Translate this page into:
Effect of chlorhexidine gluconate as hemostatic agent in healing and repair after mineral trioxide aggregate vital pulp therapy in young permanent teeth – A clinical study
*Corresponding author: Dr. Shalini Garg, Professor, Department of Pediatric and Preventive Dentistry, SGT University, Gurugram, India. shaloosandeep@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma P, Garg S, Dhindsa A, Jain N, Joshi S, Gupta A. Effect of chlorhexidine gluconate as hemostatic agent in healing and repair after mineral trioxide aggregate vital pulp therapy in young permanent teeth – A clinical study. Indian J Physiol Pharmacol 2021;65:222-8.
Abstract
Objectives:
The aim of the study was to evaluate the clinical success of mineral trioxide aggregate (MTA) partial pulpotomy as a definitive procedure in deeply carious permanent posterior teeth using 0.12% chlorhexidine (CHX) gluconate or normal saline as hemostatic agents.
Materials and Methods:
A pilot randomized control clinical trial was conducted on subjects with a deep carious lesion on 20 immature posterior teeth of subjects (10.8 ± 2.62 years). Caries and the superficial layer of exposed pulp were removed and then flushed with 0.12% CHX or saline solution. Gray MTA was placed, followed by resin-modified glass ionomer and composite.
Results:
12 months follow-up showed 100% clinical and 90% radiographical success in both groups. Dentine Bridge was formed 90% in both the study and control group, which showed MTA partial pulpotomy is an effective procedure (P = 0.000).
Conclusion:
MTA partial pulpotomy using 0.12% CHX gluconate as a hemostatic agent for the treatment of deeply carious immature permanent posterior teeth appears to increase the radiographic rate of formation of dentin bridge as compared to the normal saline.
Keywords
Vital
Immature
Posterior
Carious pulpally exposed
INTRODUCTION
Deep pit and fissure caries in newly erupted permanent posterior teeth are a potential threat to pulp vitality. A vital pulp is required to complete root formation and provides the immune protective mechanism for an immature permanent tooth. An antimicrobial interventional procedure checks the progress of tooth decay by interfering with the metabolic activity of microorganisms.[1,2] Vital pulp therapy for carious exposed immature permanent posterior teeth is used to promote root completion.[3] The vital pulp can initiate several protective mechanisms to defend the body from bacterial invasion.[3,4] Partial pulpotomy (Massler in 1972)[5] is a form of vital pulp therapy; the most superficial pulp layer and 1–2 mm dentin are removed to check bacteria/toxins affected tissue. It preserves cell-rich layer to a great extent, thus enhancing healing along with physiologic dentine deposition at the junction of pulpotomy material and pulp. The partial pulpotomy procedure has been carried out in immature permanent teeth as this has the extra advantage of allowing maturogenesis in the case of immature teeth.[6-10] Root completion in immature teeth treated with partial pulpotomy shows the procedure’s success. Biocompatible materials have immense potential for healing by repair and regeneration.[11-13] Gray mineral trioxide aggregate (MTA) provides an excellent coronal seal and a suitable environment for required healing. Gray MTA demonstrated significantly less leakage than white MTA.[14,15] It prevents further ingress of bacterial and toxins and promotes the formation of Dentin Bridge.[14-16] Chlorhexidine (CHX) may be used as a solution to be mixed with MTA. It is known to enhance MTA’s antimicrobial properties and has a significant role in pulp hemostasis and high substantiveness.[17]
Thus, the present study was planned to assess the success of MTA partial pulpotomy and is the definitive procedure for treating deeply carious immature permanent teeth using 0.12% CHX gluconate versus normal saline antiseptic, hemostatic agents.
MATERIALS AND METHODS
The present pilot study with balanced randomization was conducted. Clinicians obtained ethical clearance from the Institutional Ethical Committee review board (project no. 420) after explaining the purpose and procedure of the trial. The subjects, data analysts were kept blinded to an allocation by the chit method. It was a double-blind study: Patients and evaluators did not know about group allocation.
