Use of high-fidelity simulator for teaching cardiovascular physiology principles to the 1st year undergraduate medical students
*Corresponding author: Anahita R. Shenoy Basti, Department of Physiology, Fr Muller Medical College, Mangaluru, Karnataka, India. anahitakini@yahoo.in
-
Received: ,
Accepted: ,
How to cite this article: Suvarna P, Basti AR. Use of high-fidelity simulator for teaching cardiovascular physiology principles to the 1st year undergraduate medical students. Indian J Physiol Pharmacol 2022;66:293-8.
Abstract
Objectives:
Medical education has undergone significant changes all over the world and patient safety is one of the main reasons for the changes. The new competency-based medical curriculum in India also emphasises early clinical exposure along with the acquisition of competent and verifiable skills. The objective of this study was as follows: (1) to introduce the 1st year medical students to simulation-based learning (SBL) to develop their knowledge, skills, and communication and meet the desired learning objectives without exposing subjects to any harm and gain valuable immersive experience that felt real and (2) to obtain students feedback about SBL in learning applied aspects of physiology.
Materials and Methods:
The study was approved by the Institutional Ethical Committee. A total of 132 1st year medical students were divided into six batches and each batch was exposed to a pre-test, simulation exercise, a debriefing session, post-test, and feedback. Descriptive analysis of the data was done and values were expressed as mean and standard deviation. The McNemar test was used to study the effectiveness of SBL.
Results:
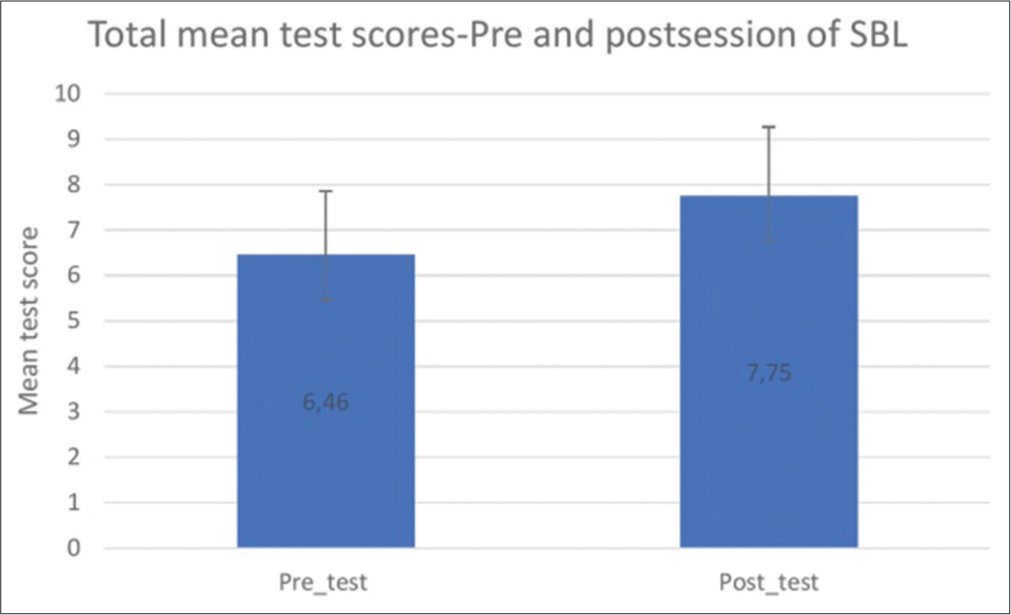
The average pre-test and post-test correct responses were 64.6% and 77.5%, respectively. This difference was found to be highly significant with P < 0.001. The mean pre-test score and post-test scores were 6.46 ± 1.39 and 7.75 ± 1.52, respectively, with P < 0.001. P < 0.05 was considered statistically significant. Positive feedback was received from the students with 86.8% of them strongly agreeing to the incorporation of simulation-based activities in the curriculum. About 76.7% strongly agreed to a self-perceived increase in their decision-making, communication, and teamwork skills. Perception of the simulation as a realistic experience was perceived by 74.4% of the students.
Conclusion:
SBL is an effective tool for learning applied physiology and was viewed by the students with interest. It also enhanced their understanding of the pathophysiological basis of the clinical scenario.
