Translate this page into:
Comparative analysis of pulmonary function in school-going adolescents: Examining the impact of depression and anxiety
*Corresponding author: Bhawana Thapa, Department of Physiology, Sikkim Manipal Institute of Medical Sciences, Sikkim Manipal University, Gangtok, Sikkim, India. bhawana.t@smims.smu.edu.in
-
Received: ,
Accepted: ,
How to cite this article: Thapa B, Bhandari SS, Kumar S, Laskar NB, Gupta S. Comparative analysis of pulmonary function in school-going adolescents: Examining the impact of depression and anxiety. Indian J Physiol Pharmacol. 2024;68:149-56. doi: 10.25259/IJPP_572_2023
Abstract
Objectives:
Given the rising concern over depression and anxiety among adolescents, this study aims to investigate their potential impact on respiratory health by comparing pulmonary function test (PFT) parameters between healthy adolescents and those with either depression or anxiety or those exhibiting symptoms of both depression and anxiety.
Materials and Methods:
In this cross-sectional study, a random sample of school-going adolescents aged 13–18 years from various schools in Sikkim, both males and females, were selected. Depression and anxiety were assessed using the Revised Children’s Anxiety and Depression Scale-25, and pulmonary function was measured using a computerised spirometer-Spirolab III. The recorded variables included forced vital capacity (FVC), forced expiratory volume in 1st second (FEV1), FEV1/FVC ratio, peak expiratory flow rate (PEFR) and forced expiratory flow at 25–75% (FEF 25–75%).
Results:
Significant differences emerged in FVC (P = 0.034), PEFR (P = 0.013) and FEF 25–75% (P = 0.023) between healthy and depressed adolescents aged 13–18 years. Similarly, a significant difference was observed in PEFR (P = 0.022) and FEF 25–75% (P = 0.002) between healthy adolescents and those with symptoms of both depression and anxiety. These differences were more pronounced among students in higher grades. Furthermore, significant differences in PEFR (P = 0.015) and FEF 25–75% (P ≤ 0.001) were found while comparing healthy males and males with symptoms of both depression and anxiety. However, no such disparities were seen in girls. There was no significant difference in any of the parameters when compared between the healthy group and those with anxiety.
Conclusion:
Depressed adolescents exhibited significantly reduced FVC, PEFR and FEF 25–75% compared to their healthy counterparts, despite being otherwise healthy. This negative association was more pronounced in the higher age group. However, anxious adolescents did not show any significant difference in PFT compared to healthy peers.
Keywords
Pulmonary Function
Depressive symptoms
Anxiety symptoms
School Students
Adolescents
INTRODUCTION
Depression is a major public health issue and is one of the leading causes of chronic disability in the world. There is evidence that major depression has a joint effect with chronic physical conditions to amplify the functional disability.[1] There are numerous research studies which have observed various disease conditions, including respiratory diseases, to be associated with depression and anxiety. Studies have also shown that the treatment outcome of many respiratory diseases is reduced in the presence of depression. Therefore, it is only relevant to look at this condition from all angles and in all age groups possible. Depression and increased levels of mental health disorders have been found to be associated with decreased lung function in the adult population of the United States.[2] It has been shown to be related to compromised Forced Expiratory Volume in 1st second (FEV1) in the general adult population, even after adjusting for confounding factors.[3] The actual mechanism causing a decline in pulmonary function in depressed populations has not been understood well. However, depression is now being seen as an inflammatory disorder, and many studies to prove its pathophysiology in this direction have been done. Alteration in innate and adaptive immune systems in depression is an established hypothesis.[4] A review paper by Maes et al.[5] has concluded that there is compromised oxidative and antioxidative balance in depressive disorders, leading to oxidative stress and subsequently inflammation. Due to the extensive surface area for the exchange of gases in the lungs, the respiratory system may be more prone to injury caused by oxidative stress, leading to reduced lung function.[6] As respiration is also under voluntary control, different emotions, such as sadness and excitement, affect the rate and depth of respiration. Depression has been found to affect the rate of respiration and the performance of respiratory muscles.[7] Han et al.,[8] in their 8-year follow-up study, found that there was a clear longitudinal association between chronic depression and faster pulmonary function decline among women. Zheng et al.,[9] in their study, concluded that depression and poor lung function are risk factors for each other.