Subjects
The study was carried out among 15 children aged between 7 and 16 years (20 vital posterior teeth) with a deep carious lesion almost approaching the pulp. Examiners selected permanent immature posterior teeth with no signs and symptoms of irreversible pulpitis or evidence of root resorption/pathologic changes in tooth-supporting structures. Written consent forms were obtained from the patients before inclusion in the study. The exclusion criteria were patients with any systemic disease and patients with clinical and radiographic symptoms of irreversible pulpitis [Figure 1]. Teeth with a history of spontaneous pain and radiographic evidence of pathologic periapical changes were considered cases of irreversible pulpitis.
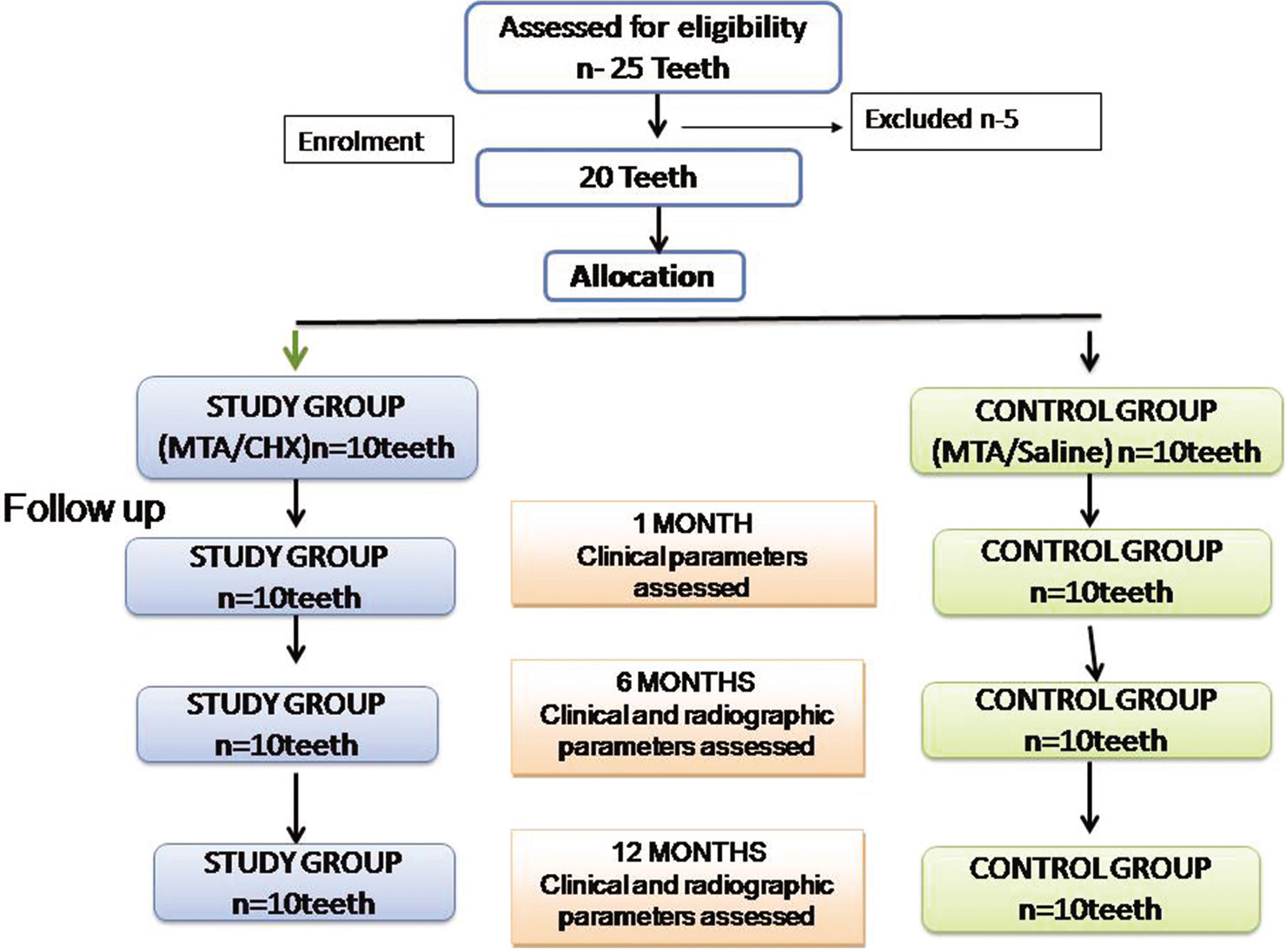
- Consort flow chart of the randomized control clinical trial.