Keywords
Physiology
Simulation
Undergraduate medical students
INTRODUCTION
Medical simulation is an emerging new day methodology for training medical professionals using advanced technology in India. Simulation provides a realistic standardised experience for learners in a controlled environment and unlike learning with real subjects, simulation allows desired learning objectives to be met without exposing subjects to any harm. This teaching tool has revolutionised how medical concepts are delivered to learners and its effectiveness is well documented in training students in cardiac and respiratory management,[1] trauma management[2] and laparoscopic skills.[3]
Simulation exercises have also been utilised to teach preclinical concepts. In a study that utilised human patient simulator to teach cardiovascular physiology, students reported simulation to be a better teaching tool than lectures and wanted more topics to be covered using simulation.[4] Daniel et al. found that simulation-based learning (SBL) enhanced the domains of both knowledge and skill in applied cardiovascular physiology.[5]
Until now the preclinical period of medical education in India was mainly used to teach the basics of life sciences, but the new competency-based medical curriculum emphasises early clinical exposure along with the acquisition of competent and verifiable skills.[6] Measuring blood pressure is one such certifiable skill introduced in the 1st year of MBBS.
Thus, we, in our study, have incorporated the components that define skills like intellectual/cognitive skills, psychomotor skills, communication skills, and team skills into a simulation scenario that involves the recording of blood pressure. Moreover, we aimed to study the effectiveness and perceptions of the 1st year medical students of SBL as an adjunct to traditional teaching methods.
MATERIALS AND METHODS
Study design
This cross-sectional interventional study was conducted by the department of physiology in the simulation centre of our institution after obtaining ethical clearance. The institutional ethical clearance number is FMMCIEC/CCM/110/2019.
Case scenario development
A case scenario on haemorrhagic shock was developed that tested knowledge and skill as well as interpersonal communication of the students.
The scenario was – a 50-year-old man, with a history of a road traffic accident with bleeding from his leg, has come to the emergency department with complaints of weakness and giddiness. His baseline parameters were
Temp. 37℃
Pulse rate 110 beats/min
BP 90/60 mm of Hg
RR 15 breaths/min
The simulation exercise was developed keeping these objectives in mind –
To test clinical knowledge
To identify the signs and symptoms of shock
To initiate appropriate first aid.
To test skill
To measure accurately measure the pulse rate and blood pressure
To perform the clinical examination of the cardiovascular system.
To test communication
To demonstrate effective teamwork, and communication with teammates, nurses, and consultants.
The expected outcomes were that students should be able
To identify it as a case of haemorrhagic shock
To be able to correctly record the pulse rate and blood pressure (within ±5 beats/min and ±5 mm of Hg of the set value)
To initiate first aid like IV fluids and leg raise
To order relevant investigations to the nurse and communicate the patient status to the consultant using identifying the situation, background, assessment, and recommendation (ISBAR).
Study participants
The study participants were the 1st year undergraduate medical students. They were explained the study protocol and were informed that their participation was completely voluntary, responses would be anonymous, and would not influence their grading. A total of 132 students participated in the study and their pre-test and post-test score were analysed. However, feedback from only 129 students was analysed as three responses were incomplete and excluded from the study.
Theory class on shock and practical examination of the cardiovascular system had been completed previously.
The simulation exercise was conducted over 6 days. Students were divided into six batches of 25 each. The simulation consisted of (1) a 15 min written pre-test on shock, (2) 20 min simulation exercise, (3) 40 min debriefing session, and (4) 15 min post-test and their feedback on the SBL session.
Simulation scenario
In the simulation centre, the students were asked to sign the confidentiality agreement and were familiarised with the high-fidelity mannequin and the workstation. This was followed by the pre-test which consisted of 10 multiple-choice questions which tested their knowledge, understanding of the pathophysiological basis of the signs, symptoms, and treatment of shock as seen in the scenario. The students were not provided with the correct answers to the MCQ as the same questions were given in the post-test. Each question carried 1 mark. The correct answer was awarded 1 mark, no marks were given for incorrect or multiple responses.
Following the completion of the pre-test, a pre-briefing session was conducted where the case scenario was presented to the students and the objectives of the session were explained. The students were required to take a brief history, perform a clinical examination, start first aid measures and inform the consultant of the status of the patient.