Anxiety disorder is one of the most predominant mental health disorders in adolescents; with a prevalence rate of 20–30% as found by different studies.[10] Major depressive disorder and anxiety are two important causes of disability, especially in women.[11] Many studies have ascertained the association of anxiety with respiratory diseases.[12-14] However, an association between compromised regulation of respiration and anxiety in normal subjects has been scarcely studied. Pine et al.,[15] compared the response to carbon dioxide inhalation in children with and without anxiety disorder. They found a definite hyperresponsiveness in children with anxiety disorder, which indicates dysregulation of respiration in these children.[15,16] A reduced FEV1/FEV was found to be associated with general anxiety.[17]
Evaluation of respiratory functions in individuals with depression and anxiety is an understudied domain in adolescent health. It is hypothesised that there will be a difference in the Pulmonary Function Test (PFT) parameters in healthy, depressed and anxious adolescents. Hence, the objective of this study was to compare the PFT parameters in depressed, anxious and healthy school-going adolescents.
MATERIALS AND METHODS
Study design and setting
This is a cross-sectional was study carried out in Higher Secondary schools coming under the purview of the Education department in the East district of Sikkim between June 2021 and July 2023. The total number of schools in the district is 31, which were enumerated and assigned unique numbers. Through a lottery system, 20% of these schools (n = 6) were randomly selected and invited to take part in the study. One of the selected schools declined to participate, resulting in a total of five participating schools. Out of these, four schools were from four different wards, and one school was from a gram panchayat unit.
Inclusion criteria
All children between the ages of 13 and 18, both male and female, who consented to participate were included in the study.
Exclusion criteria
Smokers, those diagnosed with lung diseases, those not willing to participate in the study, or those who were not able to answer more than three questions out of 25 questions of the questionnaire were excluded from the study. Students with a body mass index (BMI)>30 were also excluded, as obesity negatively affects pulmonary function.
Sample size
It was estimated considering a 40% prevalence of depression in adolescents based on a previous study[17] with a relative error of 10%. The type 1 error was restricted to 5%, that is, at a 95% confidence interval. Considering an attrition rate of 10%, the sample size calculated was 660. The total sample consisted of children between 8th and 12th standard.
Sampling strategy
To ensure representative sampling, the total number of eligible students in each class ranging from class VIII to Class XII within the selected schools were enumerated. Subsequently, 25 students were selected from each class through simple random sampling using a lottery method based on the list of eligible students obtained earlier. In some rural schools with fewer students, probability proportional to size technique was applied to calculate the number of selected students. The height and weight of all the students were recorded, and BMI was calculated. Information on the history of respiratory disease was taken using a standardised pro forma.
A total of 631 students filled up the questionnaire. Out of the total of 631 students, 277 students were excluded because of various reasons, as given in Figure 1. The pro forma was filled in the classroom itself, guided by the investigator. The flow of the participants is given in Figure 1.