Intervention
The subjects were assigned randomly through chit method to one of the two parallel groups in a 1:1 ratio and were treated with partial pulpotomy and hemostasis with 0.12% CHX gluconate (Loba Chemie Pvt. Ltd., Mumbai) in the study group, and normal saline in the control group then capped with MTA (Angelus) mixed with 0.12% CHX in the study group and with distilled water in the control group followed by permanent coronal composite restoration.
Procedure
All affected and infected carious dentin was removed with a hand piece using large round diamond (BR-31, Mani) bur. A continuous water spray and copious irrigation with a hemostatic agent were used to prevent any injury due to heat to the pulp. The pulpal roof was removed carefully with the help of a spoon excavator along with up to 2–4 mm of pulp tissue (based on fresh bleeding achieved). The pulp wound was gently flushed with a 2 ml solution of 0.12% CHX in the study group and with normal saline in the control group to control the bleeding (2 ml solution once) gently. After that, Gray MTA was mixed according to the manufacturer’s instructions on a glass slab with 0.12% CHX in the study group and with distilled water in the control group. Using MTA carrier, a thickness of 2–4 mm of the MTA was placed against on pulpal tissue. The material was adapted to the amputation site with the help of a wet applicator tip (as hydrophilic particles in MTA hardens in the presence of moisture) and a cotton pellet. The cavity floor was covered with Vitrabond as a base (light-cured resin-modified glass ionomer). The tooth was restored with a permanent coronal composite restoration. Clinical follow-up was done monthly for 3 months and then every 3 months for 12 months. Radiographic evaluation was done after every 6 months for 12 months to assess healing and dentin bridge formation. Two examiners, who were blinded to treatment type, evaluated the teeth clinically and radiographically.
Appraisal of dentine bridge formation in pulp chamber
Both immediate post-operative and after 12 months post-operative intraoral periapical (IOPA) radiographs of each site were taken using XCP extension cone paralleling technique and digitized using a digital camera (canon power shot IXUS 155,10×. IS). The digitized images were stored in JPEG format and were transferred to Adobe Photoshop (CS3 extended version). Grid was placed on the digitized IOPA radiograph. Dentine bridge formation included apprising the root lengthening, root canal thickening, and percentage increase in radio-opacity area as reported in the literature.[12-15] Square grid lines of 0.3 mm were superimposed on radiographic images. The distance between the two points of each line was measured by using superimposed square grid lines. The percentage increase was calculated by subtracting the two measurements; using the above method of immediate post-operative and after 12 months post-operative radiographs. Weighing the risk/benefit ratio cone-beam computed tomography (CBCT) should be avoided in children if assessment and follow-up can be done by digital 2D radiography as we did in the present study. CBCT examination was not done to avoid high radiation exposure [Figure 2].
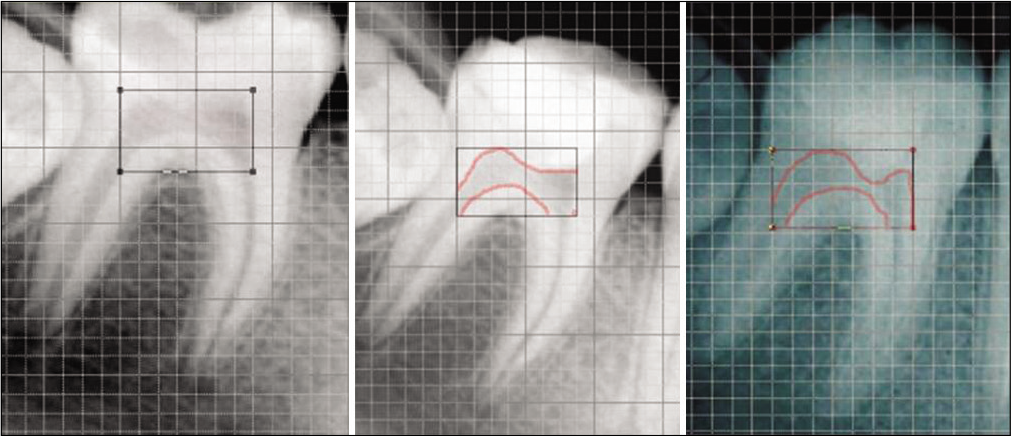
- Digital quantitative analysis between immediate post-operative and after 12 month follow-up partially pulpotomized tooth.
