Effect of purified Shilajit (Asphaltum punjabianum) on oxidative stress, arterial stiffness and endothelial function in elderly with hypertension: A randomised controlled study
*Corresponding author: Kasturi A. Patil, Department of Rasashastra and Bhaishajya Kalpana (Medicinal Chemistry and Pharmacy), BLDEA’S AVS Ayurveda Mahavidyalaya, Vijayapura, Karnataka, India. drrenupatil@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patil SG, Patil KA, Sarashetti R, Hadimur K. Effect of purified Shilajit (Asphaltum punjabianum) on oxidative stress, arterial stiffness and endothelial function in elderly with hypertension: A randomised controlled study. Indian J Physiol Pharmacol 2023;67:197-204.
Abstract
Objectives:
Growing evidence showed involvement of vascular oxidative stress in the development of endothelial dysfunction, arterial stiffness and hypertension. Many clinical trials of antioxidants have proven unsuccessful in prevention of atherosclerosis and cardiovascular events. There is a need of new therapies that reduce age- and hypertension associated arterial stiffness in elderly individuals. We aimed to determine if shilajit (Asphaltum punjabianum), a natural phytocomplex which is immunomodulator, anti-inflammatory, antioxidant and antiaging, can reduce oxidative stress and improve arterial function in the elderly with hypertension.
Materials and Methods:
A parallel arm, open-label randomised controlled study was conducted on 60 elderly patients with hypertension. Study-group participants received shilajit (500 mg-twice/day for 30 days) with antihypertensives while control-group participants received only antihypertensive therapy. Oxidative stress, arterial stiffness and endothelial function markers were assessed at baseline and after 30 days of treatment.
Results:
Between-group analysis showed a significant decrease in oxidative stress markers: Malondialdehyde (P < 0.001) and oxidised-low-density lipoproteins (P = 0.015); and increase in total antioxidant capacity (P = 0.002), superoxide dismutase (P < 0.001) and reduced glutathione (P < 0.001) with complementary therapy of shilajit. There was no change in the markers of arterial stiffness and endothelial function.
Conclusion:
These findings suggest that shilajit may be of value as a natural antioxidant to reduce oxidative stress in elderly hypertension patients.
Keywords
Shilajit
Hypertension
Oxidative stress
Arterial stiffness
Elderly
INTRODUCTION
Hypertension along with aging is a major risk factor for cardiovascular (CV) morbidity and mortality in elderly. Hypertension is more prevalent in the elderly ranging from 50% to 75%. It has been estimated that two out of three older adults suffer from hypertension. Several age-related physiological changes in the CV system and its regulatory mechanisms are attributed for the elevation of blood pressure (BP) in the older adults. Age-associated stiffening of artery and endothelial dysfunction are the major contributors for the development of hypertension.[1] Arterial stiffness is an independent and strong predictor of CV morbidity and mortality in hypertensive patients without any overt CV disease[2,3] and also in well-functioning older adults.[4]
Growing evidence has showed the involvement of vascular oxidative stress in the development of endothelial dysfunction, arterial stiffness and hypertension.[5-7] An imbalance between the reactive oxygen species (ROS) production (superoxide radicals, hydrogen peroxide, hydroxyl radical and singlet oxygen) and antioxidant defence system of the body results in oxidative stress.[7] If the level of ROS is not maintained at an optimum level, it can cause damage to the macromolecules such as proteins, DNA and RNA and cell membrane. Increased vascular oxidative stress reduces the bioavailability of nitric oxide (NO) (product of endothelium and vasodilator) and damages the endothelium, leading to impairment in endothelium-dependent vasodilation with resultant enhanced vascular tone, stiffness of artery and thus hypertension.[8,9] Reduction in oxidative stress may improve arterial function and prevent the complications associated with hypertension in elderly. Many clinical trials of antioxidants have proven unsuccessful in prevention of atherosclerosis and CV events.[10-12] Hence, there is a need of new therapies to reduce age- and hypertension associated arterial stiffness in older individuals.
