Translate this page into:
Cardiac autonomic function evaluation during the COVID-19 pandemic: A frugal innovation for Valsalva manoeuvre
*Corresponding author: Shival Srivastav, Department of Physiology, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India. drshival@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Arvind A, Srivastav S. Cardiac autonomic function evaluation during the COVID-19 pandemic: A frugal innovation for Valsalva manoeuvre. Indian J Physiol Pharmacol 2021;65(1):66-8.
Dear Sir/Ma’am,
COVID-19 pandemic has been a harbinger of change in medical practice around the world. The primary mode of spread of novel coronavirus is through droplets. In addition, aerosol mode of transmission has also been recently proposed as a potential mode of virus transfer.[1,2] Therefore, donning of personal protective equipment has been made mandatory for medical staff involved in care of COVID-19 patients. This measure is crucial to prevent person-to-person spread of infection.
In our country, we are following guidelines issued by Indian Council of Medical Research for testing of persons suspected of being infected with the virus. The guidelines are dynamic and have evolved with time, as we continue to accrue knowledge about novel coronavirus. Full guidelines are available on the website.[3]
Interestingly, COVID-19 has also emerged as a unique challenge for healthcare workers involved in autonomic function testing. Assessment of cardiac autonomic function is done using a combination of heart rate variability and the battery of tests proposed by Ewing et al.[4] Components of the battery involving exhalation such as deep breathing test (DBT) and Valsalva manoeuvre (VM) may provoke coughing. In addition, performance of deep breathing in the laboratory carries additional risk of aerosol generation, since the manoeuvre entails deep exhalation. Therefore, these factors are important in the context of COVID-19 transmission through aerosols. Hence, there exists a potential risk to the personnel involved in cardiac autonomic function testing. However, it is a well-known fact that avoidance of VM and DBT may preclude the optimal evaluation of parasympathetic reactivity, since calculation of E:I ratio, delta HR and Valsalva ratio indices is not possible in absence of these test components.
VM merits discussion in the context of COVID-19 pandemic. The manoeuvre entails performance of forced expiration maintaining an expiratory airway pressure of 40 mmHg for 15 s. The manoeuvre is used to calculate Valsalva ratio, an index of parasympathetic function. Availability of beat-to-beat blood pressure signal also helps to compute baroreflex sensitivity, an index of baroreflex integrity.[5]
Guidelines proposed by American Autonomic Society for Autonomic function testing during the COVID-19 pandemic recommend the use of disposable mouthpieces, antiviral filters and cleaning antiviral cleaning solutions for performance of VM.[6] However, in the Indian scenario, VM is commonly performed by attaching a disposable mouthpiece to the aneroid sphygmomanometer/ digital pressure transducer. Digital pressure transducers are costly and unavailable at most locations. The use of cleaning solutions carries the risk of damaging digital circuitry inside the transducers. In absence of digital transducers, the next best choice for VM is aneroid sphygmomanometer. Cleaning the tubing and interiors of aneroid manometers is also a cumbersome task. Cleaning, if not done properly, carries the risk of transmission of infection. Due to these issues, it may not be feasible to perform VM for autonomic function testing. Therefore, there is imminent need of a practical solution to aid performance of VM for the purpose of testing.
We propose a simple and frugal innovation to facilitate performance of VM for patients visiting autonomic function testing laboratories during the present pandemic.
The assembly consists of a transparent rubber tube (available as levelling hose in the market) of length of approximately 1.5 m. The same is mounted on a wooden board in a U-shaped configuration. To reduce the cost, a cardboard stand may also be used. The U-shaped limb of the rubber tube is filled with water. To facilitate visibility of the water column, blue/black ink may be added. One end of the rubber tube is connected to a disposable syringe hub for the patient to blow into the tube. A small hole is made into the hub so as to create a small leak and ensure sustained effort throughout the manoeuvre. Markings are made at the baseline level of water column and height required for the patient to blow. Two markings may be made at points equivalent to 30–40 mmHg to provide indicators for the patient. Schematic representation of the equipment is shown in [Figure 1]. Assembled equipment is shown in [Figure 2].