Statistical analysis
SPSS software (version 23.0; SPSS Inc., Chicago, IL, USA) was used for statistical analysis. One-way ANOVA and t-test were applied for comparison between study and control groups. The Pearson Chi-square test made data comparisons, and time-related variables paired t-test was used. All statistical tests were performed at the significance level of P = 0.05.
RESULTS
Twenty teeth were randomly distributed into two groups, and all the patients completed the 12 monthly follow-ups. The mean age of patients was 10.8 ± 2.62 years with 10.7 ± 2.6, 10.9 ± 2.72 years for Group I and Group II, respectively. None of the patients experienced Pain, Tender on percussion, Swelling, Mobility, dislodged restoration at any clinical follow-up to 12 months showing 100% clinical success.
MTA partial pulpotomy was a radiographically highly statistically significant effective procedure by 90% success (P = 0.00**) about all radiographic parameters, that is, absence of calcification, periapical radiolucency, and periodontal ligament changes [Figure 3]. However, one molar in the study group had periapical radiolucency, and one molar in the control group had condensing osteitis and calcification in pulp space after 6 months of follow-up. Both molars were excluded from the study, and required endodontic treatment was done. Examiners found no significant difference in radiographic success between groups.
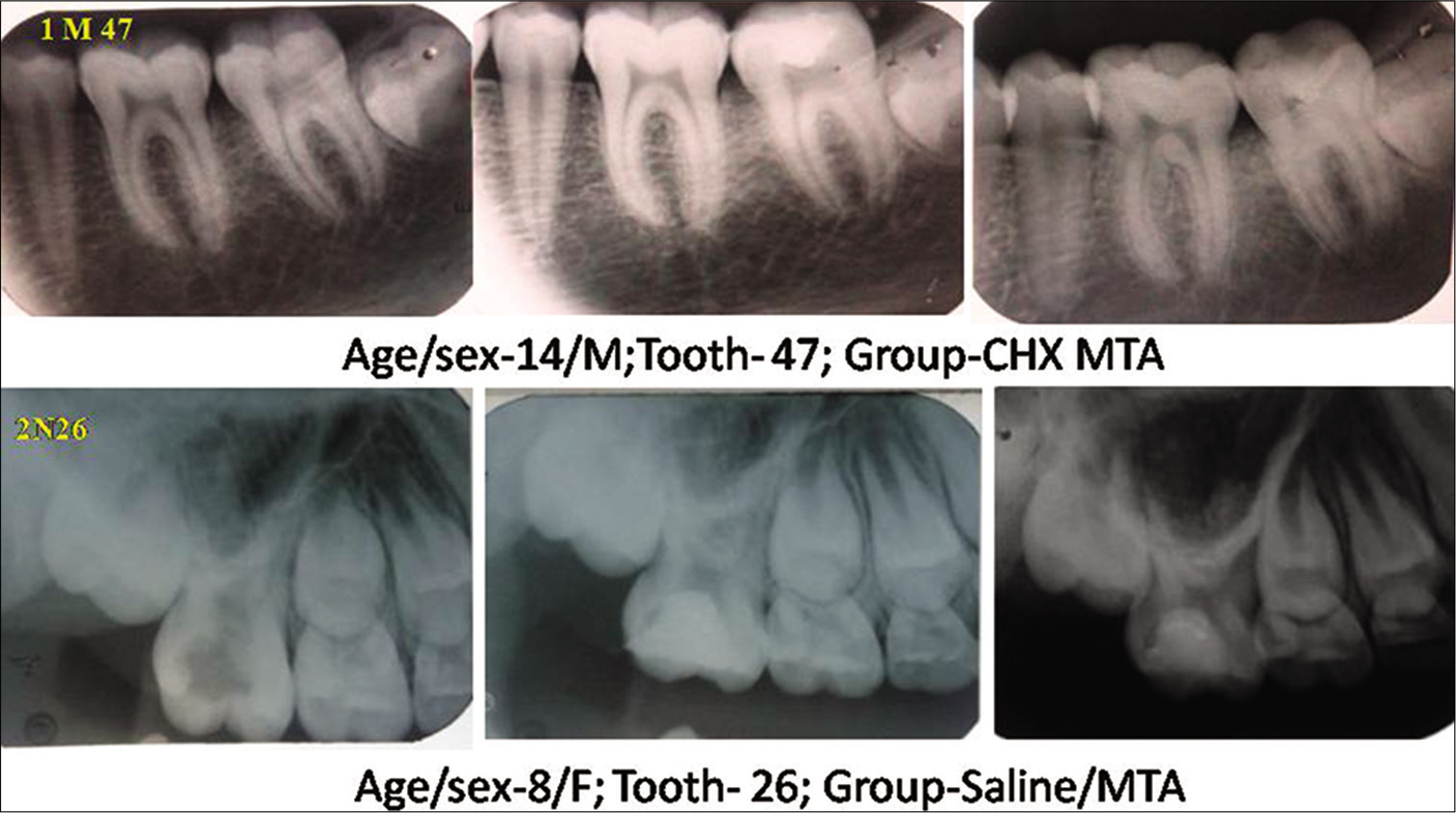
- Representative radiographs of 12 months follow up after mineral trioxide aggregate partial pulpotomy with (Group 1) or without (Group 2) using 0.12% chlorhexidine gluconate.
