Comparison of adverse effects of trastuzumab with other drug combinations for the treatment of breast cancer: A review
*Corresponding author: Rajani Mathur, Delhi Pharmaceutical Sciences and Research University (DPSRU), New Delhi, 110017, India. mathurajani@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar D, Basu S, Goyal RK, Sahoo PK, Mathur R. Comparison of adverse effects of trastuzumab with other drug combinations for the treatment of breast cancer: A review. Indian J Physiol Pharmacol 2022;66:1-15.
Abstract
Objectives:
This study compares the adverse effects (AEs) associated with trastuzumab in the treatment of human epidermal growth factor receptor 2-positive breast cancer (HER-2 + BC) when used alone or in combination with chemotherapy or with tyrosine kinase inhibitors, so as to aid in rational treatment choices.
Materials and Methods:
An electronic search was conducted on PubMed using the Mesh terms ‘BC’, ‘HER-2 positive’, ‘metastasis BC, ‘trastuzumab’, and ‘safety’. Data from 32 studies regarding AEs were extracted and categorised as trastuzumab + chemotherapy (T+C), trastuzumab biosimilar (Tb), trastuzumab + tyrosine kinase inhibitors+ chemotherapy (T+TKi+C), and trastuzumab + tyrosine kinase inhibitors (T+TKi). The data are presented as the mean percentage of AEs. The statistical comparison was represented by a box and whisker plot of the interquartile range value of AEs.
Results:
AEs related to the gastrointestinal tract, skin, nervous, blood, and lymph were reported to be the most common in T+C, T+TKi+C, and T+TKi. Nausea, vomiting, diarrhoea, constipation, neuropathy peripheral, alopecia, rash, anaemia, leucopenia, raised aspartate transaminase and alanine transaminase were the most common complaints. AEs such as myalgia, nasopharyngitis, hypertension, and ejection fraction decrease was reported to be the most common in Tb.
Conclusion:
This study concluded that biosimilar of trastuzumab is safest for the treatment of HER-2-positive BC. Cardiovascular disorder is often reported in the biosimilar group, but this group has fewer AEs reported as compared with chemotherapy, and tyrosine kinase inhibitors groups related to other systems such as digestive, nervous, and respiratory. The choice of combination is depending on the type of BC and the condition of the patients. The patients must monitor for cardiotoxicity when the biosimilar of trastuzumab is used.
Keywords
Adverse effects
Trastuzumab
Tyrosine kinase inhibitor
HER-2-positive
Metastatic breast cancer
INTRODUCTION
Breast cancer (BC) is the most common cancer among women.[1] In 2017, more than 250,000 new cases of BC were discovered in the United States, and it is estimated that 12% of all women in the US will be diagnosed with BC at some point in their lives. About 62% of BC are restricted to the breast at the time of diagnosis, while another 31% have progressed to lymph nodes around the breast.[2]
The BC accounts for 14% of all cancers in Indian women. One woman gets diagnosed with BC every 4 min in India and one woman dies of BC every 13 min, making it the most prevalent cancer among women.[3] In 2018, about 162,468 new registered cases of BC and 87,090 deaths were recorded in the country. By 2030, BC is expected to cause more deaths among women in India than any other cancer.[4]
HER-2 is a tyrosine kinase receptor that facilitates signalling pathways of cell growth, division, motility, and repair in normal cells.[5] Overexpression of HER-2 activates the phosphatidylinositol 3-kinase/protein kinase B (PI3K/Akt) ‘survival pathway’ whose action favours cell proliferation apparently by inhibiting apoptosis.[6] The ‘survival’ signal is normally coupled to the activation of the mitogenic signal involving mitogen-activated protein kinases (MAPK) pathway recruitment. Increased HER-2 expression in cancer enhances and prolongs signalling from both the PI3K/Akt and MAPK pathways, associating upregulation of HER-2 to the BC.[7]
Patients with HER-2 Positive BC are given treatment before surgery to reduce the tumor size and the neoadjuvant therapy after surgery to prevent the reoccurance of BC. Various treatments for these are chemotherapy,target therapy like tyrosine kinase inhibitors , hormonal therapy like PI3K/Akt/mTOR inhibitors (everolimus), CDK4/6 inhibitors, antiPD(L)1(programmed cell death protein ligand 1) antibodies, endocrine therapy.[8] The treatment is recommended to start within 2–6 weeks after the surgery.[9]
Trastuzumab is a recombinant humanised IgG1 monoclonal antibody against the extracellular domain of the HER-2 receptor (ErbB-2). The HER-2 receptor consists of an extracellular ligand-binding domain, a transmembrane region, and an intracellular or cytoplasmic tyrosine kinase domain. Trastuzumab binds to the extracellular domain of HER-2 and prevents cleavage of the extracellular domain of HER-2 and thereby activation of the receptor; blocking the dimerization of HER-2. By binding to the juxta membrane domain of HER-2, trastuzumab triggers the downregulation of HER-2 expression.[10] It may be administered by a 3-week cycle (i.e., the initial dose of 8 mg/kg, followed by 6 mg/kg every 3 weeks) or by a weekly cycle (i.e., initial dose of 4 mg/kg, followed by 51 further weekly doses of 2 mg/kg) and sequentially or concurrently with standard chemotherapy of anthracycline-taxane regimens (e.g., doxorubicin and cyclophosphamide [AC] plus paclitaxel/docetaxel or fluorouracil, epirubicin and cyclophosphamide plus docetaxel/paclitaxel), taxane regimen (e.g., docetaxel plus cyclophosphamide) or anthracycline regimen (e.g., AC). Trastuzumab is currently available as 150 mg (single-dose vial) and 440 mg (multidose vial) powder for concentrate solution for intravenous infusion and for subcutaneous injection containing 600 mg/5 mL. Most often, combinations of 2 or 3 of these drugs are used as adjuvant or neoadjuvant therapy.[11]
There are scattered reports of adverse effects (AEs) with trastuzumab or chemotherapy with or without tyrosine kinase inhibitors and a comparative analysis of the safety of trastuzumab with the different treatment regimens is not available. This is essential as it can assist clinicians to make the rational treatment choice that can improve the quality of life and safety of the patient. Hence, to address this, we have compared the safety profile of chemotherapy drugs and TKi with trastuzumab in a single study present in this systematic review and meta-analysis.
MATERIALS AND METHODS
Search strategy
A literature search of databases was conducted on PubMed using MeSH terms ‘BC’, ‘HER-2 positive’, ‘metastasis BC’, ‘adjuvant’, ‘neoadjuvant’, ‘trastuzumab’, ‘efficacy’, and ‘safety’ from the first available year until December 2020. The websites of the American and European societies were searched for BC meetings for relevant presentations, abstracts, and references to related reviews. Only human studies in English were evaluated, as well as randomised control trials (RCTs), observational studies, and clinical trials.
Inclusion criteria
We had included all the studies of Phases-I, II, III, and IV RCTs of HER-2-positive BC in which Tb and trastuzumab were used with and without chemotherapy and TKi.
Exclusion criteria
The following were the criteria for exclusion: Review articles, articles without relevant data (study protocol article, diseases other than BC, a study conducted in healthy subjects and without access), and studies of experimental monoclonal antibodies (mAbs).
Data extraction
The following data were extracted from each study on Microsoft Excel: The first author’s name, publication year, study design, number of patients, receptor status, trastuzumab dosage, chemotherapy regimen, mean age, stage, country, and AEs.
The studies which are included in this meta-analysis are categorised into six different categories as follows:
| S. No. | Category | Number of studies |
|---|---|---|
| 1. | Trastuzumab + chemotherapy | 11 |
| 2. | Trastuzumab biosimilar | 8 |
| 3. | Trastuzumab + chemotherapy + tyrosine kinase inhibitors | 4 |
| 4. | Trastuzumab + tyrosine kinase inhibitors | 9 |
Statistics
The data are presented as the mean percentage of AEs. The statistical comparison was done using GraphPad Prism version 8.4.2. The interquartile range (IQR) is presented in a box and whisker plot, plotted between % of AEs versus drug therapy.
Study selection flow
There were 275 articles found in the PubMed database after an electronic search. Their titles and abstracts were carefully examined and 207 were eliminated based on the methodology section’s exclusion criteria. The whole text of the remaining 68 papers was reviewed for eligibility, while 43 were excluded due to the usage of trastuzumab in combination with other mAbs. Finally, 32 studies were included in this meta-analysis which was grouped [Figure 1].

- Flowchart of study.
RESULTS
Characteristics of studies
Most of the selected articles were published in the years 2016, 2017, and 2019 and belonged to Phases II and III of clinical trials. Most of the studies were multinational or conducted in the United States. The sponsors and partners in six research have not been revealed. One of the 32 studies was funded by a government body, while the rest were funded by private organisations.