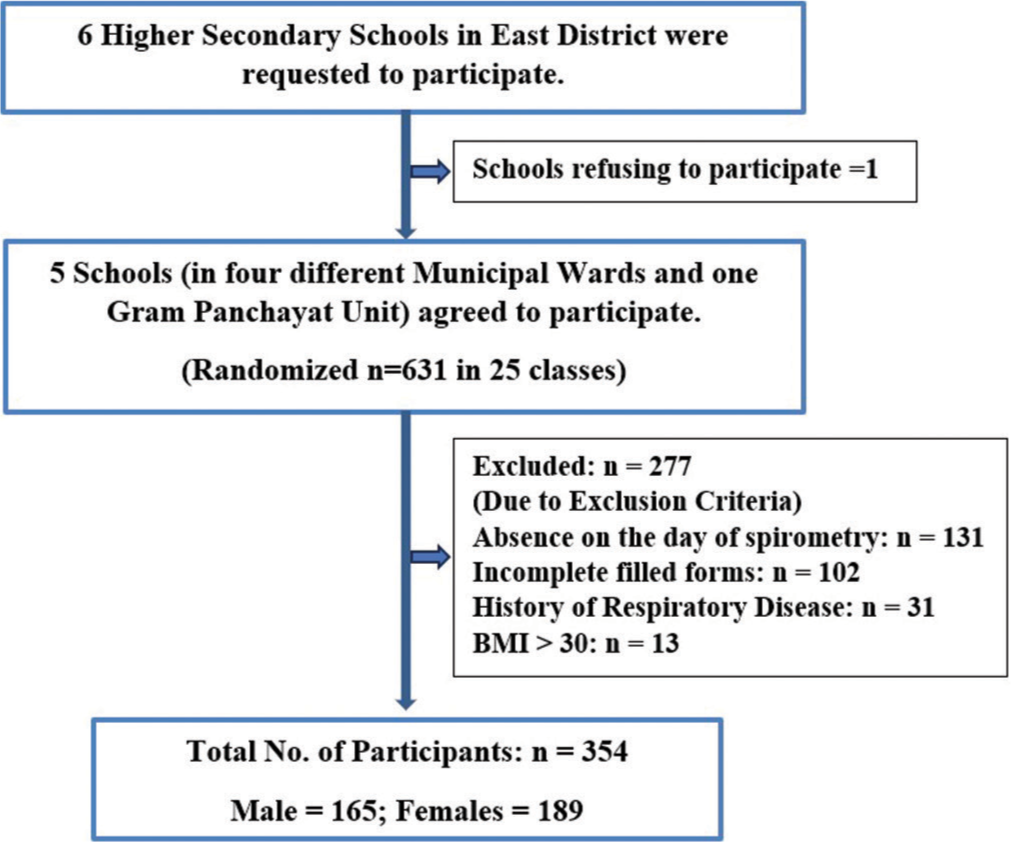
- Flow of participants through the study period. BMI: Body mass index.
Outcome measures
Depression and anxiety assessment tool
The Revised Children’s Anxiety and Depression Scale-25 (RCADS-25) is a 25-question scale that measures levels of anxiety and depression. The scale has two subsets of scales, one for the total anxiety scale and the other for the total depression scale.[18] All questions assess the frequency of symptoms and are rated on a 4-point Likert scale. The total score of the RCADS-25 is calculated by assigning 0–3 to the response categories of ‘never’, ‘sometimes’, ‘often’ and ‘always’, respectively. The sum of all 25 items is tallied and represents the severity of general anxiety and depressive symptoms. Total scores are converted to T-scores using specific equations that have been developed through research and account for the gender and grade of each child. Three sets of T scores are obtained: one for depressive symptoms, one for anxiety symptoms and one for those who have symptoms of both depression and anxiety. Scores between 65 and 70 represent medium severity and are on the borderline clinical threshold, and scores above 70 represent high severity and are above the clinical threshold. The RCADS-25 questionnaire was self-administered and filled out by the investigator as and when necessary for the diagnosis of depression and anxiety.
Students with scores ≥65 on the depression scale were categorised into the depressed group. However, within this group, individuals scoring ≥65 on the anxiety scale were excluded to mitigate the influence of anxiety as a confounding factor. Similarly, students who scored ≥65 on the anxiety scale but <65 on the depression scale were classified as anxious. Those who scored ≥65 on the third set of scores, that is, depression and anxiety scale, were categorised as depressed and anxious.
The subscales of the RCADS-25 have been validated and have acceptable reliability in school-based samples. Studies have shown that it has very good internal consistency and is acceptable to good test-retest reliability.[19,20] The test-retest stability of the RCADS-25 has been found to be acceptable with all intraclass correlation coefficient values of >0.79.[21] RCADS-25 has also been adopted for cross-cultural use.[22-25] In India, it has been developed in Hindi[26] and has been used in a few studies.[27]
PFTs
PFTs were performed as per the guidelines of the American Thoracic Society. A portable computerised spirometerSpirolab III was used. Spirometry was done in the classrooms of each school by the investigator, along with a trained technician. All recordings were taken in standing posture. The variables recorded were Forced Vital Capacity (FVC), FEV1, FEV1/FVC ratio, - Peak Expiratory Flow Rate and Forced Expiratory Flow at 25–75% (FEF 25–75%). As effort exerted by the subject can influence the quality of the spirometry results, clear instructions were given before the test, and the procedure was properly monitored. Further, three recordings were taken from each subject, and the best reading out of the three observations was taken to ensure the reliability of the test results. As the actual recorded values and predicted values of PFT vary with age, height and weight, the percentage of predicted values of PFT has been considered for analysis and comparison. This ensures the standardisation of values.
