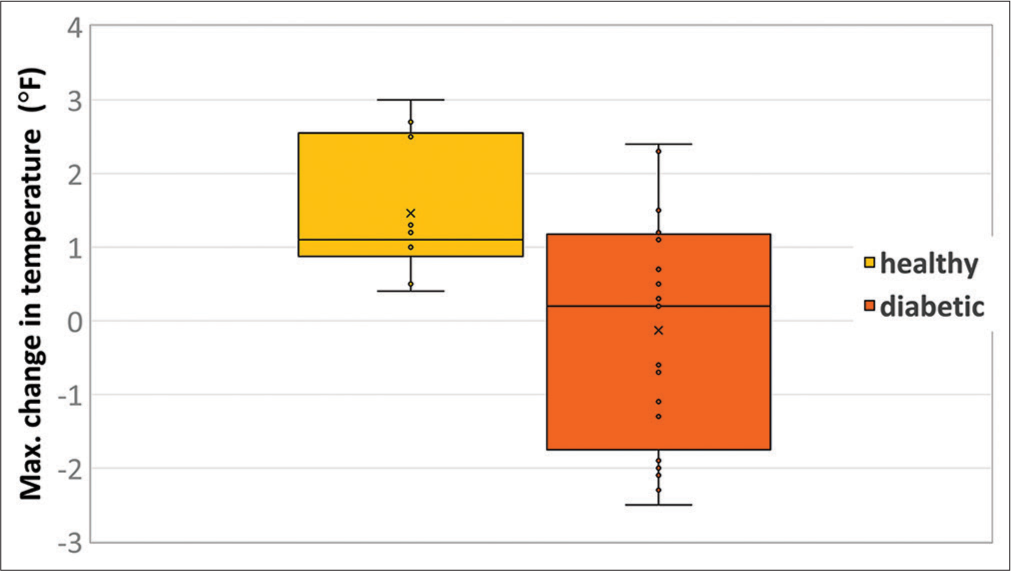
- Emax of C-fibre stimulation using capsaicin in healthy versus diabetic subjects (p=0.006).
The maximum change in temperature was recorded at an average time of 45 min in the control group and 60 min in the diabetic group after the application of capsaicin, suggesting a delayed response in those with diabetic neuropathy [Figure 7]. It was also observed that nine out of the 20 subjects in the diabetic group showed no increase in temperature after the application of capsaicin, and the remaining diabetic subjects showed only a small increment. In the control group, however, all ten volunteers responded to capsaicin with an increase in local temperature.
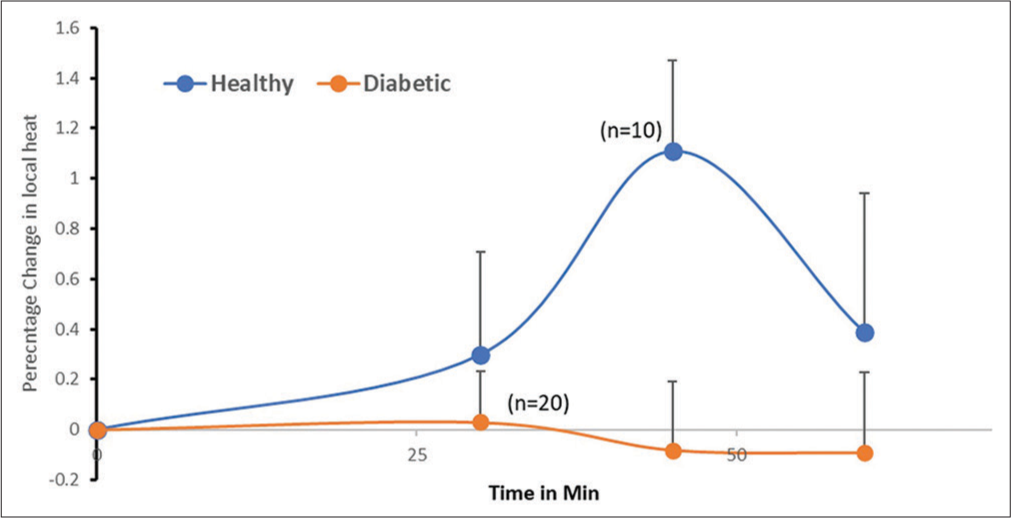
- Percentage change in local heat after C-fibre stimulation in healthy versus diabetic subjects.
In the present study, monofilament detected abnormalities in only three out of the 20 diabetic subjects, two out of whom had already developed diabetic foot ulcers. In the capsaicin experiment, nine out of the 20 diabetic subjects showed no response to C-fibre stimulation and a significantly decreased response was observed in the rest of the participants. From this observation, it is evident that monofilament testing, one of the most widely employed tests for detecting DSPN in India, fails to show uniformity in detecting neuropathy.
DISCUSSION
Diabetic peripheral neuropathies are a variety of syndromes that affect sensory, autonomic and motor nerve function and DSPN has been considered a major risk factor for foot ulceration, leading to lower limb amputation.[16] Therefore, this study was initiated to develop a suitable technique to predict the autonomic neurovascular dysfunction of the foot using topical capsaicin. DIRSTA was designed and used for close contact measurement of surface temperature.
The topical application of capsaicin as a cream has been reported to be a reproducible, sensitive, minimally invasive and robust approach for the quantification and study of thermal pain.[17] Activation of TRPV1 (vanilloid channels) by capsaicin triggers a neuronal inflammatory pathway, leading to the release of bioactive mediators such as calcitonin gene-related peptide, neurokinin A, nitric oxide and prostaglandins.[18] The concentration of capsaicin used in this study is well below the established safety limit, and no significant adverse events were reported by any of the 30 participants. Some of the healthy subjects did experience mild local irritation and allodynia that lasted for a few hours after the exposure, but no systemic side effects were reported.