Demographics and disease characteristics
The included 32 studies had a total of 12107 patients. Most of the studies are related to metastatic BC and HER2 + Stages II and III. Some of the patients were of followed up patients with ages between 30 and 80 years. The patient received trastuzumab with chemotherapy(n = 4500), or trastuzumab biosimilar (2417), or trastuzumab with tyrosine kinase inhibitors and chemotherapy (n = 719 ) or trastuzumab with tyrosine kinase inhibitors (n = 4471). The baseline characters of all the studies are shown [Table 1].[12-43]
| Disease stage | Number of patient (n) | Pre-menopausal patient (%) | Post-menopausal patients (%) | ER/PR receptor | Mean age (Years) | |
|---|---|---|---|---|---|---|
| Positive patients (%) | Negative patients (%) | |||||
| T+C | ||||||
| HER-2 + Stages I–III invasive | 50 | 38 | 62 | 50 | 50 | 58 |
| HER-2 + primary BC | 50 | 68.0 | 40.0 | NA | NA | 50 |
| HER-2 + advanced BC | 719 | NA | NA | 44.8 | 56.6 | 53.0 |
| HER-2 + MBC trastuzumab resistant | 59 | NA | 35 | 7 | 2 | 52 |
| Metastatic or locally advanced HER-2-positive BC | 26 | 23.1 | 69.2 | NA | NA | 50.7 |
| HER-2 + early or locally advanced BC | 30 | NA | NA | 56.7 | 43.3 | 48 |
| Stage II or III HER-2 + BC | 109 | 50 | 50 | 44 | 56 | 40 |
| Phase III randomised short-HER study | 1254 | 36 | 64 | 68 | 32 | 55 |
| HER-2 + early BC | 2174 | 33 | 67 | 66 | 66 | 56 |
| HER-2 + operable BC | 29 | 58.6 | 41.4 | 48.3 | 51.7 | 56 |
| Tb | ||||||
| HER-2 + BC | 379 | 49.5 | 61.7 | 13.6 | 56.5 | |
| Pre-treated HER-2 + locally recurrent or MBC | 73 | NA | 53 | 47 | 58 | |
| Stages I–IIIA operable HE-R+ BC | 271 | NA | 57 | 43 | 51.8 | |
| HER-2 + early BC | 1510 | NA | NA | NA | 53 | |
| Previously treated HER-2 + BC | 184 | 954.1 | 37.0 | 32.8 | 55 | |
| T+TKi+C | ||||||
| HER-2 + MBC | 474 | 42 | 58 | 66.5 | 33.3 | 52 |
| HER-2+ BC | 245 | NA | NA | 50 | 59 | 55 |
| T+TKi | ||||||
| HER-2 + MBC | 1646 | 47 | 53 | 29.22 | 20.77 | 52 |
| HER-2 + unresectable, locally advanced or MBC | 496 | NA | NA | 53 | 45 | 53 |
| HER-2+ BC | 69 | NA | NA | 39 | 60 | 55.5 |
| HER-2 + MBC patients previously treated | 115 | 63.5) | 36.5 | NA | NA | 59.8 |
NA: Not available, ER: Oestrogen, PR: Progestogen, BC: Breast cancer, MBC: Metastatic breast cancer, F: Women, HER-2: Human epidermal growth factor receptor-2, T+C: Trastuzumab + chemotherapy, Tb: Trastuzumab biosimilar, T+TKi+C: Trastuzumab + tyrosine kinase inhibitors+ chemotherapy, T+TKi: Trastuzumab + tyrosine kinase inhibitors
AEs
The reported AEs from each of the groups were categorised according to the system organ class (SOC). The reported AEs were subcategorised such as nausea, vomiting, thrombocytopenia, pharyngitis, nasopharyngitis, headache, hypertension, raised alanine transaminase (ALT), or aspartate transaminase (AST), and injection site reaction.
General disorders and administration site conditions
Fatigue, asthenia, peripheral oedema, pyrexia, and mucosal inflammation were the most common general disorders.
The mean percentage of patients that reported general disorders and administration site conditions are mentioned [Table 2]. The IQR is shown [Figures 2a-d].
| Mean% of patients | T+C | Tb | T+TKi+C | T+TKi |
|---|---|---|---|---|
| General disorders and administration site conditions | ||||
| Fatigue | 18.65 | 11.08 | 34.2 | 28.18 |
| Asthenia | 12.3 | 1.1125 | 0 | 2 |
| Pyrexia | 3.61 | 4.5 | 2.95 | 2.22 |
| Peripheral oedema | 2.6 | 0 | 5.875 | 0 |
| Skin and subcutaneous tissue disorders | ||||
| Alopecia | 25.19 | 8.0125 | 6.025 | 15.37 |
| Rash | 13.58 | 2.9 | 11.225 | 7.11 |
| Pruritus | 5.07 | 0 | 2.95 | 0 |
| Palmar-plantar erythrodysesthesia | 1.2 | 0 | 16.175 | 1.22 |
| Gastrointestinal disorders | ||||
| Diarrhoea | 9.1 | 43.2 | 29.21 | 42.05 |
| Nausea | 18.73 | 25.44 | 28.61 | 26.675 |
| Vomiting | 12.22 | 12.26 | 15.45 | 8.825 |
| Constipation | 8.57 | 3.11 | 10.61 | 6.175 |
| Stomatitis | 2 | 2.33 | 8.18 | 7.35 |
| Abdominal pain | 2.1 | 2.97 | 0.97 | 2.95 |
| Anorexia | 4.16 | 1.58 | 10 | 4.3 |
| Dyspepsia | 0 | 0 | 2.11 | 4.4 |
| Oral mucositis | 0 | 0 | 1.98 | 6.9 |
| Abdominal pain upper | 2.1 | 2.97 | 0.97 | 2.95 |
| Nervous system disorders | ||||
| Headache | 3.9 | 6.91 | 7.44 | 2.95 |
| Neuropathy peripheral | 9.93 | 0 | 8.43 | 0 |
| Peripheral sensory neuropathy | 12.85 | 3.46 | 3.17 | 0 |