Data collection procedure
Ethical clearance was obtained from the Institutional Ethics Committee of Sikkim Manipal Institute of Medical Sciences (SMIMS/IEC/2022–148). Written permission was obtained from the Director of school education, Department of Human Resource Development, Government of Sikkim, to conduct the study across various government schools in the state. In private schools, permission was obtained from the principals of the respective schools. The RCADS-25 was used for the assessment of depression. Permission to use the RCADS-25 was obtained from its authors.
Written informed consent was taken from students who were 18 years of age, and consent of teachers and parents for those who were below 18 years, whereby it was clearly mentioned that data confidentiality would be maintained while ensuring the anonymity of the subjects. After this, the process of data collection was started.
Statistical analysis
Descriptive statistics were used to summarise demographic data. The grouped data were subjected to normality tests (Shapiro Wilk’s) accompanied by visual analysis of histograms, based on which the decision was taken to analyse data through parametric and non-parametric tests of comparison. During subgroup analysis, group sizes ≥30 were considered sufficient for the Central Limit Theorem to hold and subject data to parametric analysis.
Independent t-test was used as a parametric test of comparison, and Wilcoxon’s test was used as a non-parametric test of comparison. Comparisons were computed between healthy and each affected group under the domains of depression, anxiety and population experiencing symptoms of both depression and anxiety. The level of significance was set at P < 0.05 and 95% confidence interval. Participants with RCADS scores ≥65 in each category (Depression, Anxiety and both Depression and Anxiety) were considered affected. Subgroup analyses for depression, anxiety and combined depression and anxiety were performed in both genders and two subgroups based on their academic class. The analysis included the percentage of predicted values of PFT. Data analysis was executed using ‘Statistical Package for the Social Sciences software version 20.0’.
RESULTS
A total of 631 students filled the questionnaires with only 354 undergoing spirometry due to various exclusion criteria, as given in Figure 1. Among the participants, 165 (46.61%) were boys and 189 (53.39%) were girls. The mean age of the total population was 15.4 years, with a standard deviation of 1.8, as shown in Table 1. Of the 354 students, 76 (21.47%) exhibited depressive symptoms, 109 (30.79%) showed symptoms of anxiety, and among these, 107 (30.22%) displayed symptoms of both depression and anxiety, as per the scores of RCADS [Table 1]. This indicates a substantial proportion of students experiencing the co-occurrence of depression and anxiety. Further, the analysis revealed that only 25 (7%) students showed symptoms of depression alone and did not show symptoms of anxiety (hereafter referred to as purely depressed), whereas 58 (16%) showed symptoms of anxiety alone and did not show symptoms of depression (hereafter referred to as purely anxious). A comparison of PFT was then made between the healthy group (those who did not show any symptom of depression or anxiety) and these three different groups, namely depressed, anxious and depressed and anxious.
| Total (n=354) | Male (n=165) | Female (n=189) | P | |
|---|---|---|---|---|
| (Mean±SD) | ||||
| Age (years) | 15.4±1.8 | 15.44±1.91 | 15.35±1.69 | 0.662 |
| Height (cm) | 160.31±9.79 | 165.98±8.42 | 155.26±8.02 | <0.001 |
| Weight (kg) | 50.39±9.17 | 53.06±9.94 | 48.01±7.71 | <0.001 |
| Body mass index (kg/m2) | 19.60±3.12 | 19.19±2.89 | 19.97±3.28 | 0.019 |
| n(% of total population) | ||||
| Grade | ||||
| Class VIII–X | 144 (40.68) | 70 (19.77) | 74 (20.90) | |
| Class XI–XII | 210 (59.32) | 97 (27.40) | 113 (31.92) | |
| Depressed | ||||
| Class VIII–X | 14 (3.95) | 3 (0.85) | 11 (3.10) | |
| Class XI–XII | 11 (3.11) | 7 (1.98) | 4 (1.13) | |
| Anxious | ||||
| Class VIII–IX | 36 (10.17) | 20 (5.65) | 16 (4.52) | |
| Class XI–XII | 22 (6.21) | 10 (2.82) | 12 (3.38) | |
| Depressed as well as anxious | ||||
| Class VIII–X | 65 (18.36) | 26 (7.34) | 39 (11.02) | |
| Class XI–XII | 42 (11.86) | 15 (4.24) | 27 (7.62) | |
All values are in mean and SD unless stated otherwise. SD: Standard deviation
There was a significant difference in PFT parameters such as FVC (P = 0.034), PEFR (P = 0.013) and FEF 25–75% (P = 0.023) between the children who had only depression and those who were healthy [Table 2].