Shilajit (Asphaltum punjabianum), a naturally occurring herbomineral, is a safe and potent dietary supplement which is widely used in Ayurveda and Siddha (Indian traditional systems) as a rasayan (rejuvenator) for disease prevention, longevity and improving the quality of life. It is used as panacea for several ailments in traditional medicine. Even though shilajit is in use for centuries in traditional medicine and claimed to be effective for many diseases, its systematic clinical evaluation on humans is lacking. Shilajit is a brown to blackish natural product that oozes out from layers of mountainous rocks due to strong heat during summer. This organic exudate is formed by gradual decomposition of certain plants by the microorganisms for centuries. It is mainly composed of humus, organic plant material that was compressed by layers of rock in mountains, minerals and fulvic acid. Perennial grasses, legumes, litter and latex of plants are the common plants sources of humus. It is available in Russia, Tibet and Afghanistan but most commonly found in India especially in the Himalayan mountains.[13,14] Experimental evidence shows that shilajit is an immunomodulator, anti-inflammatory, antioxidant and anti-aging.[13,15-17] Thus, we hypothesised that a complementary therapy of shilajit with antihypertensive drugs may improve endothelial function and arterial stiffness by reducing vascular oxidative stress and inflammation. Therefore, the present study was aimed to determine if shilajit as an adjunct with antihypertensive medicines induces favourable modulation in oxidative stress, endothelial function and arterial stiffness in elderly patients with hypertension.
MATERIALS AND METHODS
Ethics
Ethical approval of the study was obtained from the Institutional Ethical Committee. Research objectives and protocol of the study was explained to the patients and their written consent was taken before their enrolment for the study. The guidelines of ICMR for biomedical research and declaration of Helsinki have been followed during the entire study.
Study population and design
A parallel arm, open-label randomised controlled study was conducted on elderly patients (n = 66) with hypertension with age ranging from 60 to 80 years. A total of 60 patients was required for this two-treatment parallel-design study. Considering 95% confidence level, 80% power and between-group mean difference of 1.2 m/s with standard deviation of about 1.5 (in arterial stiffness), the sample size was calculated as 66. Subjects of either sex with systolic BP (SBP) and diastolic BP (DBP) between 140–159 mmHg and 90–99 mmHg, respectively, or those taking antihypertensive drugs were included for the study. Subjects with secondary hypertension, diabetes mellitus, chronic kidney disease, those receiving any regular medical treatment other than antihypertensive drugs, herbals or vitamins supplementation; and history of alcoholism (alcohol abuse) and cannot refrain from alcohol consumption during the study period were excluded from the study. Patients were screened for eligibility from BLDEA Ayurveda Mahavidyalaya Hospital, India and Shri B. M. Patil Medical College, Hospital and Research Centre, India. Eligible patients were allocated to study or control group using randomisation (random number table) method. The study has been registered prospectively in clinical trial registry – India: CTRI/2016/04/006878.
Intervention
Participants of study group received purified shilajit (500 mg twice per day) as a complimentary medicine with antihypertensive therapy while control group participants received only antihypertensive therapy for 30 days.
Purification of shilajit: The source of the shilajit was from Himalayan Mountain, India. Shilajit was purified using traditional Ayurvedic method by treating it with herbal decoction known as Triphala Kwatha (1:3 ratio). Triphala kwatha was prepared using triphala powder and water (1:16 ratio). Triphala powder consists of equal proportion of three fruits namely, Amalaki (Emblica officinalis), Bibhitaki (Terminalia bellirica) and Haritaki (Terminalia chebula). One part of triphala powder was mixed in 16 parts of water and boiled until the mixture was reduced to 1/8th of its initial quantity on moderate flame with constant stirring. The contents were filtered using clean cloth and decoction was obtained.[18] This freshly prepared triphala kwatha was used for purification of shilajit. One part of shilajit and three parts of triphala kwatha (1:3 ratio) was taken, mixed well and dissolved completely. The impurities were removed by filtering the mixture. The filtrate was boiled on moderate flame until the mixture attains semisolid consistency. It was then poured on a plate which was smeared with ghee and kept for drying. A standardisation and quality control aspect of shilajit was followed as per the traditional method (colour, taste, odour, texture and water solubility test). After complete drying shilajit was collected from plate, powdered and encapsulated (500 mg).[19]
Dosage regimen of purified shilajit: Several studies have proved that shilajit is safe at doses of 0.2–5.0 g/kg body weight.[20,21] Recommended dosage of shilajit varies during health and disease. About 125 mg–1 g/day is recommended for patients while for healthy people 10 g–40 g/day as a rasayan.[22] Based on the history of dosage and duration of treatment with shilajit for elderly patients in Ayurvedic hospitals, findings of our unpublished data and a documented clinical study,[23] an oral administration of 500 mg twice a day for 4 weeks was selected for the present study.