| Dizziness | 1.71 | 0 | 2.44 | 0 |
| Musculoskeletal and connective tissue disorders | ||||
| Muscle spasms | 0 | 0 | 1.22 | 2.95 |
| Pain in extremity | 1.06 | 0 | 2.33 | 0 |
| Arthralgia | 8.57 | 0 | 10.3 | 0 |
| Myalgia | 7.99 | 33.3 | 4.86 | 0 |
| Back pain | 1.01 | 0 | 1.66 | 0 |
| Infections and infestations | ||||
| Paronychia | 0 | 0 | 13.57 | 3.44 |
| UTI | 0 | 0 | 5.87 | 1.64 |
| Injection site pain | 0 | 0 | 0 | 0 |
| Upper respiratory tract infection | 0 | 0 | 1.47 | 1.33 |
| Nasopharyngitis | 4.12 | 1.11 | 2.45 | 0 |
| Infusion-related reaction | 2.76 | 0.4 | 1.45 | 0 |
| Respiratory, thoracic and mediastinal disorders | ||||
| Epistaxis | 11.375 | 2.77 | 2.64 | 7.9 |
| Cough | 5.83 | 3.11 | 6.2 | 2.95 |
| Metabolism and nutrition disorders | ||||
| Decreased appetite | 5.58 | 7.625 | 5.66 | 8.82 |
| Hypokalaemia | 0 | 6.25 | 1.58 | 8.82 |
| Hyponatremia | 0 | 0 | 0.53 | 3.45 |
| Hypocalcaemia | 0 | 0 | 0.53 | 1.72 |
| Eye disorders | ||||
| Dry eye | 0 | 0 | 4.4 | 0 |
| Psychiatric disorders | ||||
| Depression | 3.81 | 0 | 1.775 | 0 |
| Insomnia | 2.9 | 0 | 0 | 1.55 |
| Anxiety | 3.81 | 0 | 0 | 0 |
| Blood and lymphatic system disorders | ||||
| Anaemia | 5.92 | 13.25 | 33.77 | 11.2 |
| Leucopenia | 0.32 | 9.75 | 6.79 | 10.37 |
| Neutropenia | 7.6 | 14.54 | 27.47 | 16.75 |
| Thrombocytopenia | 10.18 | 4.38 | 12.06 | 0 |
| Investigational disorder | ||||
| Raised AST | 8.96 | 13.81 | 17.25 | 25.45 |
| Increase WBC | 6.81 | 1.64 | 0 | 0 |
| Raised ALT | 5.97 | 9.87 | 17.6 | 28.32 |
| ALP increased | 1.81 | 0 | 9 | 1 |
| Blood bilirubin increased | 8.33 | 1.08 | 0 | 1.51 |
| Increase neutrophil count | 1.99 | 0 | 1.77 | 0 |
| Cardiovascular disorders | ||||
| Cardiac disorder | 2.38 | 1.14 | 0 | 0 |
| LSVD increase | 0.42 | 0.48 | 0 | 0 |
| Congestive heart failure | 0 | 0 | 0 | 0 |
| Left ventricular dysfunction | 0 | 0 | 0 | 0 |
| Palpitation | 0 | 0 | 0 | 0 |
| Hypertension | 0.375 | 1.01 | 0 | 0 |
| Hot flush | 0 | 0 | 0 | 0 |
| Palpitations | 0 | 0 | 0 | 0 |
| Reference | 12–22 | 23–30 | 31–34 | 35–41 |
n: Total patients, LSVD: Left ventricle systolic dysfunction, UTI: Urinary tract infection, AST: Aspartate transaminase, ALT: Alanine transaminase, WBC: White blood cell, AEs: Adverse effects
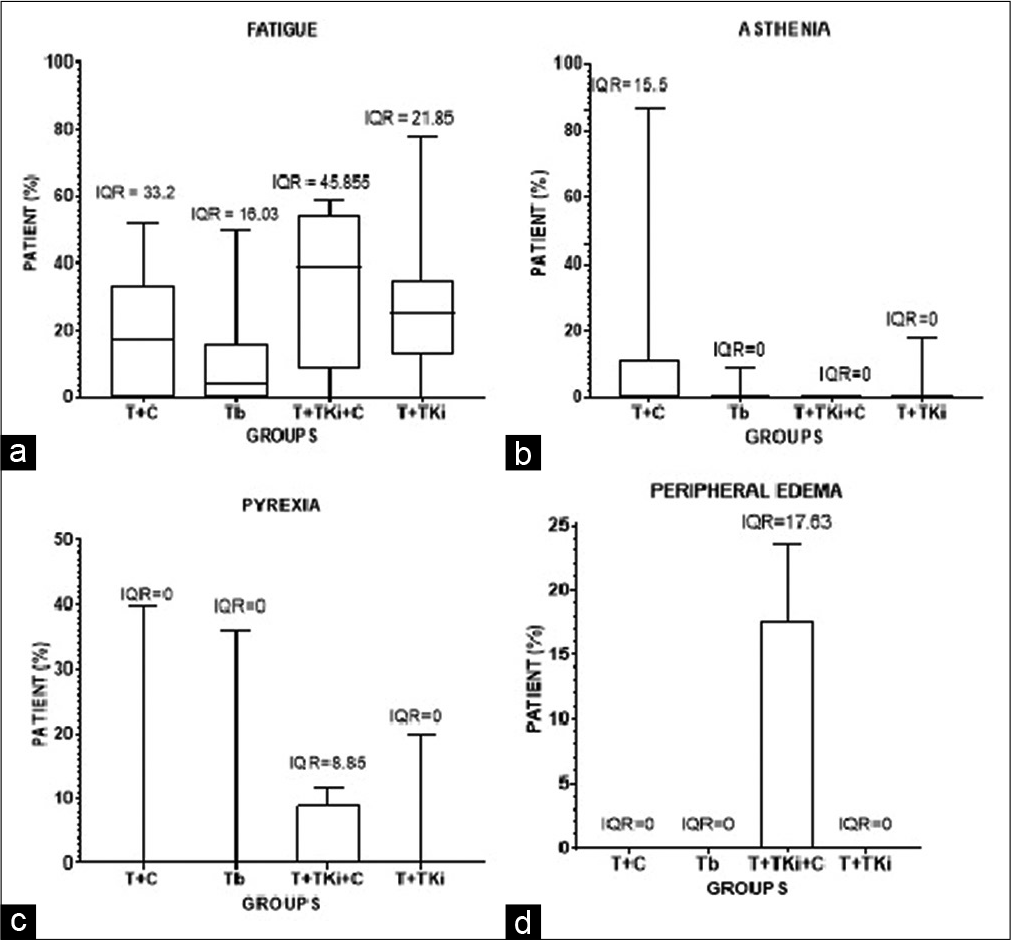
- Box and whisker representation of the range of patients in different groups showing (a) fatigue, (b) asthenia, (c) pyrexia and (d) peripheral oedema.
Skin and subcutaneous tissue disorders
Alopecia, rash, nail disorder pruritus, palmar-plantar erythrodysesthesia, dry skin, and skin discolouration were the most common skin disorders.
The mean percentage of patients that reported skin and subcutaneous tissue disorders are mentioned [Table 2]. The IQR is shown [Figures 3a-e].

- Box and whisker representation of the range of patients in different groups showing (a) fatigue, (b) asthenia, (c) pyrexia, (d) peripheral oedema and (e) palmar-plantar erythrodysesthesia.
Gastrointestinal disorders
Diarrhoea, nausea, vomiting, constipation, anorexia, and abdominal pain were the most common GI disorders.
The mean percentage of patients that reported gastrointestinal disorders are mentioned [Table 2]. The IQR is shown [Figures 4a-h].
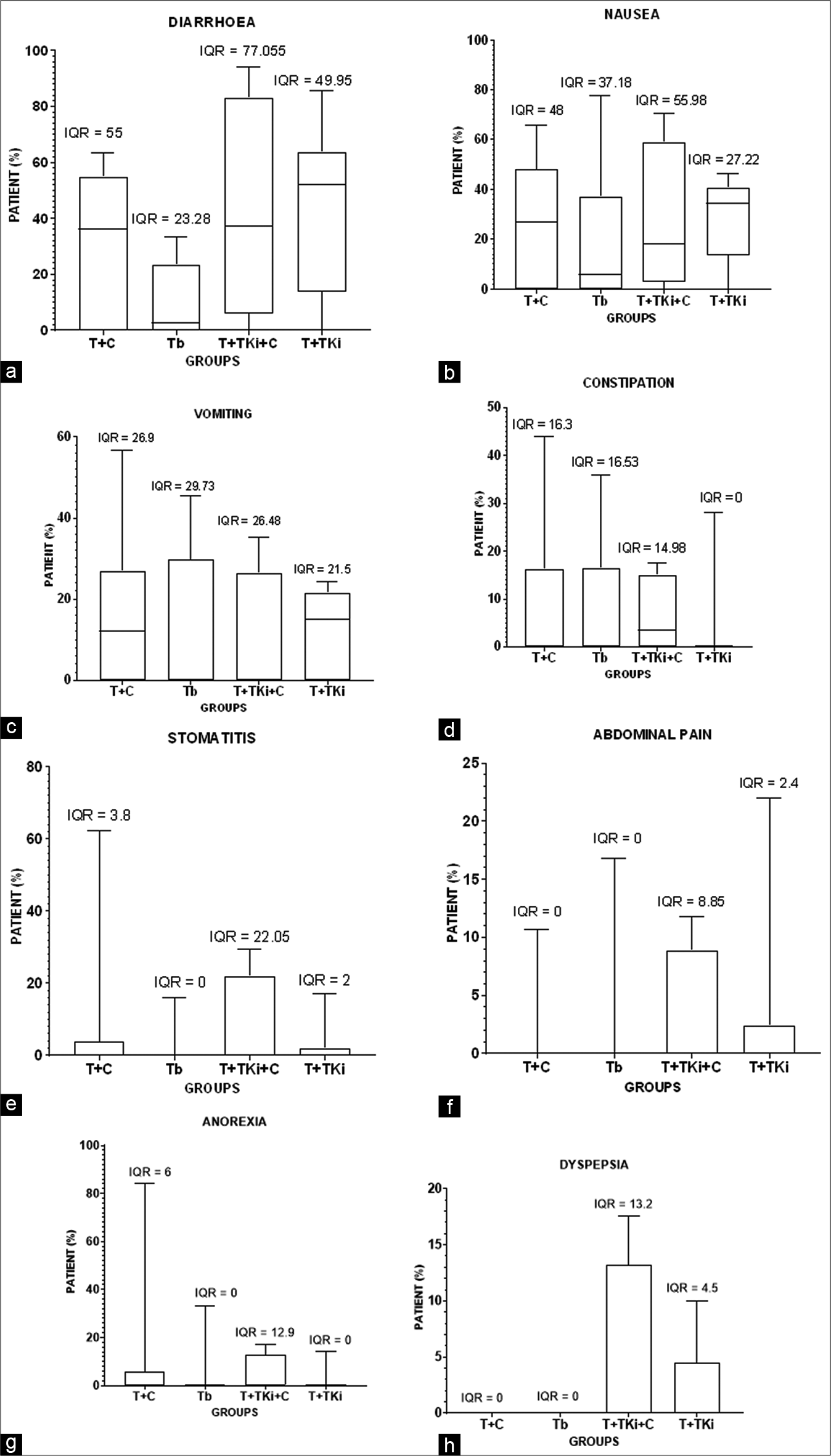
- (a and b) Box and whisker representation of the range of patients in different groups showing (a) diarrhoea, (b) nausea, (c) vomiting, (d) constipation, (e) stomatitis, (f) abdominal pain, (g) anorexia and (h) dyspepsia.
Nervous system disorders
Headache, neuropathy peripheral, peripheral sensory neuropathy, sensory neuropathy, and dizziness were the most common reported nervous system disorders.
The mean percentage of patients that reported nervous system disorders are mentioned [Table 2]. The IQR is shown [Figures 5a-d].

- Box and whisker representation of the range of patients in different groups showing (a) headache, (b) peripheral neuropathy, (c) peripheral sensory neuropathy and (d) dizziness.
Musculoskeletal and connective tissue disorders
Muscle spasms, pain in the extremity, arthralgia, and myalgia were the most common musculoskeletal and connective tissue disorders.
The mean percentage of patients that reported musculoskeletal and connective tissue disorders are mentioned [Table 2]. The IQR is shown [Figures 6a-d].