| PFT parameters in the percentage of predicted values | Healthy (n=215) | Depressed (n=25) | *U, P |
|---|---|---|---|
| FVC | 87 (73–97) | 79 (56.5–89.5) | −2.121, 0.034 |
| FEV1 | 96 (83–108) | 90 (63.5–102.5) | −1.775, 0.076 |
| FEV1/FVC | 113 (108–115) | 112 (106.5–115) | −0.171, 0.864 |
| PEFR | 84 (65–104) | 61 (46–93) | −2.476, 0.013 |
| FEF (25–75%) | 115 (86–138) | 94 (69–117.5) | −2.280, 0.023 |
All values are in median and inter-quartile range unless stated otherwise, FVC: Forced vital capacity, FEV1: Forced expiratory volume (in 1stsecond), PEFR: Peak expiratory flow rate, FEF (25–75%): Forced expiratory flow at 25–75%, PFT: Pulmonary function test, *U: *Mann-Whitney U test statistic
However, no significant difference was seen in any of the PFT parameters when a comparison was made between the purely anxious group and the healthy cohort.
In the comparative analysis of PFT between the healthy group and those experiencing both depression and anxiety, it was revealed that PEFR (P = 0.022) and FEF 25–75% (P = 0.002) showed significant differences in these groups, as outlined in Table 3.
| PFT parameters in the percentage of predicted values | Healthy (n=215) | Depressed and anxious (n=107) | P |
|---|---|---|---|
| FVC | 86.26±16.9 | 85.14±17.83 | 0.583 |
| FEV1 | 95.55±17.30 | 93.77±19.21 | 0.404 |
| FEV1/FVC | 110.26±9.41 | 108.60±12.79 | 0.190 |
| PEFR | 84.17±6.66 | 76.78±2.20 | 0.022 |
| FEF (25–75%) | 112.96±36.1 | 100.72±27.81 | 0.002 |
All values are in mean and standard deviation unless stated otherwise. FVC: Forced vital capacity, FEV1: Forced expiratory volume (in 1stsecond), PEFR: Peak expiratory flow rate. FEF (25–75%): Forced expiratory flow at 25–75%, PFT: Pulmonary function test
To delve deeper into this, the students were further divided into two subsets for analysis. One subset comprised students from grades VIII to X, while the other included students from grades XI and XII. This division aimed to explore whether the reduction in pulmonary function was age-related and linked to the chronicity of depression and anxiety.
A comparison of PFT was then conducted between the healthy group and those experiencing both depression and anxiety in both subsets. In the subset of students from grades VIII to X, no significant differences were found in any PFT parameter. However, in the subset of students from grades XI and XII, a significant difference was observed in FEV1/FVC (P = 0.012), PEFR (P = 0.008) and FEF 25–75% (P = 0.001), as detailed in Table 4.
| PFT parameters in the percentage of predicted values | Healthy (n=60) | Depressed and anxious (n=42) | P |
|---|---|---|---|
| FVC | 83.8±15.5 | 85.92±20 | 0.551 |
| FEV1 | 94.56±18 | 94.76±21 | 0.961 |
| FEV1/FVC | 113±6.37 | 109.71±6 | 0.012 |
| PEFR | 88.28±27 | 73.70±26 | 0.008 |
| FEF (25–75%) | 117±38 | 96.8±23 | 0.001 |
All values are in the median and interquartile range unless stated otherwise. FVC: Forced vital capacity, FEV1: Forced expiratory volume (in 1stsecond), PEFR: Peak expiratory flow rate, FEF (25–75%): Forced expiratory flow at 25–75%, PFT: Pulmonary function test
The total sample was further stratified into two groups based on gender, and an analysis was conducted to compare pulmonary function between those with both depression and anxiety and the healthy groups in both genders. Notably, a significant difference was observed in PEFR (P = 0.015) and FEF 25–75% (P < 0.001) when the comparison was made among boys, as outlined in Table 5. However, no such difference was noted in girls.