The students were further divided into smaller groups and were assigned to either elicit history, record the vitals or perform a clinical examination of the CVS. They were instructed to work together to come up with suggestions for investigations that could help with the diagnosis and also come up with a provisional diagnosis. They were also instructed to initiate first-aid measures, and call and inform the consultant regarding the ‘patient’ status.
The students then entered the simulation scenario which was placed in an emergency department environment with actors comprising one nurse and one patient bystander, both enacted by the teaching faculty of our department. The high-fidelity simulator used was METIman (Medical Education Technologies Inc., CAE Healthcare, Canada). The voice of the simulator was managed behind the scenes by another faculty member. As the scenario evolved, the patient’s status was also modified accordingly as depicted in [Figure 1]. The faculties acted as facilitators throughout the scenario. All involved faculties have been trained and have completed certified courses in simulation. Students started with a brief elicitation of history followed by an examination of vitals and a clinical examination of the cardiovascular system.

- Sequence of events during SBL. SBL: Simulation-based learning.
Students were given 20 min to complete their evaluation, start first aid measures, and inform the consultant of their findings. The facilitators observed and evaluated the students’ performance based on a checklist. This was followed by a three-phase method of debriefing where the students expressed their reaction to the simulation scenario followed by the analysis of their performance in terms of the positive attributes and also the delta (deficiencies) and finally the summary of their experience. The facilitators then gave their constructive feedback and their observations, highlighting the positives and avoiding negative impact words to create a positive learning environment.
This was followed by a post-test and feedback session. The feedback form consisted of 14 questions of which 13 were rated on a 5-point Likert scale using strongly disagree and strongly agree as to the anchoring points, and one open-ended question was used to document the students’ opinion of the simulation exercise.
A total of 132 responses to the pre-and post-test were considered for the analysis. A total of 129 feedback responses from the students were analysed.
Data analysis
Descriptive analysis of the data was done and values were expressed as mean and standard deviation. The McNemar test was used to study the effectiveness of SBL. P ≤ 0.05 was considered statistically significant.
RESULTS
A total of 132 pre-and post-test responses and 129 responses to feedback responses were considered for the study. All students were in the age group of 17–20 years.
The percentage of correct responses in pre-test and post-test is depicted in [Table 1]. The percentage of correct responses was found to be significantly higher in the post-test (P < 0.001). Analysis of the student feedback is represented in [Table 2]. About 86.8% of the students want simulation-based activities to be included in the curriculum. Furthermore, 76.7% of the students perceive an increase in their decision-making, communication, and teamwork skills.
| Question no. | Pre-test (%) | Post-test (%) | P value |
|---|---|---|---|
| n=132 | |||
| 1. | 45.5 | 74.2 | <0.001 |
| 2. | 73.5 | 82.6 | 0.112 |
| 3. | 90.2 | 97 | 0.049 |
| 4. | 74.2 | 90.9 | <0.001 |
| 5. | 94.7 | 97.7 | 0.344 |
| 6. | 89.4 | 93.9 | 0.286 |
| 7. | 76.5 | 87.9 | 0.033 |
| 8. | 21.2 | 40.2 | 0.001 |
| 9. | 39.4 | 59.1 | 0.002 |
| 10. | 41.7 | 51.5 | 0.143 |
| Total | 64.6 | 77.5 | <0.001 |
| Question | Strongly disagree (%) | Disagree (%) | Neutral (%) | Agree (%) | Strongly agree (%) | Mean | Standard deviation |
|---|---|---|---|---|---|---|---|
| I was able to understand the given problem | 0 | 0 | 4 (3.1) | 46 (35.7) | 79 (61.2) | 4.58 | 0.55 |
| I got to know additional information on the given topic | 0 | 0 | 3 (2.3) | 41 (31.8) | 85 (65.9) | 4.64 | 0.53 |
| I was able to understand the clinical symptoms and signs of the patient | 0 | 0 | 9 (7) | 56 (43.4) | 64 (49.6) | 4.47 | 0.60 |
| I was able to correlate the clinical features to the pathophysiology of the condition. | 0 | 0 | 7 (5.4) | 55 (42.6) | 67 (51.9) | 4.43 | 0.62 |
| I was able to reflect effectively by interacting with the facilitator during the discussion | 0 | 0 | 4 (3.1) | 31 (24) | 94 (72.9) | 4.70 | 0.52 |
| I was able to learn from the group discussion | 0 | 1 (0.8) | 7 (5.4) | 39 (30.2) | 82 (63.6) | 4.57 | 0.64 |