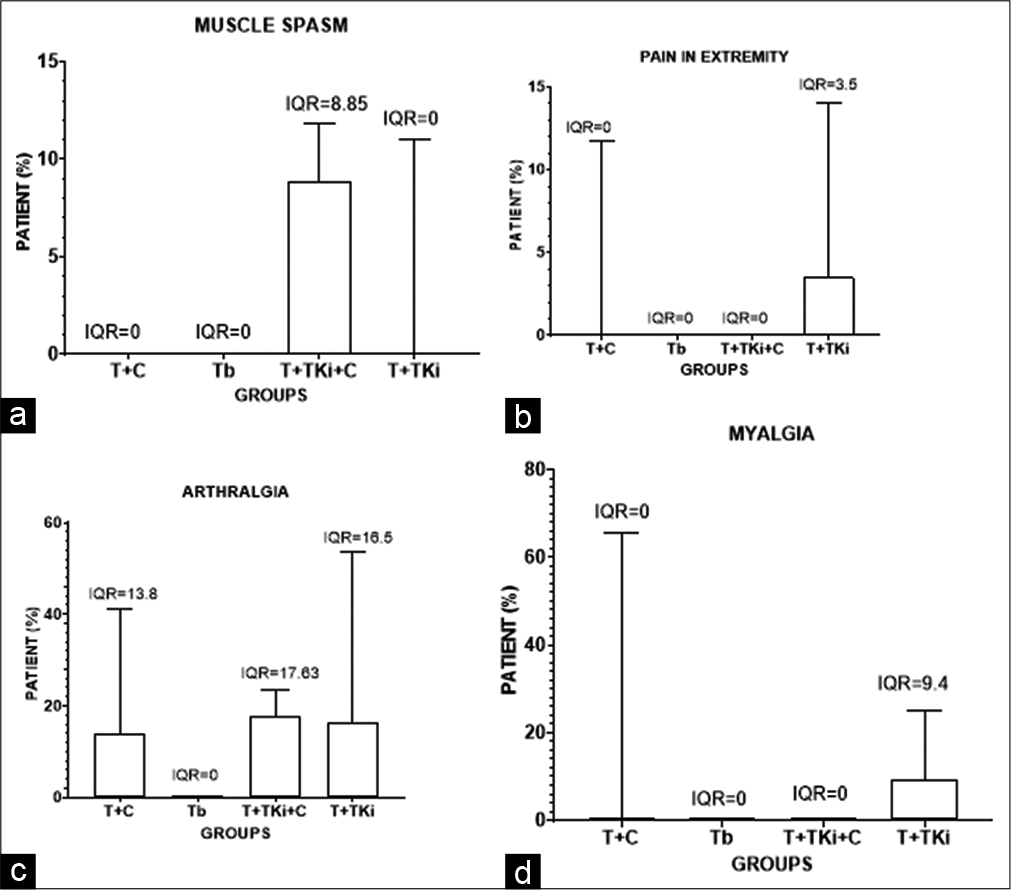
- Box and whisker representation of the range of patients in different groups showing (a) muscle and spasm, (b) pain in extremity, (c) arthralgia and (d) myalgia.
Infections and infestations disorder
Paronychia, urinary tract infection, injection site pain, upper respiratory tract infection, nasopharyngitis, and infusion-related reaction were the most common infections and infestations disorders.
The mean percentage of patients that reported infections and infestations disorders are mentioned [Table 2]. The IQR is shown [Figures 7a-d].
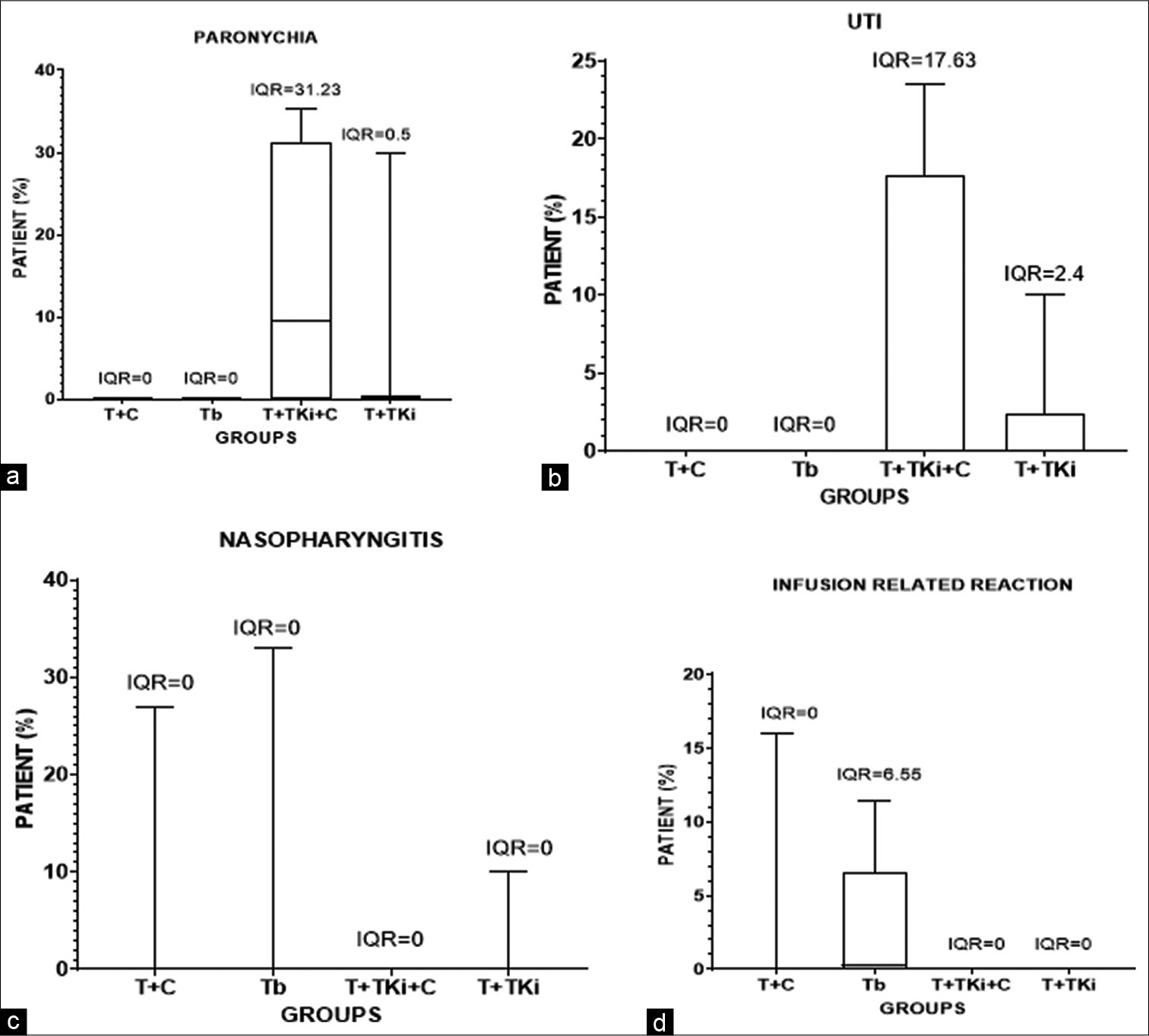
- Box and whisker representation of the range of patients in different groups showing (a) paronychia, (b) UTI, (d) nasopharyngitis and (d) infusion-related reaction.
Respiratory, thoracic, and mediastinal disorders
Dyspnoea, epistaxis, and cough were the most common respiratory, thoracic and mediastinal disorders.
The mean percentage of patients that reported respiratory, thoracic, and mediastinal disorders are mentioned [Table 2]. The IQR is shown [Figures 8a-c].
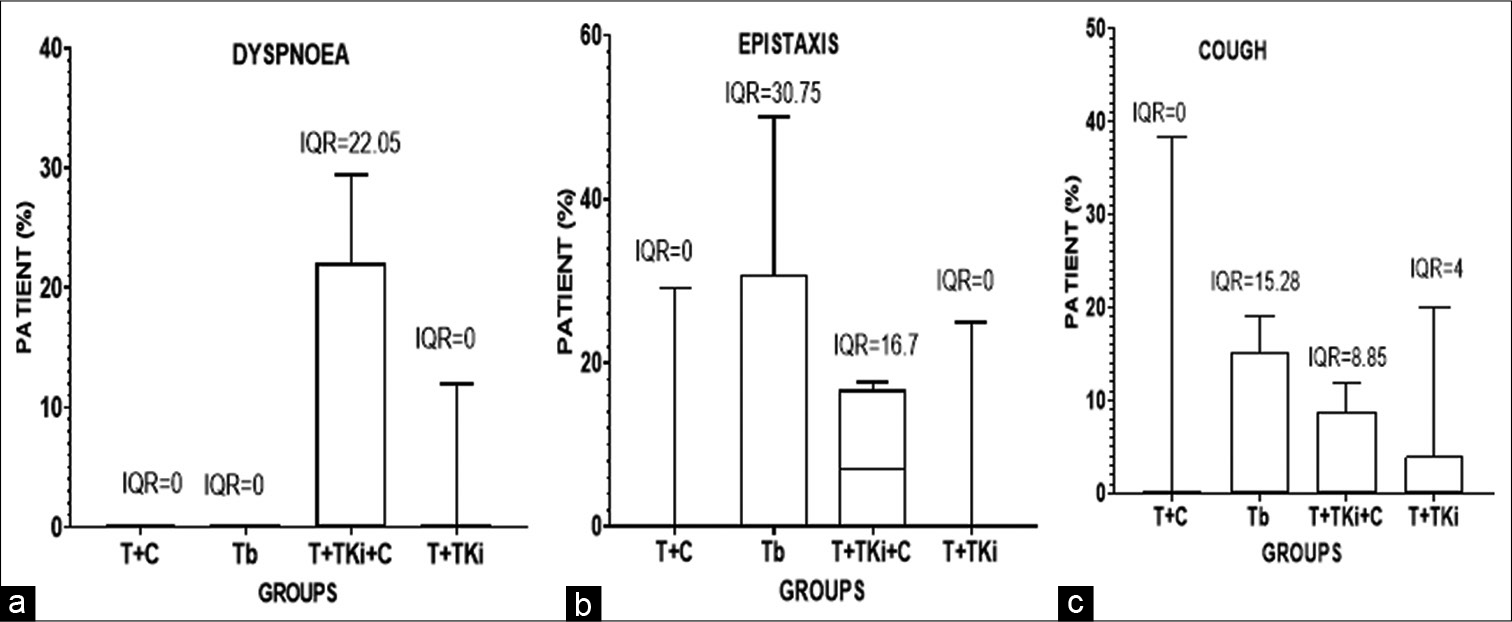
- Box and whisker representation of the range of patients in different groups showing (a) dyspnoea, (b) epistaxis and (c) cough.