| PFT parameters in the percentage of predicted values | Healthy (n=124) | Depressed and anxious. (n=41) | P |
|---|---|---|---|
| FVC | 87.79±15 | 87.8±19.43 | 0.998 |
| FEV1 | 100.62±17 | 98.17±21 | 0.456 |
| FEV1/FVC | 113.89±4.45 | 112.29±8.53 | 0.254 |
| PEFR | 94.6±23 | 80.3±33.87 | 0.015 |
| FEF (25–75%) | 127.8±29 | 107.14±31.5 | <0.001 |
All values are in median and inter-quartile range unless stated otherwise, FVC: Forced vital capacity, FEV1: Forced expiratory volume (in 1stsecond), PEFR: Peak expiratory flow rate, FEF (25–75%): Forced expiratory flow forced expiratory flow at 25–75%, PFT: Pulmonary function test
DISCUSSION
The primary objective of this study was to explore if there was any relationship between depression and anxiety with pulmonary function in adolescents without any respiratory disease.
In our study, it was seen that FVC, PEFR and FEF 25–75% were significantly lesser in the depressed group than in the healthy group. However, other parameters were not found to be significantly different, which is almost similar to the findings of a study by Peng et al.[28] who, in addition to FVC, also found a negative association of FEV1 with depression. Krommydas et al.[29] found a similar association in asthmatic depressed patients.
However, their study was done on an adult population. As PEFR and FEF 25–75% reduction are early changes and indicate future development of decreased FEV1, it can be thought that the changes seen in the adolescent age group may indicate possibilities of progression to FEV1 reduction after they transition to adulthood. This inference is also supported by our other finding in which it was seen that the negative association of PFT with depression and anxiety was seen in students of higher age groups (Grades XI and XII), and no significant difference was seen in younger age groups (Grade VIII to X).
Goodwin et al.[2] found an association of depression with restrictive lung disease in adults. In our study, a reduction of FVC was seen in the depressed group, which can be compared to the finding of restrictive lung disease.
Han et al. [8], in their 8-year-long longitudinal study, saw that PFT parameters such as FVC, FEV1 and PEFR in depressed women declined much faster compared to women with no signs of depression at baseline assessment. They also found that there was a higher risk of pulmonary disease mortality in women with depressive symptoms than the women who had no depression. No such relation was found in men. This is contrary to our finding as in this study, a significant difference in PEFR and FEF 25–75% was observed when compared between healthy males and males with depression and anxiety, whereas no such difference was seen in females [Table 5].
This difference in findings could be due to the different demography of the population that we studied. Future studies could explore the underlying mechanisms driving these gender-specific differences further.
The findings of Ochs-Balcom et al.[30] is similar to the finding of this study, where they found a negative association between depression and PFT in males, but these males were smokers. This smoking habit could have been the confounding factor affecting lung function rather than depression.
Research suggests that inflammatory processes play a role in the development and progression of depressive symptoms. This, in turn, has been documented as a possible risk factor for a decline in pulmonary function.[31] This was further studied by Lu et al.[32], who found a relation between depression and decline in pulmonary function in older adults, which was, in turn, associated with increased serum levels of proinflammatory markers – Interleukin 6 and C-reactive protein.
Anxiety and obstructive lung disease both have a common symptom of dyspnoea. There are studies in which reported dyspnoea in anxiety is common. Many studies have reported the coexistence of anxiety and respiratory diseases. There is much evidence from community-based studies to suggest a strong association between asthma and anxiety and mood disorders. This association has also been found in the young population by several studies.[2] However, very few studies have assessed the association of anxiety with a measurable decline in lung function in otherwise healthy individuals.