Diabetic neuropathy has been reported to exhibit length-dependent nerve involvement in the ‘stocking and glove’ pattern.[19] As the longest sensory axons are the first to be affected, the dermatome corresponding to the sural nerve supply (at the dorsolateral aspect of foot) was selected as the site of application of capsaicin in the present study.
Considering the convenience and compliance of the subjects, the periodicity of evaluation of study parameters during the conduct of the experiment could not be spaced closely. Furthermore, due to the study limitations, other methods used for evaluating neuropathy could not be compared with these findings. Therefore, further studies employing laser Doppler flowmetry with frequent monitoring, along with individual comparisons among the various assessment methods, would help to understand the usefulness of TRPV1 activation-mediated autonomic neurovascular phenomenon over other techniques for predicting diabetic foot disease.
The results of the present study show a substantial reduction in the neuronal pathway-mediated localised rise in temperature in diabetic patients and suggest that the measurement of neurovascular response to C-fibre stimulation using capsaicin is a simple, safe, feasible, cost-effective and unbiased technique for the objective prediction of SFN for the primary prevention of diabetic foot disease. Further horizontal studies with a larger sample size will help to establish the proposed method’s sensitivity and specificity and to gain insight into its performance in clinical practice.
CONCLUSION
This study has proved that capsaicin-induced vasodilation and the measurement of its associated increase in local temperature can detect SFN, which is shown to be the predominant form in the initial stages of DSPN. Hence, the integration of this test in clinical practice can prove to be highly beneficial to the patients and society at large as it can decrease the financial and emotional burden caused by diabetic neuropathy and its complications, mainly diabetic foot which is a major emerging problem in the present times, especially in India.
Acknowledgment
The study was conducted under the Short Term Studentship (STS)-2020 program initiated by ICMR. STS fellowship was awarded to Velpandian Deepshidha. We acknowledge Dr. Ajit Sawhney, Dept of Endocrinology, for providing extensive support for this study. We also thank Dr. Pankaj Sharma, Ocular Pharmacology and pharmacy division of Dr. RP Center, AIIMS, for helping us formulate the capsaicin preparation.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Conflicts of interest
Nil.
Financial support and sponsorship
This research was conducted under short Term Studentship (2020) awarded to V.Deepshidha by ICMR (India).
References
- Prevalence of diabetes and prediabetes in 15 states of India: Results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5:585-96.
- [CrossRef] [PubMed] [Google Scholar]
- Global epidemiology of diabetic foot ulceration: A systematic review and meta-analysis. Ann Med. 2017;49:106-16.
- [CrossRef] [PubMed] [Google Scholar]
- The international consensus and practical guidelines on the management and prevention of the diabetic foot. Curr Diab Rep. 2003;3:475-9.
- [CrossRef] [PubMed] [Google Scholar]
- Economic burden of diabetic patients in India: A review. Diabetes Metab Syndr. 2019;13:2469-72.
- [CrossRef] [PubMed] [Google Scholar]
- The Utah early neuropathy scale: A sensitive clinical scale for early sensory predominant neuropathy. J Peripher Nerv Syst. 2008;13:218-27.
- [CrossRef] [PubMed] [Google Scholar]
- Performance analysis of noninvasive electrophysiological methods for the assessment of diabetic sensorimotor polyneuropathy in clinical research: A systematic review and meta-analysis with trial sequential analysis. Sci Rep. 2020;10:21770.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnostic challenge of small fibre neuropathy: Clinical presentations, evaluations, and causes. Lancet Neurol. 2017;16:934-44.
- [CrossRef] [PubMed] [Google Scholar]
- The usefulness of quantifying intraepidermal nerve fibers density in the diagnostic of diabetic peripheral neuropathy: A cross-sectional study. Diabetol Metab Syndr. 2016;8:31.
- [CrossRef] [PubMed] [Google Scholar]
- Roles of TRPV1 and neuropeptidergic receptors in dorsal root reflex-mediated neurogenic inflammation induced by intradermal injection of capsaicin. Mol Pain. 2007;3:30.
- [CrossRef] [PubMed] [Google Scholar]
- TRPV channels and vascular function. Acta Physiol (Oxf). 2011;203:99-116.
- [CrossRef] [PubMed] [Google Scholar]
- Use of graded Semmes Weinstein monofilament testing for ascertaining peripheral neuropathy in people with and without diabetes. Diabetes Res Clin Pract. 2019;151:1-10.
- [CrossRef] [PubMed] [Google Scholar]
- Profile of the capsaicin 8% patch for the management of neuropathic pain associated with postherpetic neuralgia: Safety, efficacy, and patient acceptability. Patient Prefer Adherence. 2016;10:1913-8.
- [CrossRef] [PubMed] [Google Scholar]
- The acute effect of skin preheating on capsaicin-induced central sensitization in humans. Pain Pract. 2019;19:811-20.
- [CrossRef] [PubMed] [Google Scholar]
- Alternative ankle-brachial index method identifies additional at-risk individuals. J Am Coll Cardiol. 2013;62:553-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetic peripheral neuropathies: Their cost to patient and society and the value of knowledge of risk factors for development of interventions. Eur Neurol. 1999;41:35-43.
- [CrossRef] [PubMed] [Google Scholar]
- Differentiation between capsaicin-induced allodynia and hyperalgesia using a thermal operant assay. Behav Brain Res. 2006;170:308-15.
- [CrossRef] [PubMed] [Google Scholar]
- Distinct BOLD fMRI responses of capsaicin-induced thermal sensation reveal pain-related brain activation in nonhuman primates. PLoS One. 2016;11:e0156805.
- [CrossRef] [PubMed] [Google Scholar]