Metabolism and nutrition disorders
Decreased, hypokalaemia, hyponatremia, hypocalcaemia, and hypomagnesaemia were the most common metabolism and nutrition disorders.
The mean percentage of patients that reported metabolism and nutrition disorders are mentioned [Table 2]. The IQR is shown [Figures 9a-d].
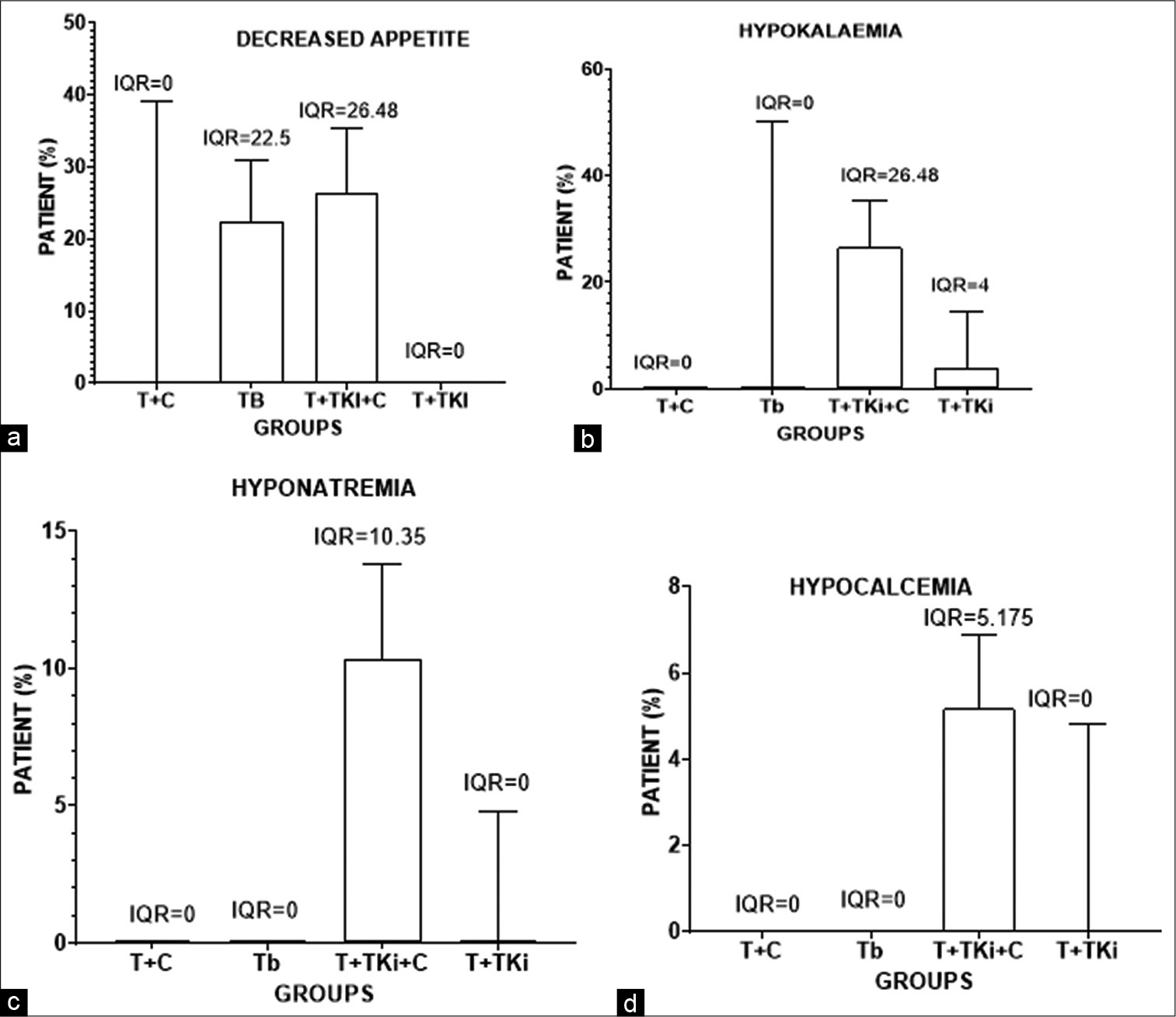
- Box and whisker representation of the range of patients in different groups showing (a) decreased appetite, (b) hypokalaemia, (c) hyponatremia and (d) hypocalcaemia.
Eye disorders
Dry eye was a common eye disorder.
The mean percentage of patients that reported these eye disorders are mentioned [Table 2]. The IQR is shown [Figure 10].
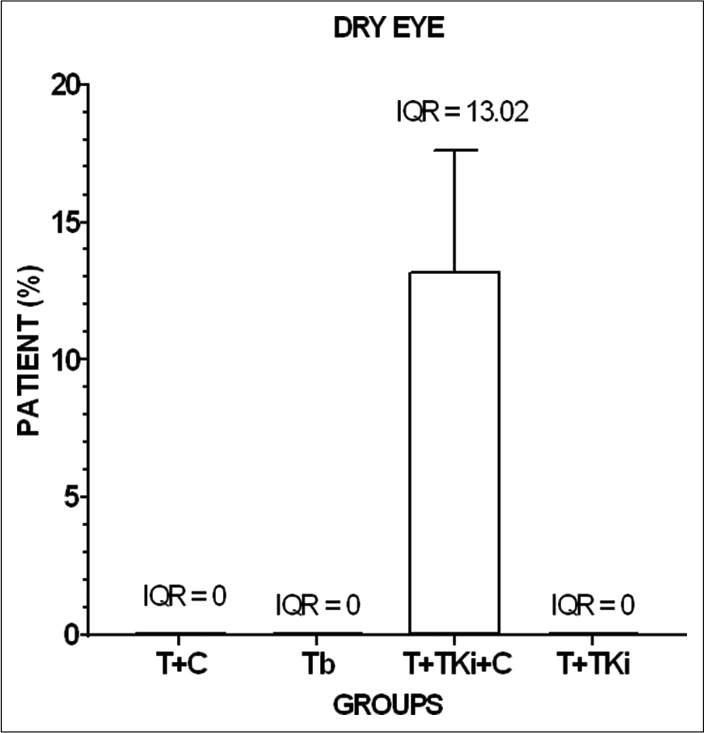
- Box and whisker representation of the range of patients in different groups showing dry eye.
Psychiatric disorders
Depression and insomnia anxiety were the most common psychiatric disorders. The mean percentage of patients that reported psychiatric disorders are mentioned [Table 2]. The IQR is shown [Figure 11].
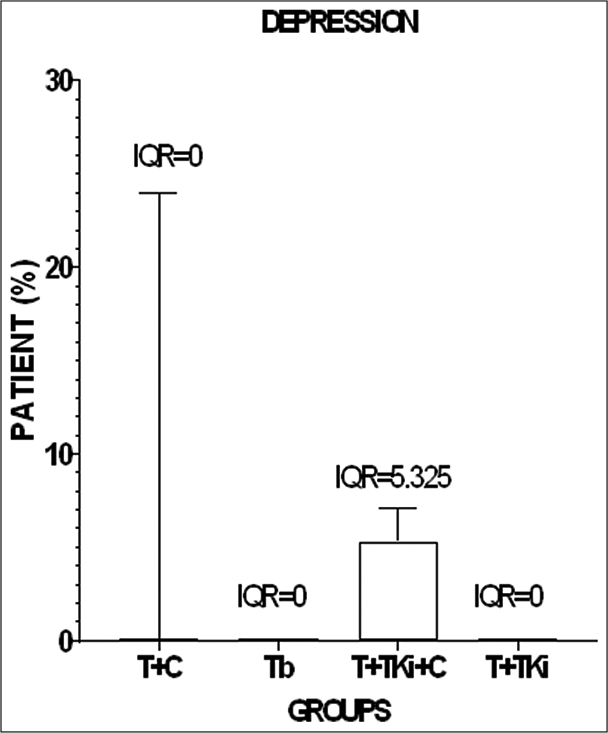
- Box and whisker representation of the range of patients in different groups showing depression.
Blood and lymphatic system disorders
Anaemia, leucopenia, neutropenia, and thrombocytopaenia were the most common blood and lymphatic system disorders.
The mean percentage of patients that reported blood and lymphatic system disorders are mentioned [Table 2]. The IQR is shown [Figures 12a-d].