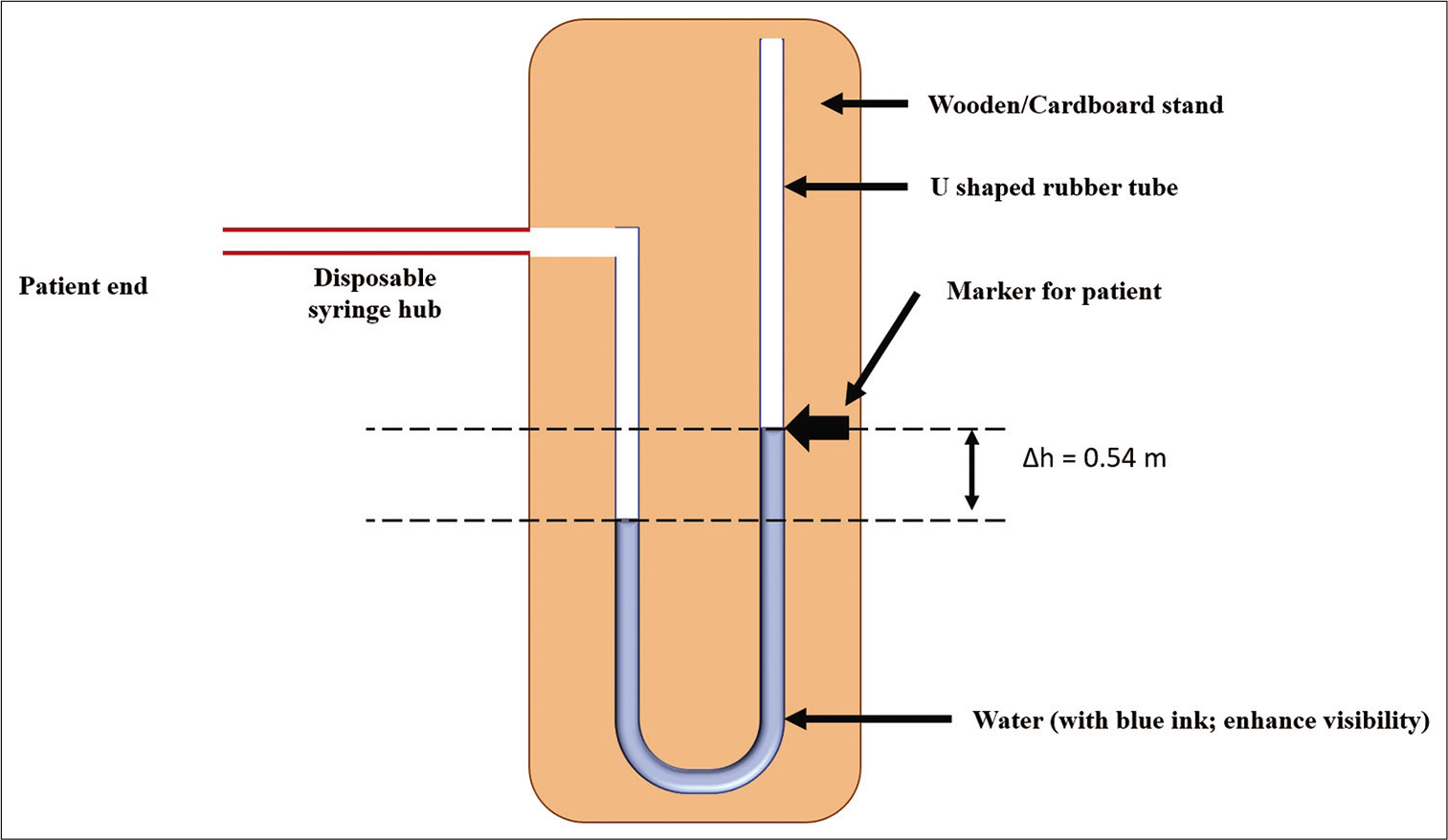
- Schematic representation of the equipment. Schematic representation of the set up. The height difference needed between the two columns for a Valsalva manoeuvre equivalent to 40 mmHg was computed to be 0.54 m and is shown in the figure as Δh.
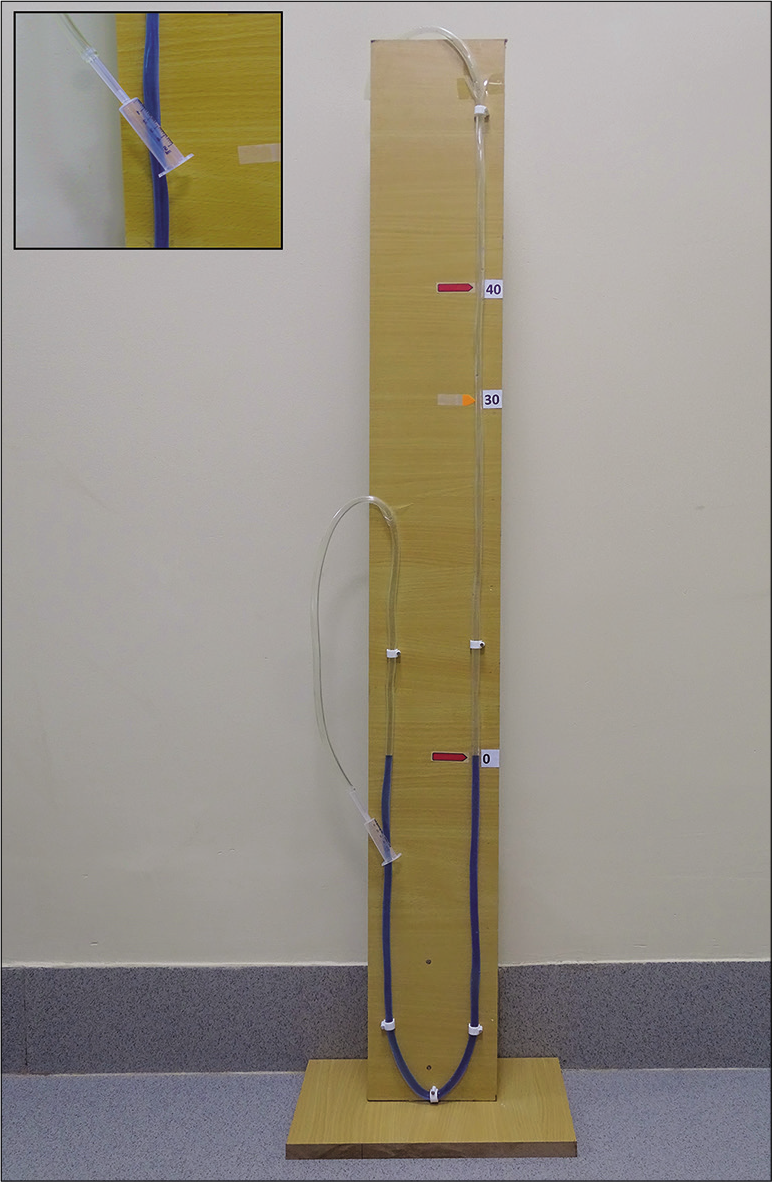
- Assembled setup with disposable syringe hub. The picture shows the assembled equipment filled with water (mixed with blue ink). Disposable syringe hub with a small leak is attached at one end (shown in inset) for the patient to blow into the system. Three markings are made on the board for basal level of water (shown as ‘0’), 30 mmHg and 40 mmHg (shown as ‘30’ and ‘40,’ respectively).
To perform the VM, the patient will be required to blow into the disposable syringe hub connected to the rubber tube to push the water column to a height equivalent to 40 mmHg of mercury. Since we are using a water column, equivalent height of the same needs to be computed. The same can was computed using the formula ρhg, substituting the density of water in place of mercury. Calculation was done using ρ1h1g = ρ2h2g, where ρ1 and h1 are density and height for mercury (13.6 g/ml and 40 cm, respectively) and ρ2 is the density of water and g is the gravitational constant. We calculated h2 and found it to be approximately 0.54 m. Markings were made at points equivalent to 30 mmHg and 40 mmHg, respectively.
After performing the manoeuvre, the tube can be emptied and be rinsed completely using soap/disinfectant solution. The entire tube may be replaced, if need arises without adding much to the cost (tube was available locally at Rs. 10/m length; we used 1.5 m tube length for the assembly). Ink added to water may be prepared in bulk on a daily basis and discarded at the end of the day.
Advantages of the setup are low cost, high visibility and reduced risk of transmission of infection. This frugal innovation may prove to be really useful for autonomic function laboratories serving patients during the present pandemic period. There are some potential disadvantages, which we observed and have tried to address. Addition of ink to water may cause a small change in density. However, this will not have a large impact on VM, as it has been shown that VM performed at lower expiratory pressures (~30 mmHg) may also be used for the estimation of VR and BRS.