Quantitative percentage increase in protective radio-opacity (calcific bridge below MTA) in radiographic pulp chamber space is 13.177 irrespective of groups; while individually it was 10.555 ± 4.824 in the control group and 15.800 ± 5.9380 in the study group (P = 0.05), which showed study group performed better with 1.5 folds more competent than the control group [Table 1]. Dentine bridge formation was observed radiographically in pulp chamber below the MTA at 6 months in 80% molars of the study group, and 50% molars of the control group (P = 0.042) at 6 months and showed it was highly significantly effective in rapid formation of dentine bridge (P = 0.035). However, at 12 months, dentine bridge was formed in 90% of teeth in both the groups, which showed MTA partial pulpotomy is an effective procedure in the formation of dentine bridge (P = 0.00) [Table 2].
| Group | n | Mean | Std. deviation | Std. error mean | t-test for Equality of Means | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| t | df | Sig. (2-tailed) | Mean difference | Std. error difference | 95% confidence Interval of the difference | ||||||
| Lower | Upper | ||||||||||
| % Increase | |||||||||||
| Saline/MTA (Control ) | 9 | 10.555 | 4.82470 | 1.6082 | –2.05 | 16 | 0.056 | –5.24444 | 2.55033 | –10.65091 | 0.16202 |
| CHX/MTA (study) | 9 | 15.800 | 5.93801 | 1.9793 | |||||||
MTA: Mineral trioxide aggregate, CHX: Chlorhexidine
| Radiographic Parameters | Group | 6 months | 12 months | P-value separately within groups | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| 6 months | 12 months | |||||||
| Dentine bridge formation | Study (Chlorhexidine 0.12%/MTA) | Present | 8 | 80 | 9 | 90 | 0.035** | 0.000** |
| 40 | 45 | |||||||
| Absent | 2 | 20 | 1 | 10 | ||||
| 10 | 5 | |||||||
| Total | 10 | 100 | 10 | 100 | ||||
| Control (Normal Saline/MTA) | Present | 5 | 50 | 9 | 90 | 0.292 | 0.000** | |
| 25 | 5 | |||||||
| Absent | 5 | 50 | 1 | 10 | ||||
| 25 | 5 | |||||||
| Total | 10 | 100 | 10 | 100 | ||||
| Total | 20 | 20 | ||||||
| P-value combine that is total intergroup | 0.042 | |||||||
MTA: Mineral trioxide aggregate, CHX: Chlorhexidine. **Significance level of P=0.05
Root formation after 6 months of partial pulpotomy had attained one stage increase (Demirjian’s stage of root development) by 50% in the study group and 20% in the control group at 12 months with complete closure of root (100%) in both groups at 12 months (P = 0.000). Moreover, examiners found 30% rapid attainment of root development in the CHX group than saline group [Table 3] and [Figure 4].