A study by Ho et al.[33] suggests that anxiety was one of the motive causes associated with respiratory symptoms other than lung disease. Spitzer et al.[17] also found an actual quantitative airflow limitation in anxiety and panic disorders. In our study, no significant difference was seen in any of the parameters of PFT between purely anxious and healthy adolescents. As the study by Spitzer et al. was on the general population, future studies could investigate whether these relationships differ across different age groups.[17]
The coexistence of depression and anxiety was found to be common. However, the PFT of the healthy group was also compared with those who had both depression and anxiety. The result was similar to those that were found in purely depressed participants, such as PEFR and FEF 25–75%, which was significantly reduced.
As many studies have shown a negative association between pulmonary function and depression and anxiety in the adult population, analysis was done to see if this relationship was stronger in the higher age groups. On analysis, it was seen that no difference in PFT was observed when a comparison was done between the healthy group and those with depression and anxiety in students of Grades VIII, IX and X. However, there was a significant difference in FEV1/FVC, PEFR and FEF 25–75% when comparison was done between these groups in the subset of students from grades XI and XII. This difference could be related to age, and the reduction in PFT may have become progressively more evident in the older age group.
However, it is important to note that despite the significant reduction in PFT values in the depressed and anxious adolescents as compared to the healthy group, the overall parameters measured remained within the normal range for both groups.
Limitations of the study
While estimating the prevalence, the diagnosis was made on the basis of questionnaire scores and not by interview with a psychiatrist
As there was the coexistence of depression and anxiety in most participants, the number of students who were purely depressed or purely anxious was much less for analysis.
CONCLUSION
The PFT parameters such as PEFR and FEF 25–75% were significantly decreased in depressed adolescents who were otherwise healthy individuals. In higher age group depressed adolescents, FEV1/FVC was also reduced. There was no compromise of lung function in anxious students. A reduction of PEFR and FEF by 25–75% was seen in the group who had symptoms of both depression and anxiety. Therefore, evaluation of lung function in depressed and anxious adolescents and timely intervention may prove beneficial for the lung health of these depressed and anxious adolescents. A longitudinal study in this regard may throw more light on this association.
Ethical approval
The research/study approved by the Institutional Ethics Board at Sikkim Manipal Institute of Medical Sciences, number SMIMS/IEC/2021-05, dated 18th March 2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Joint effect of depression and chronic conditions on disability: Results from a population-based study. Psychosom Med. 2007;69:332-8.
- [CrossRef] [PubMed] [Google Scholar]
- Association between lung function and mental health problems among adults in the United States: Findings from the First National Health and Nutrition Examination Survey. Am J Epidemiol. 2007;165:383-8.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between depression and lung function in the general population in Korea: A retrospective cross-sectional study. Int J COPD. 2018;13:2207-13.
- [CrossRef] [PubMed] [Google Scholar]
- The bidirectional relationship of depression and inflammation: Double trouble. Neuron. 2020;107:234-56.
- [CrossRef] [PubMed] [Google Scholar]
- A review on the oxidative and nitrosative stress (O&NS) pathways in major depression and their possible contribution to the (neuro) degenerative processes in that illness. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:676-92.
- [CrossRef] [PubMed] [Google Scholar]
- Oxidative stress and respiratory system: Pharmacological and clinical reappraisal of N-acetylcysteine. COPD. 2014;11:705.
- [CrossRef] [PubMed] [Google Scholar]
- WHO - Maternal, newborn, child and adolescent health/adolescent development. 2017. Geneva: WHO; Available from: http://www.who.int/maternal_child_adolescent/topics/adolescence/development/en [Last accessed on 2020 Aug 31]
- [Google Scholar]
- Relationships of persistent depressive symptoms with subsequent lung function trajectory and respiratory disease mortality. J Affect Disord. 2022;309:404-10.
- [CrossRef] [PubMed] [Google Scholar]
- Depressive symptoms and chronic lung disease in middle-aged and older Chinese adults: Prospective bidirectional association and mediation analysis. J Affect Disord. 2022;297:283-93.
- [CrossRef] [PubMed] [Google Scholar]
- Global, regional, and national incidence, prevalence, and years lived with disability for 354 Diseases and Injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789-858.