Composition of purified shilajit: A chemical analysis of purified shilajit has shown the presence of the following substances: (1) Organic matter (90.4%) such as fulvic acid, humic acids, humins; (2) inorganic elements such as sodium (0.54 ± 0.011%), potassium (1.23 ± 0.02%), magnesium (0.48 ± 0.005%), calcium (2.83 ± 0.06%), manganese (0.015 ± 0.001%), iron (0.77 ± 0.015%), cobalt (0.00042 %), Nickel (0.00019%), copper (0.0051 ± 0.00035%), zinc (0.13 ± 0.01), arsenic (<0.00006%), selenium (<0.0001%), bismuth (<0.00007%), lead (0.017 ± 0.0015%), silver (0.0014 ± 0.0001%), aluminium (0.070 ± 0.0005%), cadmium (<0.00009%), phosphorus (0.31 ± 0.007%), antimony (<0.00004%) and inorganic elements as oxides such as Na2O (0.75 ± 0.02%), K2O (1.48 ± 0.028%), MgO (0.80±0.008%), CaO (3.96 ± 0.084%), Fe2O3 (1.10 ± 0.02%), NiO (0.00024%), CuO (0.0064 ± 0.0004%), ZnO (0.16 ± 0.012%), AS2O3 (<0.0006%), SeO2 (<0.001%), Bi2O3 (<0.0007%), Sb2O3 (<0.0004%), PbO (0.018 ± 0.0016%), AgO (0.0016 ± 0.001%), Al2O3 (0.19 ± 0.00094%) and PO4 (0.31 ± 0.007%) SiO2 (0.82 ± 0.03%).
Data collection
Data were collected in the morning between 8.00 h and 10.00 h after supine rest for 10 min at room temperature. Venous blood samples for the estimation of biochemical parameters were collected in the morning after an overnight fasting.
Body mass index (BMI): Height (cm) was measured using stadiometer (BIOCON™) mounted on the wall. Weight (kg) was measured using a weighing machine. BMI was estimated from weight in kilograms (kg) divided by height in meters squared (m2) and was expressed as kg/m2.
BP: As BP is more variable in older adults, so an average of nine BP readings was taken.[1] Brachial BP was measured thrice with an interval of one min on every visit for 3 consecutive days in a sitting posture using mercury sphygmomanometer. Pulse pressure was estimated as the difference between SBP and DBP. Mean arterial pressure was estimated by adding 1/3rd of pulse pressure to the DBP.
Heart rate: It was measured using a non-invasive automated digital device (Periscope, Genesis Medical Systems, India).
Oxidative stress and antioxidants: Oxidative stress markers such as malondialdehyde (MDA) and oxidised low-density lipoprotein (Ox-LDL); and antioxidants such as total antioxidant capacity (TAOC), superoxide dismutase (SOD) and reduced glutathione (GSH) were estimated. Serum MDA was estimated by Satoh method,[24] Ox-LDL was estimated by enzyme-linked immunosorbent assay (ELISA) method (Biospes Co. Ltd, China). SOD activity was measured by Marklund and Marklund method.[25] Blood reduced glutathione was estimated by Beutler et al. method.[26] TAOC in serum was estimated by ELISA method (Biospes Co. Ltd, China).
Assessment of arterial stiffness: Arterial stiffness was assessed by oscillometric method using a non-invasive digital device (Periscope, Genesis Medical Systems, India). Periscope is a validated 8-channel real time PC-based simultaneous acquisition (200 samples/second) and CV analysis system.[27] Arterial pressure waveform from four limbs (brachial and tibial arteries) and ECG were recorded simultaneously for 10 s and were stored in the computer for further analysis. Brachial-ankle pulse wave velocity (baPWV) was estimated by dividing the distance between the sampling points and pulse transit time elapsed between brachium and respective ankle. The carotid-femoral pulse wave velocity (cfPWV) was calculated automatically by the device using the regression equation (0.8333*Avg.baPWV-233.33) and composite baPWV found out by averaging left and right baPWV.[28]
-
Assessment of endothelial function: Biomarkers of endothelial system were estimated.