| Tooth Id No. | Group | Age | Sex | Dentine bridge formation | Demirjian’s stage of root formation | Protective dentine formation (in %) | ||
|---|---|---|---|---|---|---|---|---|
| 6 months | 12 months | 6 months | 12 months | |||||
| 2Bi | Saline/MTA | 14 | M | No | Yes | One stage increase | Two stage increase | 7 |
| 2Fj | 13 | M | No | Yes | Healing | One stage increase | 8 | |
| 2Fe | 13 | M | Yes | Yes | Healing | One stage increase | 17 | |
| 2Ff | 13 | M | Yes | Yes | Healing | One stage increase | 17 | |
| 2Gi | 14 | M | Yes | Yes | Healing | One stage increase | 9 | |
| 2Lb | 9 | F | No | Yes | Healing | Healing | 8 | |
| 2Nb | 8 | F | Yes | Yes | Healing | One stage increase | 9 | |
| 2Pb | 7 | M | Yes | Yes | One stage increase | Two stage increase | 16 | |
| 2Qa | 9 | M | No | Yes | Healing | One stage increase | 4 | |
| 2Ed | 9 | M | No | No | Healing | Healing | NA | |
| 1Ag | CHX/MTA | 9 | M | Yes | Yes | Healing | One stage increase | 17 |
| 1Hb | 9 | M | Yes | Yes | One stage increase | Two stage increase | 20 | |
| 1Hc | 9 | M | No | Yes | One stage increase | Two stage increase | 8 | |
| 1Hb | 9 | M | Yes | Yes | One stage increase | Two stage increase | 25 | |
| 1Jh | 14 | M | Yes | Yes | Healing | Healing | 22.2 | |
| 1Kc | 8 | F | Yes | Yes | One stage increase | One stage increase | 17 | |
| 1Kd | 8 | F | Yes | Yes | One stage increase | Two stage increase | 13 | |
| 1Mi | 14 | M | Yes | Yes | Healing | One stage increase | 10 | |
| 1Oi | 14 | F | Yes | Yes | Healing | One stage increase | 10 | |
| 1Dh | 13 | M | No | No | Healing | Healing | NA | |
MTA: Mineral trioxide aggregate, CHX: Chlorhexidine
![Quantitative dentine bridge formed in study group (chlorhexidine/mineral trioxide aggregate [MTA]) and control group (saline/MTA) according to time period.](/content/114/2021/65/4/img/IJPP-65-222-g004.png)
- Quantitative dentine bridge formed in study group (chlorhexidine/mineral trioxide aggregate [MTA]) and control group (saline/MTA) according to time period.
DISCUSSION
Partial pulpotomy by removing the infected pulp (not more than 2–4 mm) is a proven alternative for immature permanent teeth with exposed vital pulps and appears to complete the aims and objectives of any other vital pulp therapy.[1,4] Bio inductive materials like MTA promote healing by providing a suitable environment with a tight coronal seal.[18]
Healing is observed to be different when partial pulpotomy is done in traumatized teeth than in carious teeth. Fewer success chances lie in carious teeth as the presence of bacteria and ingression of bacteria in dentinal tubules may slow down the healing, and hence a deep carious lesion approximating pulp is usually treated by pulpotomy to maintain the forms and functions of pulp. When a tooth is pulpally involved by trauma, there is no associated bacterial infection if checked immediately; the type of bacteria would also be different. Dentinal tubules in a carious tooth are affected as caries lesion progresses over time. Restorative cavity prepared will be almost sterilized and ecologically diverse in the emergency treatment of a partially pulpotomized traumatized immature anterior tooth compared to an immature permanent molar with carious exposure.[16] Similar studies have been reported in the literature by various authors.[8-11]
Antibacterial agents like CHX will work favorably to promote healing and has a key role in cavity disinfection. CHX is effective against Gram-positive, facultative anaerobes, aerobes Actinomyces, Fusobacterium nucleatum, odontolites, Enterococcus faecalis, Escherichia coli, Staphylococcus aureus, and Candida albicans.[19] Antibacterial and antimicrobial effects of CHX mixed with MTA significantly better in vitro.[20] CHX has shown a significant reduction in caries associated with Streptococcus mutans and Lactobacillus growth. It acts by binding to both pulp and hard tissue surfaces. This property helps it in being active for a more extended period, even after its use. Antibacterial action is due to increased cellular membrane permeability followed by coagulation of the cytoplasmic macromolecules.[21]
CHX gel has a great potential to be used as an endodontic auxiliary chemical substance. Ferraz et al. 2007 assessed in vitro the antimicrobial efficacy of CHX gluconate gel as an additional endodontic chemical compared to sodium hypochlorite (NaOCl) and CHX gluconate solution using agar diffusion test against five facultative anaerobic bacteria and four pigmented Gram-negative anaerobes. The larger growth inhibition zones were with 2% CHX gluconate gel, that is, 11.79 mm (P < 0.05) than produced by all NaOCl concentrations, including 5.25% (9.54 mm).[22]
In the present study, the clinical success rate was 100% irrespective of groups, proving partial pulpotomy is highly successful.[8,11] Mejare and Cvek in 1993 and Mass and Zilberman in 1995 reported 93.5% and 91.4% success in carious immature teeth treated with partial pulpotomy for 24–140 months. Intact coronal seal leading to no bacterial recontamination in the present study must have contributed to partial pulpotomy’s high significant clinical success. Massler, in 1972,[23] described the most crucial reason for the failure of vital pulp therapy as bacterial recontamination and suggested that the critical factor in vital pulp therapy is the coronal seal.