| I was able to come to a differential diagnosis based on the patient’s symptoms | 0 | 1 (0.8) | 16 (12.4) | 41 (31.8) | 71 (55) | 4.41 | 0.74 |
| I was able to understand my mistakes | 0 | 0 | 4 (3.1) | 47 (36.4) | 78 (60.5) | 4.57 | 0.56 |
| The simulation provided a realistic and valuable learning experience | 0 | 0 | 4 (3.1) | 29 (22.5) | 96 (74.4) | 4.71 | 0.52 |
| Simulation training enhances decision-making, communication and teamwork skill development | 0 | 0 | 5 (3.9) | 25 (19.4) | 99 (76.7) | 4.73 | 0.53 |
| A better understanding of physiology concepts has been achieved through simulation | 0 | 0 | 5 (3.9) | 30 (23.3) | 94 (72.9) | 4.69 | 0.54 |
| I am more confident in recording correctly BP, pulse and examination of precordium | 1 (0.8) | 2 (1.6) | 17 (13.2) | 59 (45.7) | 50 (38.8) | 4.20 | 0.78 |
| Simulation-based activities should be integrated in medical education curriculum | 0 | 0 | 3 (2.3) | 14 (10.9) | 112 (86.8) | 4.84 | 0.42 |
The top value is the number of students and in parenthesis is the % of the total
[Figure 1] shows the sequence of events during the simulation exercise. [Figure 2] is the graph representing the mean pre-test and post-test scores which were found to be 6.46 ± 1.39 and 7.75 ± 1.52. The interquartile range for the pre-test and post-test scores is 5.25–7 and 7–9, respectively. [Figure 3] is a picture of students performing the simulation exercise.
- Sequence of events during SBL. SBL: Simulation-based learning.

- Students performing the simulation exercise.
DISCUSSION
The objective of our study was to assess the effectiveness of SBL in the 1st year undergraduate medical students. The data from matched pre-and post-test showed a significant improvement in students’ knowledge immediately following the session and support our hypothesis that the use of simulation for active learning improved students’ understanding and knowledge. Favorable feedback was also given by the students about their simulation experience.
In our study, the average post-test scores were significantly higher than the pre-test score. A significantly higher percentage of students answered questions 1, 8, and 9 correctly in the post-test. These questions were about the vital signs in a patient with shock, the most appropriate fluid for treatment, and improvement seen in the vitals post-treatment. These were the parameters that were recorded by the students and thus the active learning could have facilitated better registration.
Questions 2, 6, and 10 were recall-based and were not discussed during the debriefing, and have not shown significant improvement in the post-test scores. In question 5, the pre-test score was above 90% thus limiting the ability to discriminate between pre- and post-testing scores.
Quantitative and qualitative research has shown an improvement in students’ knowledge, skill, and communication following simulation exercises.[7-9] A study by Jabaay et al. found students’ performance improved by 18% following the simulation experience.[10] A similar study that tested the knowledge and skills of undergraduate medical students in applied physiology of the cardiovascular system showed a significant improvement in the post-simulation exercise.[5]
In a study by Heitz et al., neurophysiology concepts were taught using a high-fidelity simulator. The post-test scores were higher compared to the pre-test, also summative assessment conducted 11 days later showed good retention of both application and recall-based questions. Feedback from these students showed that the majority of them reported that simulation enhanced their learning of the concepts of basic sciences.[11]
Students have rated simulation to be more stressful (mean 4.1, 95% CI 3.9–4.3), but also more enjoyable and more stimulating, and closer to the actual clinical setting compared to group discussion in a randomised control trial.[12]
Our simulation activity was well received by the students with 86.8% of them strongly agreeing to simulation-based activities to be included in their curriculum. About 76.7% strongly agreed to ‘Simulation training enhances decision-making, communication, teamwork, skill development.’ 74.4% found simulation provided a realistic and valuable learning experience. About 72.9% felt that a better understanding of physiology concepts was achieved.
For the open-ended question, asking for any other comments, a response such as ‘Realistic, panicky experience’ was received, indicating that students were engaged in the simulation exercise which is known to further enhance learning.[13] Another student wrote ‘Gave an overview of what lies ahead of us.’ Students also requested for more simulation sessions to be conducted in smaller groups.