Asymmetric dimethylarginine (ADMA): It is an endogenous competitive inhibitor of NO synthase. It competes with L-arginine and reduces vascular nitric oxide production.[29] Lesser the ADMA better is the endothelial function. ADMA was estimated by ELISA method (Biospes Co. Ltd. China).
Total NO concentration (NOx): It is a key molecule of endothelium that maintains vascular homoeostasis. Reduction in bioavailability of NOx results in endothelial dysfunction. It was measured by kinetic cadmium-reduction method.[30]
Endothelial NO synthase (eNOS): This enzyme is responsible for the production of NO in the vascular endothelium. eNOS was quantified by ELISA Method (Biospes Co. Ltd. China).
Endothelin-1 (ET-1): It is a potent vasoconstrictor and a product of vascular endothelial cells. Lesser the ET-1 better is the endothelial function. ET-1 was estimated by ELISA Method (Biospes Co. Ltd. China).
Other biochemical parameters: Fasting blood glucose, lipid profile, urea and creatinine were measured using commercial diagnostic kits (Erba Diagnostics Mannheim Gmbh, India).
Statistical analysis
Blinding was done at analysis level. Persons who were handling and analysing the data were kept blinded. Normality tests were used to evaluate the distribution of data. Statistical significance was established at P < 0.05. The obtained data were expressed in mean and standard deviation. An unpaired-t-test was used to find the difference in baseline characteristics between two groups. Paired-t-test (for normal distribution data) and Wilcoxon signed-rank test (for non-normal distribution data) were applied to determine the significant difference between pre-intervention and post-intervention values within the group. Analysis of covariance was used to find the differences between groups.
RESULTS
Consolidated statement of randomised trial (CONSORT)
The details of participant flow through the study are depicted in CONSORT diagram [Figure 1]. A total of 92 patients were screened for eligibility, from which 26 subjects were excluded (20 subjects were not meeting inclusion criteria and six subjects declined to participate) and 66 participants were selected as per our selection criteria. After randomisation, eligible participants were allocated to study group (n = 33) and control group (n = 33). Six participants were lost during follow-up (five patients from study group and one patient from control group). Post-intervention investigation of 28 participants from the study group and 32 participants from the control group was done. Finally, a data of 60 patients was analysed.