Parameter like maturogenesis was assessed by Demirjian’s stages of root formation was unique to this study. At 6 months, 50% of permanent molars showed one stage increase in Demirjian’s root formation stage in the study group compared to 20% in the control group (P = 0.000). At 12 months, complete root closure (100%) in both groups has occurred. Examiners found 30% more rapid root development in the study group than in the control group. Various authors also reported apexogenesis by vital pulp therapy.[8,22,24,25] Visual analysis of 6 months post-operative IOPA radiographs showed significantly faster dentine bridge formation by approximately 12 weeks (P = 0.042) below the MTA with CHX group (80%) as compared to MTA with normal saline group (50%). However, at 12 months, dentine bridge was formed in 90 percent of permanent molars in both groups, which showed MTA partial pulpotomy was the significantly effective procedure in dentine bridge formation (P = 0.000) irrespective of CHX use. Significant dentine bridge formation with MTA has been reported in the literature.[26-29] Complete quantitative analysis of percentage increase in protective radio-opacity showed a significantly higher mean of dentine bridge formation under pulp capping agent (1.5 times) in the study group. Similar radiographic findings have been reported by Mass and Zilberman in 2011. Alves et al., 2010 conducted a 10-year prospective study on qualitative and quantitative radiographic assessment of sealed carious dentin and found that sealing of carious dentin arrested caries, promoted deposition of tertiary dentin, and induced mineral gain in the radiolucent zone.[30]
We did a two-dimensional examination in our study to avoid additional radiation exposure from CBCT. American association of pediatric dentistry suggests avoiding 3-dimensional radiography radiation exposure for children as they are more sensitive to radiation (lifetime risk for cancer incidence and mortality per unit dose of ionizing radiation are higher), and they have a longer lifetime for ill-effects to develop. Further research on immature teeth partial pulpotomy is required to assess the treatment results of new biocompatible agents as applicable to the adult population. The use of biologically accurate diagnostic techniques and bioengineered medicaments should provide a broader scope for vital pulp therapy procedures.[1]
CONCLUSION
MTA, when used with CHX gluconate 0.12% as cavity antiseptic agent for hemostasis after pulp amputation in partial pulpotomy and as a solvent for MTA capping, leads to faster and thicker bridge formation along with uninterrupted maturogenesis probably by providing the required physiologically favorable environment for a natural protective mechanism for healing in an immature permanent carious molar. The use of CHX as an antiseptic agent in MTA partial pulpotomy should be promoted over normal saline for faster recovery of pulp and success of treatment to save immature, deeply carious permanent posterior teeth in children.
Limitation
More extensive studies in terms of the period and sample size are required to confirm the findings.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Partial pulpotomy for immature permanent, its present and future. Pediatr Dent. 2002;24:29-32.
- [Google Scholar]
- A clinical and microbiological study of deep carious lesions during stepwise excavation using long treatment intervals. Caries Res. 1997;31:411-7.
- [CrossRef] [PubMed] [Google Scholar]
- Vital pulp therapy in cariously exposed permanent teeth and its limitations. Aust Endod J. 2002;28:29-37.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective clinical study of mineral trioxide aggregate for partial pulpotomy in cariously exposed permanent teeth. J Endod. 2006;32:731-5.