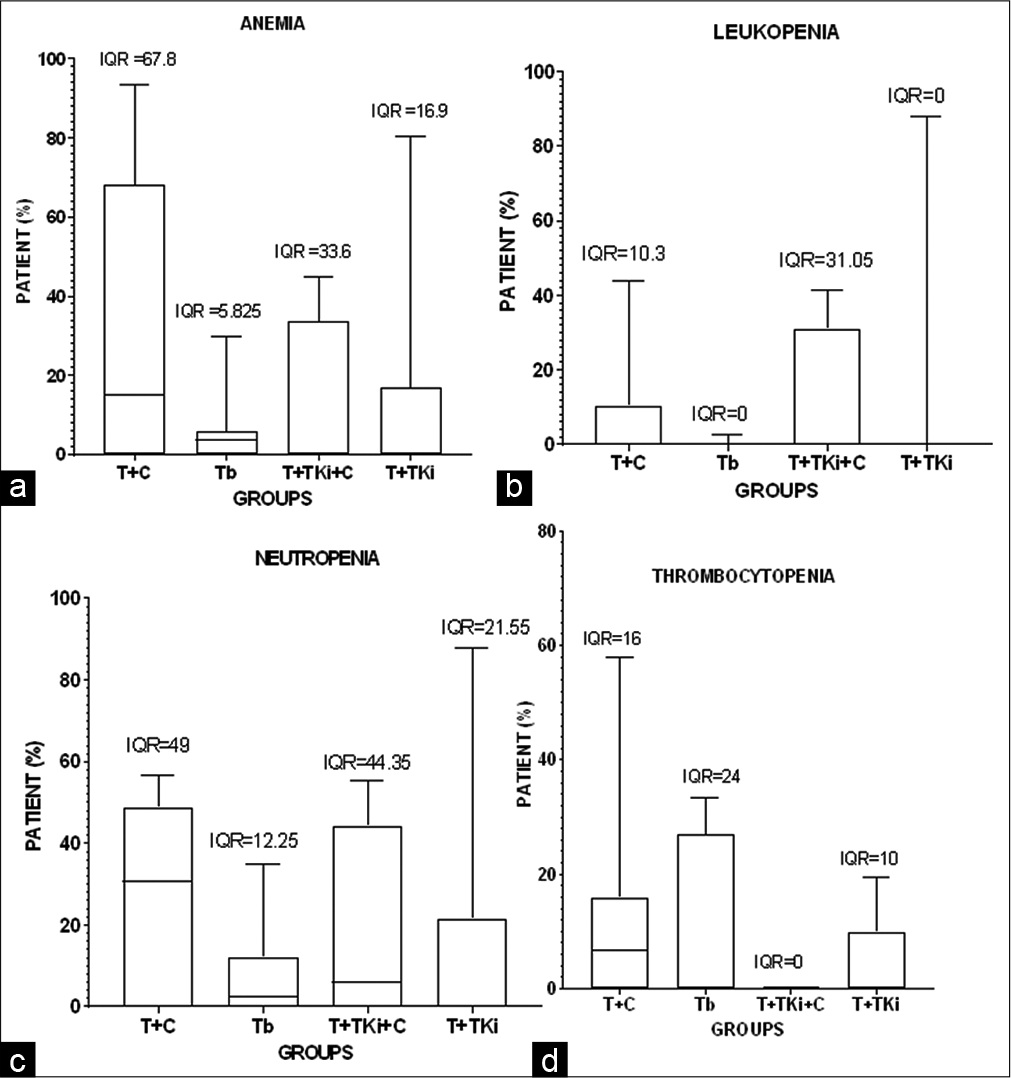
- Box and whisker representation of the range of patients in different groups showing (a) anaemia, (b) leucopenia, (c) neutropenia and (d) thrombocytopenia.
Investigational disorders
Raised AST, ALT, increase WBC, and decreased platelet count were the most common investigational disorders.
The mean percentage of patients that reported investigational disorders are mentioned [Table 2]. The IQR is shown [Figures 13a-c].
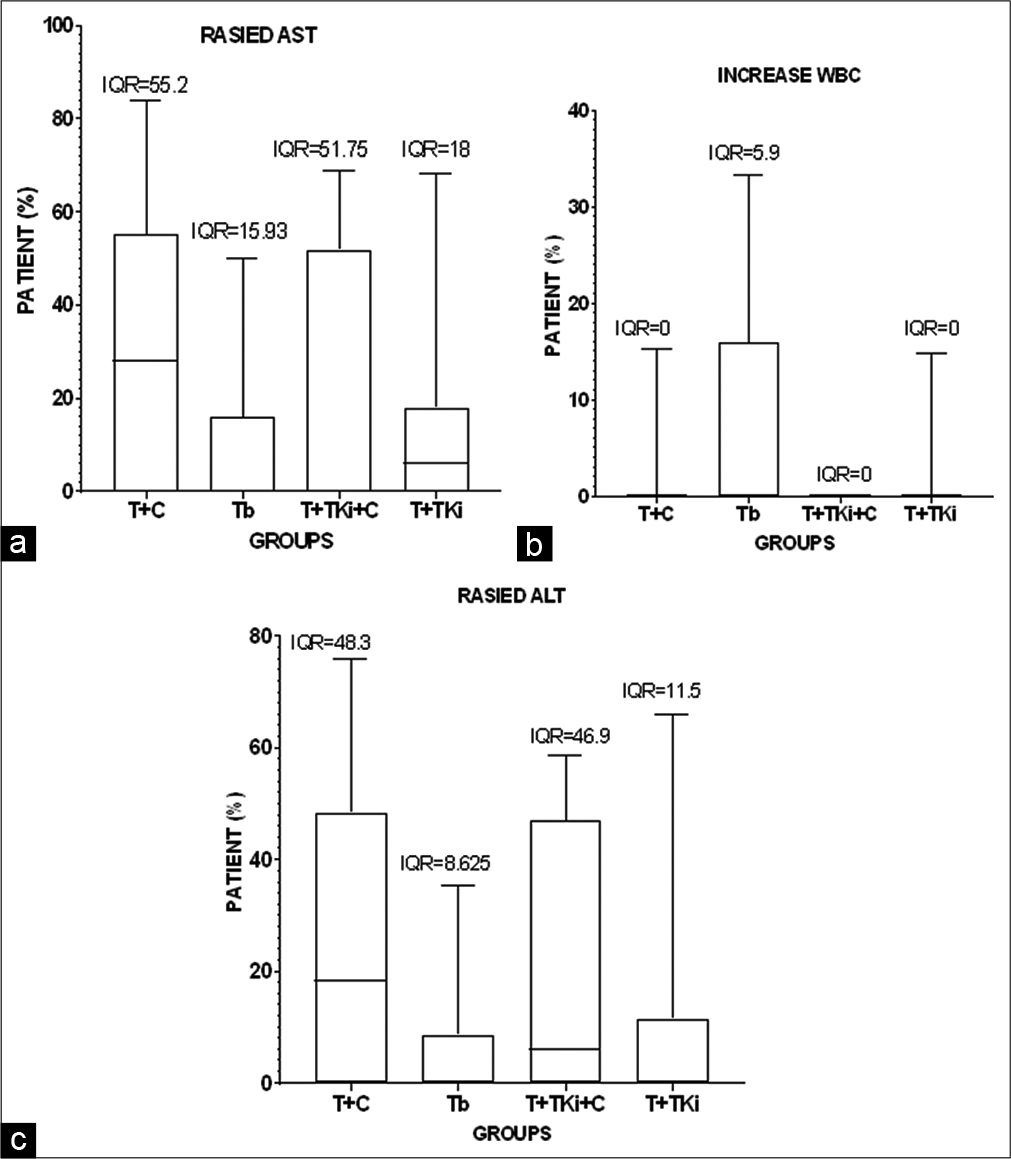
- Box and whisker representation of the range of patients in different groups showing (a) increase AST, (b) increase WBC and (c) increase ALT.
Cardiovascular disorders
The mean percentage of patients that reported cardiac disorder, ejection fraction decrease, and palpitation left ventricular dysfunction were the most common cardiovascular disorders. No vascular disorder was reported in T+TKi+C and T+TKi.
The mean percentage of patients that reported investigational disorders are mentioned [Table 2]. The IQR is shown [Figures 14a and b].
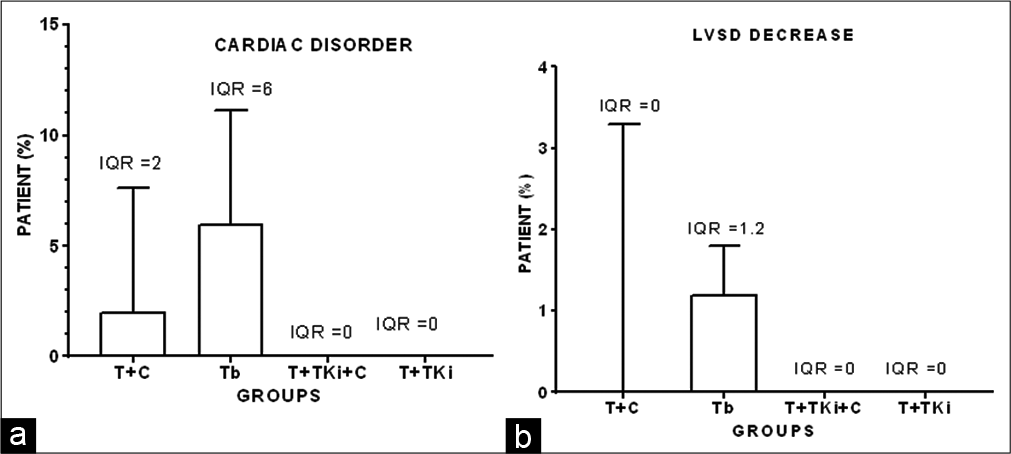
- Box and whisker representation of the range of patients in different groups showing (a) cardiac disorder and (b) LSVD decrease.