[5,7] Therefore, minor change in density of the solution due to addition of ink is unlikely to cause an impact on the manoeuvre. The setup is large in size but can be placed near the bedside in autonomic function laboratories as a permanent setup for performance of VM. An important point to be noted in the assembly of the equipment is the nature of the tube material. We chose a rigid transparent tube keeping in mind ease of availability locally, cost constraints and ease of mounting of the tube on the wooden board. The use of a compliant tube should be avoided as it will buffer the expiratory pressure generated leading to higher effort being exerted by the patient to achieve the desired pressure level in the device.
We believe that our frugal innovation may help physiologists continue autonomic function evaluation during the present COVID-19 pandemic without posing additional risk to patients/healthcare personnel. The setup is low cost, easy to disinfect and can be used as a tool for performance of VM.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Consideration of the aerosol transmission for COVID-19 and public health. Risk Anal. 2020;40:902-7.
- [CrossRef] [PubMed] [Google Scholar]
- Protection and disinfection policies against SARS-CoV-2 (COVID-19) Infez Med. 2020;28:185-91.
- [Google Scholar]
- Strategy for COVID-19 Testing in India (Version 6 Dated 04/09/2020) 2020. Indian Council of Medical Research, Department of Health Research, Ministry of Health and Family Welfare, Government of India. Available from: https://www.icmr.gov.in/pdf/covid/strategy/testing_strategy_v6_04092020.pdf [Last accessed on 2020 Sep 24]
- [Google Scholar]
- Diagnosis and management of diabetic autonomic neuropathy. Br Med J (Clin Res Ed). 1982;285:916-8.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of baroreflex responses to lower body negative pressure and Valsalva maneuver in healthy subjects. Indian J Physiol Pharmacol. 2018;62:278-85.
- [Google Scholar]
- Autonomic function testing in the COVID-19 pandemic: An American autonomic society position statement. Clin Auton Res. 2020;30:295-7.
- [CrossRef] [PubMed] [Google Scholar]
- Response variability to stimulus variables during Valsalva maneuver. Indian J Physiol Pharmacol. 1992;36:13.
- [Google Scholar]