- [CrossRef] [PubMed] [Google Scholar]
- Therapy conductive to healing of the human pulp. Oral Surg Oral Med Oral Pathol. 1972;34:122-30.
- [CrossRef] [Google Scholar]
- Use of enamel matrix derivative in partial pulpotomy. Int Endod J. 2009;42:584-92.
- [CrossRef] [PubMed] [Google Scholar]
- Partial pulpotomy another treatment option for cariously exposed permanent molars. J Dent Child. 1995;62:342-5.
- [Google Scholar]
- Calcium hydroxide vs MTA aggregate for partial pulpotomy of permanent teeth with deep caries. Eur Arch Paediatr Dent. 2007;8:99-104.
- [CrossRef] [PubMed] [Google Scholar]
- Long term radiographic evaluation after partial pulpotomy in young permanent molars. Quintessence Int. 2011;42:547.
- [Google Scholar]
- Partial pulpotomy in young permanent teeth with deep carious lesions. Endod Dent Traumatol. 1993;9:238-42.
- [CrossRef] [PubMed] [Google Scholar]
- Mineral trioxide aggregate: A comprehensive literature review--Part I: Chemical, physical, and antibacterial properties. J Endod. 2010;36:16-27.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of setting properties and retention characteristics of MTA when used as a furcation perforation repair material. J Endod. 1998;24:768-71.
- [CrossRef] [Google Scholar]
- Pulpal response to nano hydroxyapatite, mineral trioxide aggregate and calcium hydroxide when used as a direct pulp capping agent: An in vivo study. J Clin Pediatr Dent. 2014;38:201-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of white and gray mineral trioxide aggregate (MTA) simulating a one-or two-step apical barrier technique. J Endod. 2004;30:876-9.
- [CrossRef] [PubMed] [Google Scholar]
- Partial pulpotomy and tooth reconstruction of a crown-fractured permanent incisor: A case report. Quintessence Int. 2003;34:740-7.
- [Google Scholar]
- Contemporary perspectives on vital pulp therapy: Views from the endodontists and pediatric dentists. Pediatr Dent. 2008;30:261-7.
- [Google Scholar]
- Multifaceted use of pro root MTA root canal repair material. Pediatr Dent. 2001;23:326-30.
- [Google Scholar]
- The effects of chlorhexidine gluconate (0.12%) on the antimicrobial properties of tooth-colored pro root mineral trioxide aggregate. J Endod. 2004;30:429-31.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of chlorhexidine on the antibacterial effects of MTA. Quintessence Int. 2012;43:901-6.
- [Google Scholar]
- Effect of intensive treatment with chlorhexidine on number of Streptococcus mutans in saliva. Scand J Dent Res. 1981;89:445-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative study of the antimicrobial efficacy of chlorhexidine gel, chlorhexidine solution and sodium hypochlorite as endodontic irrigants. Braz Dent J. 2007;18:294-8.
- [CrossRef] [PubMed] [Google Scholar]
- A long-term retrospective clinical study on MTA pulpotomies in immature permanent incisors with complicated crown fractures. Eur J Paediatr Dent. 2014;15:29-34.
- [Google Scholar]
- Pulpotomy in caries-exposed immature permanent molars using calcium-enriched mixture cement or mineral trioxide aggregate: A randomized clinical trial. Int J Paediatr Dent. 2013;23:56-63.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of mineral trioxide aggregate (MTA) versus calcium hydroxide cement (Dycal) in the formation of a dentine bridge: A randomised controlled trial. Int Dent J. 2012;62:33-9.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic evaluation of immature traumatized incisors following different endodontic treatments. Dent Traumatol. 2021;37:330-7.
- [CrossRef] [PubMed] [Google Scholar]
- Conservative management of mature permanent teeth with carious pulp exposure. J Endod. 2020;46:S33-41.
- [CrossRef] [PubMed] [Google Scholar]
- Is partial pulpotomy in cariously exposed posterior permanent teeth a viable treatment option? Evid Based Dent. 2020;21:112-3.
- [CrossRef] [PubMed] [Google Scholar]
- Qualitative and quantitative radiographic assessment of sealed carious dentin: A 10-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:135-41.
- [CrossRef] [PubMed] [Google Scholar]