Mortality
In most of the studies, no deaths were reported due to monoclonal antibody-associated AEs. The reasons behind these deaths include congestive heart failure, left ventricular systolic dysfunction, BC, or any other reasons which were not specified.
DISCUSSION
The term BC refers to a malignant tumour that has developed from cells in the breast. Usually, BC either begins in the cells of the lobules, which are the milk-producing glands, or the ducts, the passages that drain milk from the lobules to the nipple. The treatment plans for BC are usually classified according to the type of disease, its stage, and any special circumstances. Some treatments are local, which means that they only impact the tumour and not the rest of the body. Most of the women with BC will undergo surgery to remove the tumour. The first-line treatment option for HER-2-positive BC is a combination of pertuzumab, trastuzumab, and a single chemotherapeutic drug.[44] In the second-line treatment, monotherapy of trastuzumab emtansine (T-DM1) is used which is an antibody-drug conjugate that incorporates the HER2-targeted anti-tumour properties of trastuzumab with the cytotoxic activity of the microtubule inhibitory agent (a derivative of maytansine [DM1]) and allows intracellular drug delivery specifically to HER2-overexpressing cells.[45]
Beyond trastuzumab, pertuzumab, and T-DM1, a new class of therapy that is, tyrosine kinase inhibitors (neratinib and tucatinib), were approved for the treatment of HER-2-positive BC that had progressed despite routine treatment after trastuzumab. Bottom of FormOther emerging therapies and novel combinations Top of Form Bottom of Formsuch as the immune checkpoint inhibitors (Keytruda), CDK4/6 inhibitors, and alpha-specific PI3K inhibitors (alpelisib) were also approved.[46]
Trastuzumab therapy prolongs the survival of patients with HER-2 BC when combined with chemotherapy or with tyrosine kinase inhibitors and has been demonstrated to lead a dramatic improvements in disease-free survival.Trastuzumab is a specially made antibody that targets HER-2-positive cancer cells. Trastuzumab attaches to the HER-2 protein on the surface of HER-2-positive cancer cells. Data suggested that both dual HER-2 blockades and mono HER-2 blockade increase AEs risk and huge differences were found among the treatment strategy subgroups.[47]
In the absence of head-to-head to trial, we have conducted a meta-analysis of various study (original research) articles published during the year from 2016 to 2020. The research was done on 27 January 2021. We found 275 articles on PubMed out of which 111 were screening for analyses. Out of 111, we included 35 articles for our study. Out of 32 studies, maximum studies were of Phases II and III CT, conducted in 2017–2019 on age group 71–80 and mainly conducted in the USA. Our main concern or main objective is to study adverse events.
The reported AEs from each of the groups were categorised according to the SOC. The maximum number of AEs reported are related to digestive after that blood-related disorder. The five most prevalent general disorders were noted, with fatigue and asthenia being the most common. The T+C regimen and T+TKi+C regimen had the largest percentage of subjects reporting overall disorder, while the Tb had the lowest rate. Moreover, percentages, respectively, indicating that overall disorder was prevalent in the T+C and T+TKi+C groups. The four most prevalent skin disorders were identified, with baldness and rash being the most common. The T+C regimen had the largest percentage of subjects reporting skin disorder and the T+TKi+C regimen had the lowest percentage. The 13 most frequent digestive system disorders were reported, including diarrhoea, nausea, vomiting, constipation, stomatitis, anorexia, and stomach pain. The T+TKi+C regimen had the largest percentage of subjects reporting digestive disorders. The five most prevalent nerve system disorders were documented, with headaches and neuropathy being the most common. T+C regimens had the largest percentage of subjects reporting neurological disorders followed by T+TKi+C regimens. In the musculoskeletal system, disorder arthralgia, pain in extremity, and back pain in the most common were reported.
The highest percentage in subject reported musculoskeletal system disorder were of T+TKi+C and T+C regimen. In respiratory system, disorder cough and epistaxis were most commonly reported. The highest percentage of subject reported respiratory system disorder was of T+C and T+TKi regimen. In T+TKi+C, infection and infestation were found at a high rate. Few patients in all treatment regimens experienced a decrease in appetite, which was particularly common in the T+TKi regimen. Anaemia, leucopenia, neutropenia, and thrombocytopenia were found in all groups. T+TKi+C regimens had the highest percentage of subjects reporting blood associated disorders followed by Tb. Out of 32 studies, death is reported with biosimilar and T+C.
Repeated electronic searches did not reveal any previous single meta-analysis that assesses and compares the safety of trastuzumab with the various combination used for the treatment of BC. The previous meta-analysis by Dahabreh et al. found that the use of trastuzumab benefits in disease control and survival came at the cost of serious cardiovascular AEs, particularly heart failure accompanied by LVEF decline.[48] Furthermore, Abraham J states that the combination of trastuzumab and lapatinib (seems to be a safe treatment option in terms of cardiotoxicity but the lapatinib was associated with two well-documented AEs, diarrhoea and dermatologic toxicity.[40] Similar results are also shown by Xin et al. and Xu et al. that is, the use of lapatinib and trastuzumab in HER2-positive BC cause skin rash, diarrhoea, neutropenia, and hepatic and other AEs.[49,50] Gianni L, Dafni U, et al. found that cardiac toxicity was comparable between anti-HER2 combination therapy and anti-HER2 monotherapy.[51]
As we have seen that the previous studies only reported about cardiovascular AEs related to trastuzumab but our study concluded all the systemic AEs along with cardiovascular, more often cardiotoxicity when TKi is given combined with chemotherapy, other systemic toxicities also occur. Furthermore, when chemotherapy is given in this combination, it causes higher systemic side effects. As a result, this study implies that Tb is preferable to alternative medication combinations but the patients must be monitored for cardiovascular toxicity.
Limitations of our study
There are certain limitations to our meta-analysis that should be acknowledged. First limitation is that the number of studies and patients included in some of the outcomes is minimal, reducing the meta-analysis ability to reveal statistically significant results. Our study’s second limitation is that the data were gathered from published research rather than from individual patient data (IPD). When compared to IPD studies, meta-analyses based on published data tend to exaggerate treatment effects. However, if all authors do not agree to disclose their whole databases to the analysing group, analyses employing IPD may include fewer research. In general, an IPD-based meta-analysis will provide a more reliable estimate of the correlation.
CONCLUSION
This study concluded that biosimilar of trastuzumab (SB-3 and CT-6P) is safest for the treatment of HER-2-positive BC. Cardiovascular disorder is often reported with biosimilar group, but this group has less AEs reported as compared with chemotherapy, tyrosine kinase inhibitors groups related to other systems such as digestive, nervous, and respiratory.
The choice of combination is depending on the type of BC and the condition of patients. The patients must monitor for cardiotoxicity when the biosimilar of trastuzumab is used.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Three-dimensional in vitro hydro-and cryogen-based cell-culture models for the study of breast-cancer metastasis to bone. Cancers. 2018;10:292.
- [CrossRef] [PubMed] [Google Scholar]
- News I. Cancer Cases in India Estimated to be 13.9 Lakh in 2020 m. Cancer Cases in India Estimated to be 13.9 lakh in 2020 May Rise to 15.7 Lakh by 2025: Report India News Times of India. 2021. The Times of India. Available from: https://timesofindia.indiatimes.com/india/cancer-cases-in-india-estimated-to-be-13-9lakh-in-2020-may-rise-to-15-7-lakhby-2025report/articleshow/77628680.cms. [Last accessed on 2021 Oct 25]
- [Google Scholar]
- Available from: https://www.nationalbreastcncer.org/wpcontent/uploads/2020-breast-cancer-stats.pdf. [Last accessed on 2021 Oct 25]
- The distinctive nature of HER2-positive breast cancers. N Engl J Med. 2005;353:1652-4.
- [CrossRef] [PubMed] [Google Scholar]
- Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science. 1989;244:707-12.
- [CrossRef] [PubMed] [Google Scholar]
- Epidermal growth factor receptor (HER1) tyrosine kinase inhibitor ZD1839 (Iressa) inhibits HER2/neu (erbB2)-overexpressing breast cancer cells in vitro and in vivo. Cancer Res. 2001;61:8887-95.
- [Google Scholar]
- Spotlight on Trastuzumab in the management of HER2-positive metastatic and early-stage breast cancer. BioDrugs. 2006;20:259-62.
- [CrossRef] [PubMed] [Google Scholar]
- Primary breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26(Suppl 5):v8-30.
- [CrossRef] [PubMed] [Google Scholar]
- Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005;353:1673-84.
- [CrossRef] [PubMed] [Google Scholar]
- Neoadjuvant chemotherapy with trastuzumab, docetaxel, and carboplatin administered every 3 weeks for Japanese women with HER2-positive primary breast cancer: Efficacy and safety. Int J Clin Oncol. 2017;22:880-6.