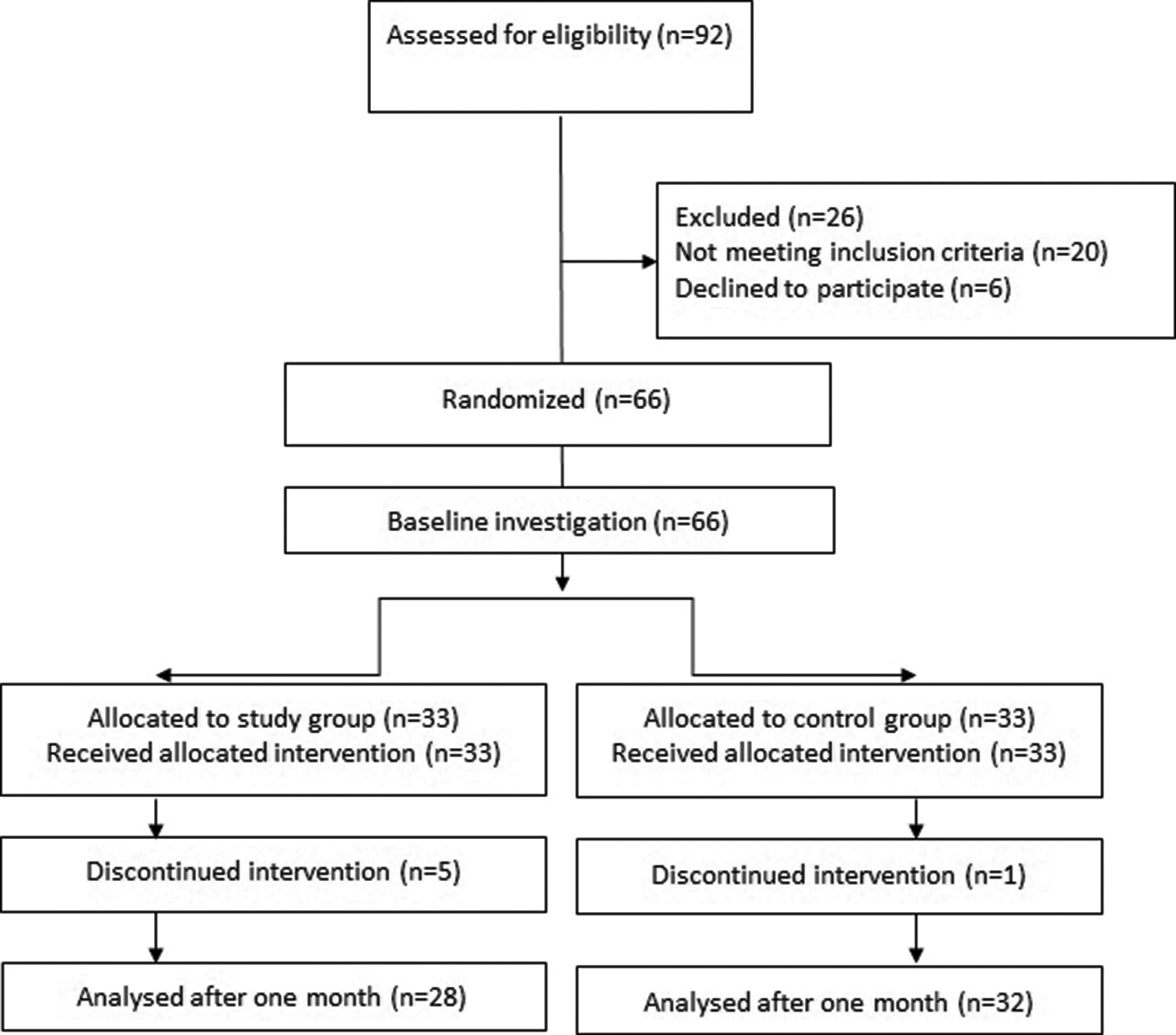
- Consolidated statement of randomised trial diagram. n: Denotes number of participants
Baseline characteristics of participants
The baseline characteristics of the participants (n = 60) are shown in [Table 1]. Mean age of the patients was about 66 years. There were 38 male and 22 female participants. BMI of study and control group participants was 24.99 ± 2.24 and 24.04 ± 2.42 respectively. There was no significant difference in baseline values between the two groups.
| Variable | Study group (n=28) | Control group (n=32) | P-value |
|---|---|---|---|
| Mean±SD | Mean±SD | ||
| Age (years) | 66.29±3.63 | 66.91±3.39 | 0.499 |
| Sex (M/F) | 18/10 | 20/12 | - |
| BMI (kg/m2) | 24.99±2.24 | 24.04±2.42 | 0.12 |
| Systolic BP (mmHg) | 142.18±16.56 | 140.34±14.52 | 0.449 |
| Diastolic BP (mmHg) | 81.25±7.87 | 79.81±7.35 | 0.652 |
| Pulse pressure (mmHg) | 60.93±13.08 | 60.53±12.85 | 0.469 |
| MAP (mmHg) | 101.64±9.72 | 100.06±8.37 | 0.906 |
| HR (bpm) | 69.79±8.26 | 71.51±9.35 | 0.452 |
| Fasting blood glucose (mg/dL) | 93.28±11.32 | 92.25±12.06 | 0.733 |
| Serum triglyceride (mg/dL) | 109.05±23.5 | 105.25±20.5 | 0.399 |
| Total cholesterol (mg/dL) | 152.36±24.01 | 150.81±24.25 | 0.805 |
| HDL cholesterol (mg/dL) | 47.04±4.03 | 46.22±4.26 | 0.874 |
| Urea | 27.4±4.9 | 26.53±4.5 | 0.528 |
| Creatinine | 1.03±0.2 | 1.15±1.21 | 0.459 |
| Antihypertensive therapy, (%) | |||
| Use of CCBs | 18 (64.28) | 20 (62.5) | -- |
| Use of beta blockers | 10 (35.71) | 13 (40.63) | -- |
| Use of ARBs | 05 (17.85) | 06 (18.75) | -- |
| Use of diuretics | 08 (28.57) | 10 (31.25) | -- |
| Use ACE inhibitors | 2 (7.14) | 2 (6.25) | -- |
Unpaired t-test was applied to determine the difference between the baseline values of study and control group; BMI: Body mass index, MAP: Mean arterial pressure, HR: Heart rate, ACE: Angiotensin converting enzyme, ARBs: Angiotensin receptor blockers, CCBs: Calcium channel blockers, BP: Blood pressure, HDL: High-density lipoprotein, n: Denotes number of participants, SD: Standard deviation, M/F: Male/Female