Although the simulation activity had overall positive feedback, the lowest score received was for the question ‘I am more confident in recording correctly BP, pulse, and examination of the precordium.’ As the activity was group-based not all students got a hands-on experience of the clinical examination, this could probably attribute to the lack of confidence in performing the clinical skill. In the future, this could be overcome by conducting the simulation exercise in smaller groups. Keeping this feedback in mind, certification sessions were conducted to further enhance the confidence of the students.
The present generation of students relies heavily on technology for their learning. Thus, integration of technology into the curriculum in an attempt to achieve optimal results has become the need of the hour. Educators have found it challenging to make students realise the clinical relevance of physiological concepts. In our study, simulation exercise was used to enhance students understanding of the clinical relevance of physiological concepts in CVS. Although CBME curriculum insists on integration of simulation in the curriculum, there are limited data available in this area, thus, this can be considered the novelty of our study.
Learning with the help of simulation-based activities can help the students to link basic science concepts to their practical applications.[14] SBL improved the recalling of correct information, comprehension of that knowledge, and improved integration and application of that knowledge in a clinical scenario a concept strongly endorsed by the current competency-based undergraduate medical curriculum.
CONCLUSION
Based on the feedback received from the students, we can conclude that they viewed SBL with interest. The improvement in the post-test score indicates that the SBL was an effective tool to enhance understanding of the pathophysiological basis of the clinical scenario.
Limitation
The use of multiple-choice questions for assessment only tested the knowledge of the participants, but not their skills. Long-term retention was not evaluated, this can be taken up as further scope of our study. As the student-to-simulator ratio was high, the simulation had to be conducted in batches occupying a greater number of class hours. If this ratio is reduced, more simulation scenarios can be incorporated to achieve greater hands-on exposure and a better understanding of the clinical application of the concepts in physiology.
Acknowledgment
We would like to thank the simulation centre of our college for their support and guidance in conducting the simulation session.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- The effect of simulator training on clinical skill acquisition, retention and transfer. Med Educ. 2009;43:784-9.
- [CrossRef] [PubMed] [Google Scholar]
- The simulated trauma patient teaching module-does it improve student performance? J Trauma. 2007;62:1416-20.
- [CrossRef] [PubMed] [Google Scholar]
- Virtual reality and computer-enhanced training devices equally improve laparoscopic surgical skill in novices. JSLS. 2008;12:219-26.
- [Google Scholar]
- Using a high-fidelity patient simulator with first-year medical students to facilitate learning of cardiovascular function curves. Adv Physiol Educ. 2012;36:213-9.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of simulation-based teaching of applied physiology of the cardiovascular system on the undergraduate medical student. Natl J Physiol Pharm Pharmacol. 2017;7:328-32.
- [CrossRef] [Google Scholar]
- Available from: https://www.nmc.org.in/wp-content/uploads/2020/01/UG-Curriculum-Vol-I.pdf [Last accessed on 2022 Jan 22]
- An integrated simulation-based early clinical exposure module in cardiovascular physiology. IJPP. 2020;64:147-54.
- [CrossRef] [Google Scholar]
- Introduction of an undergraduate interprofessional simulation based skills training program in obstetrics and gynaecology in India. Adv Simul. 2019;4:6.
- [CrossRef] [PubMed] [Google Scholar]
- Communication skills training through “role play” in an acute critical care course. Natl Med J India. 2021;34:92-4.
- [CrossRef] [PubMed] [Google Scholar]
- Medical simulation-based learning outcomes in pre-clinical medical education. Cureus. 2020;12:e11875.
- [CrossRef] [Google Scholar]
- Large group high-fidelity simulation enhances medical student learning. Med Teach. 2009;31:e206-10.
- [CrossRef] [PubMed] [Google Scholar]
- Improved medical student satisfaction and test performance with a simulation-based emergency medicine curriculum: A randomized controlled trial. Ann Emerg Med. 2009;54:684-91.
- [CrossRef] [PubMed] [Google Scholar]
- Engagement and learning in simulation: Recommendations of the Simnovate Engaged Learning Domain Group. BMJ Stel. 2017;3:S23-32.
- [CrossRef] [Google Scholar]
- Student perception on the integration of simulation experiences into human physiology curricula. Adv Physiol Educ. 2019;43:332-8.
- [CrossRef] [PubMed] [Google Scholar]