- [CrossRef] [PubMed] [Google Scholar]
- Neoadjuvant buparlisib plus trastuzumab and paclitaxel for women with HER2+ primary breast cancer: A randomised, double-blind, placebo-controlled phase II trial (NeoPHOEBE) Eur J Cancer. 2017;85:133-45.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of everolimus in combination with trastuzumab and paclitaxel in Asian patients with HER2+ advanced breast cancer in BOLERO-1. Breast Cancer Res. 2017;19:47.
- [CrossRef] [PubMed] [Google Scholar]
- Phase II study of buparlisib (BKM120) and trastuzumab in patients with HER2+ locally advanced or metastatic breast cancer resistant to trastuzumab-based therapy. Breast Cancer Res Treat. 2018;168:357-64.
- [CrossRef] [PubMed] [Google Scholar]
- A phase I trial of ganetespib in combination with paclitaxel and trastuzumab in patients with human epidermal growth factor receptor-2 (HER2)-positive metastatic breast cancer. Breast Cancer Res. 2017;19:89.
- [CrossRef] [PubMed] [Google Scholar]
- Oral vinorelbine in combination with trastuzumab as a first-line therapy of metastatic or locally advanced HER2-positive breast cancer. Cancer Chemother Pharmacol. 2016;77:1069-77.
- [CrossRef] [PubMed] [Google Scholar]
- Trastuzumab, non-pegylated liposomal-encapsulated doxorubicin and paclitaxel in the neoadjuvant setting of HER-2 positive breast cancer. Int J Clin Pharm. 2016;38:446-53.
- [CrossRef] [PubMed] [Google Scholar]
- Trastuzumab in combination with weekly paclitaxel and carboplatin as neoadjuvant treatment for HER2-positive breast cancer: The TRAIN-study. Eur J Cancer. 2017;74:47-54.
- [CrossRef] [PubMed] [Google Scholar]
- 9 weeks vs 1 year adjuvant trastuzumab in combination with chemotherapy: Results of the phase III multicentric Italian study Short-HER. J Clin Oncol. 2017;35(Suppl 15):501.
- [CrossRef] [Google Scholar]
- Effect of adjuvant trastuzumab for a duration of 9 weeks vs 1 year with concomitant chemotherapy for early human epidermal growth factor receptor 2-positive breast cancer: The sold randomized clinical trial. JAMA oncol. 2018;4:1199-206.
- [CrossRef] [PubMed] [Google Scholar]
- Neoadjuvant chemotherapy with nabpaclitaxel plus trastuzumab followed by 5-fluorouracil/ epirubicin/cyclophosphamide for her2-positive operable breast cancer: A multicenter phase II trial. Anticancer Res. 2019;39:2053-9.
- [CrossRef] [PubMed] [Google Scholar]
- Trastuzumab emtansine (T-DM1) plus S-1 in patients with trastuzumab-pretreated HER2-positive advanced or metastatic breast cancer: A phase Ib study. Oncology. 2019;96:309-17.
- [CrossRef] [PubMed] [Google Scholar]
- A multicenter Phase II study evaluating the efficacy, safety and pharmacokinetics of trastuzumab emtansine in Japanese patients with heavily pretreated HER2-positive locally recurrent or metastatic breast cancer. Jpn J Clin Oncol. 2016;46:407-14.
- [CrossRef] [PubMed] [Google Scholar]
- CT-P6 compared with reference trastuzumab for HER2-positive breast cancer: A randomised, double-blind, active-controlled, phase 3 equivalence trial. Lancet Oncol. 2017;18:917-28.
- [CrossRef] [Google Scholar]
- A phase III study comparing SB3 (a proposed trastuzumab biosimilar) and trastuzumab reference product in HER2-positive early breast cancer treated with neoadjuvantadjuvant treatment: Final safety, immunogenicity and survival results. Eur J Cancer. 2018;93:19-27.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Safety of the trastuzumab biosimilar ABP 980 in women with HER2-positive early breast cancer in the randomized, double-blind, active-controlled LILAC study. Drug Saf. 2020;43:233-42.
- [CrossRef] [PubMed] [Google Scholar]
- Three-year follow-up from a phase 3 study of SB3 (a trastuzumab biosimilar) versus reference trastuzumab in the neoadjuvant setting for human epidermal growth factor receptor 2-positive breast cancer. Eur J Cancer. 2019;120:1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N Engl J Med. 2020;382:610-21.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of CT-P6 versus reference trastuzumab in HER2-positive early breast cancer: Updated results of a randomised phase 3 trial. Cancer Chemother Pharmacol. 2019;84:839-47.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of dasatinib with trastuzumab and paclitaxel in first line HER2-positive metastatic breast cancer: Results from the phase II GEICAM/2010-04 study. Breast Cancer Res Treat. 2019;174:693-701.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized, controlled phase II trial of neoadjuvant ado-trastuzumab emtansine, lapatinib, and nabpaclitaxel versus trastuzumab, pertuzumab, and paclitaxel in HER2-positive breast cancer (TEAL study) Breast Cancer Res. 2019;21:100.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of trastuzumab, lapatinib, and paclitaxel neoadjuvant treatment with or without prolonged exposure to anti-HER2 therapy, and with or without hormone therapy for HER2-positive primary breast cancer: A randomised, five-arm, multicentre, open-label phase II trial. Breast Cancer. 2018;25:407-15.
- [CrossRef] [PubMed] [Google Scholar]
- A phase I/II study of epertinib plus trastuzumab with or without chemotherapy in patients with HER2-positive metastatic breast cancer. Breast Cancer Res. 2019;22:1.
- [CrossRef] [PubMed] [Google Scholar]
- Neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET): A multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2016;17:367-77.
- [CrossRef] [Google Scholar]
- Trastuzumab emtansine versus capecitabine plus lapatinib in patients with previously treated HER2-positive advanced breast cancer (EMILIA): A descriptive analysis of final overall survival results from a randomised, open-label, phase 3 trial. Lancet Oncol. 2017;18:732-42.
- [CrossRef] [Google Scholar]
- Phase III, randomized study of dual human epidermal growth factor receptor 2 (HER2) blockade with lapatinib plus trastuzumab in combination with an aromatase inhibitor in postmenopausal women with HER2-positive, hormone receptor-positive metastatic breast cancer: ALTERNATIVE. J Clin Oncol. 2018;36:741-8.
- [CrossRef] [PubMed] [Google Scholar]
- Phase I dose-escalation trial of tucatinib in combination with trastuzumab in patients with HER2-positive breast cancer brain metastases. Ann Oncol. 2020;31:1231-9.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective, multicenter study of the efficacy of lapatinib plus trastuzumab in HER2-positive metastatic breast cancer patients previously treated with trastuzumab, lapatinib, or both: The Trastyvere study. Clin Transl Oncol. 2020;22:420-8.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and efficacy of T-DM1 Plus neratinib in patients with metastatic HER2-positive breast cancer: NSABP foundation Trial FB-10. J Clin Oncol. 2019;37:2601-9.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized phase II study to determine the efficacy and tolerability of two doses of eribulin plus lapatinib in trastuzumab-pretreated patients with HER-2-positive metastatic breast cancer (E-VITA) Anticancer Drugs. 2019;30:394-401.
- [CrossRef] [PubMed] [Google Scholar]
- Phase II clinical trial of first-line eribulin plus trastuzumab for advanced or recurrent HER2-positive breast cancer. Anticancer Res. 2018;38:4073-81.
- [CrossRef] [PubMed] [Google Scholar]
- A phase Ib study of entinostat plus lapatinib with or without trastuzumab in patients with HER2-positive metastatic breast cancer that progressed during trastuzumab treatment. Br J Cancer. 2019;120:1105-12.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of subcutaneous trastuzumab and intravenous trastuzumab as part of adjuvant therapy for HER2-positive early breast cancer: Final analysis of the randomised, two-cohort PrefHer study. Eur J Cancer. 2017;86:82-90.
- [CrossRef] [PubMed] [Google Scholar]
- Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367:1783-91.
- [CrossRef] [PubMed] [Google Scholar]
- Combination therapies for the treatment of HER2-positive breast cancer: Current and future prospects. Expert Rev Anticancer Ther. 2018;18:629-49.
- [CrossRef] [PubMed] [Google Scholar]
- Lapatinib, trastuzumab or the combination added to preoperative chemotherapy for breast cancer: A meta-analysis of randomized evidence. Breast Cancer Res Treat. 2012;135:655-62.
- [CrossRef] [PubMed] [Google Scholar]
- Trastuzumab in the adjuvant treatment of early-stage breast cancer: A systematic review and meta-analysis of randomized controlled trials. Oncologist. 2008;13:620-30.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of lapatinib or trastuzumab, alone and in combination, in human epidermal growth factor receptor 2-positive breast cancer: A meta-analysis of randomized controlled trials. Cancer Med. 2016;5:3454-63.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of lapatinib and trastuzumab for HER2-positive breast cancer: A systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2017;7:e013053.
- [CrossRef] [PubMed] [Google Scholar]
- Herceptin adjuvant (HERA) trial study team treatment with trastuzumab for 1 year after adjuvant chemotherapy in patients with HER2-positive early breast cancer: A 4-year follow-up of a randomised controlled trial. Lancet Oncol. 2011;12:236-44.
- [CrossRef] [Google Scholar]