- [CrossRef] [PubMed] [Google Scholar]
- Anxiety and asthma symptoms in urban adolescents with asthma: The mediating role of illness perceptions. J Clin Psychol Med Settings. 2010;17:349-56.
- [CrossRef] [PubMed] [Google Scholar]
- Asthma and anxiety disorders. Adv Psychosom Med. 2003;24:51-71.
- [CrossRef] [PubMed] [Google Scholar]
- Anxiety, depression, and asthma control: Changes after standardized treatment. J Allergy Clin Immunol Pract. 2018;6:1953-9.
- [CrossRef] [PubMed] [Google Scholar]
- Differential carbon dioxide sensitivity in childhood anxiety disorders and nonill comparison group. Arch Gen Psychiatry. 2000;57:960-7.
- [CrossRef] [PubMed] [Google Scholar]
- Ventilatory physiology of children and adolescents with anxiety disorders. Arch Gen Psychiatry. 1998;55:123-9.
- [CrossRef] [PubMed] [Google Scholar]
- Mental health problems, obstructive lung disease and lung function: Findings from the general population. J Psychosom Res. 2011;71:174-9.
- [CrossRef] [PubMed] [Google Scholar]
- Chorpita revised children's anxiety and depression scale user's guide. 2015. Available from: https://www.childfirst.ucla.edu [Last accessed on 2023 Sep 11]
- [Google Scholar]
- Psychometric evaluation of two short versions of the Revised Child Anxiety and Depression Scale. BMC Psychiatry. 2020;20:47.
- [CrossRef] [PubMed] [Google Scholar]
- The revised child anxiety and depression scale 25-parent version: Scale development and validation in a school-based and clinical sample. Assessment. 2017;24:712-28.
- [CrossRef] [PubMed] [Google Scholar]
- A brief questionnaire of DSM-IV-defined anxiety and depression symptoms among children. Clin Psychol Psychother. 2002;9:430-42.
- [CrossRef] [Google Scholar]
- Psychometric properties of the spanish revised child anxiety and depression scale 25-item version in El Salvador. J Psychopathol Behav Assess. 2021;43:271-80.
- [CrossRef] [Google Scholar]
- Translation and adaptation of the revised children's anxiety and depression scale: A qualitative study in Belize. J Adolesc Health. 2023;72:S34-9.
- [CrossRef] [PubMed] [Google Scholar]
- Rapid mental health screening in conflict zones: A translation and cross-cultural adaptation into Arabic of the shortened Revised Child Anxiety and Depression Scale (RCADS-25) Confl Health. 2021;15:51.
- [CrossRef] [PubMed] [Google Scholar]
- Psychometric properties of the Turkish version of the Revised Child Anxiety and Depression Scale-Child Version in a clinical sample. Psychiatr Clin Psychopharmacol. 2017;27:84-92.
- [CrossRef] [Google Scholar]
- Adapting a revised child anxiety and depression scale for rural India: A pilot, amenable to scale up. Available from: https://psyarxiv.com/25pnr [Last accessed on 2023 Sep 16]
- [Google Scholar]
- Feasibility and acceptability of a remote stepped care mental health programme for adolescents during the COVID-19 pandemic in India. Int J Environ Res Public Health. 2023;20:1722.
- [CrossRef] [PubMed] [Google Scholar]
- Association between depressive symptoms and lung function in the United States adults without pulmonary diseases: A cross-sectional study from NHANES. J Affect Disord. 2023;325:787-93.
- [CrossRef] [PubMed] [Google Scholar]
- Depression and pulmonary function in outpatients with asthma. Respir Med. 2004;98:220-4.
- [CrossRef] [PubMed] [Google Scholar]
- The association of depressive symptoms and pulmonary function in healthy adults. Psychosom Med. 2013;75:737-43.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease. JAMA. 2013;309:2353-61.
- [CrossRef] [PubMed] [Google Scholar]
- Systemic inflammation, depression and obstructive pulmonary function: A population-based study. Respir Res. 2013;14:53.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship of anxiety and depression with respiratory symptoms: Comparison between depressed and non-depressed smokers in Singapore. Int J Environ Res Public Health. 2019;16:163.
- [CrossRef] [PubMed] [Google Scholar]