Oxidative stress
There was a significant reduction in MDA (0.46 ± 0.34 vs. −0.04 ± 0.22; P < 0.001) and Ox-LDL (3.14±6.29 vs. −1.9 ± 5.87; P = 0.015) and significant enhancement in SOD (−0.19 ± 0.41 vs. 0.15±0.37: P < 0.001), GSH (−2.92 ± 4.87 vs. 0.04 ± 3.08; P < 0.001) and TAOC (P = 0.002) in the study group than the control group participants. Within-group analysis showed a significant decrease in oxidative stress markers (MDA and Ox-LDL) and significant increase in antioxidants (SOD, GSH and TAOC) in study group with no change in the control group participants [Table 2].
| Parameters | Study group | Control group | Between group | |||||
|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Mean change | Pre-test | Post-test | Mean change | ANCOVA | ||
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean change | P-value | |
| MDA (nmol/mL) | 2.02±0.38 | 1.55±0.38 | 0.46±0.34b*** | 1.76±0.37 | 1.81±0.37 | −0.04±0.22a | 0.5 | <0.001*** |
| Ox-LDL (μg/L) | 43.59±8.79 | 40.46±7.38 | 3.14±6.29a* | 38.61±9.37 | 40.51±9.95 | −1.9±5.87b | 5.04 | 0.015* |
| SOD (U/mL) | 2.53±0.92 | 3.17±0.77 | −0.63±0.97b** | 1.86±0.92 | 1.78±0.91 | 0.08±0.27a | −0.71 | <0.001*** |
| GSH (mg/dL) | 18.36±6.69 | 21.28±5.77 | −2.92±4.87a*** | 18.41±7.17 | 18.36±6.99 | 0.04±3.08b | −2.96 | <0.001*** |
| TAOC (U/mL) | 1.94±0.53 | 2.13±0.57 | −0.19±0.41a* | 2.05±0.41 | 1.89±0.44 | 0.15±0.37a | −0.34 | 0.002** |
*P<0.05, **P<0.01, ***P<0.001, aPaired-t-test, bWilcoxon Signed-rank test. ANCOVA: Analysis of covariance test was applied to determine the difference between study and control groups, MDA: Malondialdehyde, SOD: Superoxide dismutase, TAOC: total antioxidant capacity, OxLDL: Oxidised low-density lipoprotein, HDL: High-density lipoprotein, GSH: Glutathione, SD: Standard deviation
Arterial stiffness and endothelial function
There was no significant change in the arterial stiffness markers – baPWV (P = 0.983) and cfPWV (P = 0.552) between group and within-study or control group. We did not find any change in the endothelial markers – ADMA (P = 0.939), NOx (P = 0.111), ET-1 (P = 0.862) and eNOS (P = 0.906) between group and within-study or control group after a 1 month treatment of shilajit with antihypertensive therapy [Table 3].
| Parameters | Study group | Control group | Between group | |||||
|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Mean change | Pre-test | Post-test | Mean change | ANCOVA | ||
| Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean±SD | Mean changes | P-value | |
| baPWV (m/s) | 17.28±3.88 | 17.49±3.29 | −0.21±1.6b | 16.75±3.16 | 17.35±3.98 | −0.6±2.43b | 0.39 | 0.983 |
| cfPWV (m/s) | 11.31±2.17 | 11.12±2.18 | 0.19±1.64a | 11.39±2.05 | 11.41±1.89 | −0.27±0.63b | 0.46 | 0.552 |
| NOx (μmol/L) | 36.79±12.28 | 37.58±11.58 | −0.78±4.09a | 33.56±9.38 | 41.69±12.31 | 1.46±10.08b | −2.24 | 0.111 |
| ET-1 (ng/L) | 38.24±8.94 | 31.87±10.86 | −0.64±13.01b | 35.89±7.13 | 37.59±9.41 | −1.69±8.85a | 1.05 | 0.862 |
| eNOS (pg/mL) | 62.45±10.71 | 58.94±11.55 | 3.5±9.53a | 56.1±14.73 | 53.69±14.42 | 2.41±7.97b | 1.09 | 0.906 |
| ADMA (μmol/L) | 2.92±1.12 | 2.89±0.89 | 0.04±0.79a | 2.93±1.06 | 2.87±0.96 | 0.06±0.98b | −0.02 | 0.939 |
*P<0.05, **P<0.01, ***P<0.001; aPaired-t-test, bWilcoxon Signed-rank test. ANCOVA: Analysis of covariance test was applied to determine the difference between study and control groups, baPWV: Brachial-ankle pulse wave velocity, cfPWV: Carotid-femoral pulse wave velocity, ET-1: Endothelin-1, eNOS: Endothelial nitric oxide synthase, ADMA: Asymmetric dimethylarginine, SD: Standard deviation
Adverse events
No adverse events occurred during the study.
DISCUSSION
We believe that this is first study to report the effect of purified shilajit on oxidative stress and vascular function in elderly patients with hypertension. We observed a significant reduction in oxidative stress and enhancement in antioxidant defence by the combined treatment with shilajit and antihypertensive drug for 1 month. Shilajit did not induce any beneficial change in the arterial stiffness and endothelial function. No adverse effects of shilajit were reported.
Hypertension and arterial stiffness are independent risk factors for CV morbidity and mortality.[31] There is a bidirectional relationship between BP and arterial stiffness.[32] High BP can accelerate the age-related stiffening of arteries. Antihypertensive therapy can effectively control BP but cannot prevent the progression of age-associated stiffening of arteries. On the contrary, it has been reported that arterial stiffness increases at a faster rate in well-controlled treated hypertensive patients when compared to normotensives.[33] Oxidative stress is implicated in the pathophysiology of vascular dysfunction and atherosclerosis.[34] Vascular oxidative stress is involved in inactivation of NO and its reduction in bioavailability. NO is a key molecule of endothelium that is involved in multitude of vascular function: Regulates vascular tone, vascular permeability and antithrombotic properties. Sufficient bioavailability of NO is essential for the vascular integrity and function. Insufficient NO bioavailability results in endothelial dysfunction and decreased vasodilator capacity that is associated with all major CV risk factors such hypertension, diabetes, hyperlipidaemia and atherosclerosis.[8,9] The primary antioxidant defence systems present in the vascular wall to neutralise ROS are endogenous enzymes such as SOD, glutathione peroxidase, catalase, thioredoxin peroxidase and hemeoxygenase.[35]
The present study has showed a significant reduction in oxidative stress markers – MDA (P < 0.001) and Ox-LDL (P = 0.015), and significant increase in TAOC (P = 0.002), SOD (P < 0.001) and GSH (P < 0.001) in patients treated with shilajit and antihypertensive drugs when compared to only antihypertensive therapy. These findings implicate that shilajit can effectively reduce oxidative stress and enhance antioxidant capacity in elderly patients with hypertension. This reduction in oxidative stress can be attributed to the presence of active molecules such as fulvic acid and dibenzo-alpha-pyrones in the shilajit.[13,36] Organic compounds present in the shilajit are broadly grouped into humic substances including fulvic acid, humic acids, humans (80–85% of total organic mass) and non-humic substances (15–20%). Humic substances are formed by the interaction of plants and microorganisms.[15] Fulvic acids are known for its powerful antioxidant actions which have superoxide and hydroxyl radical scavenging properties[37] and complement-fixing activity.[36] Bhattacharya et al. have shown that shilajit has free radical scavenging and antioxidant effects against superoxide, hydroxyl radicals and NO. These antioxidant effects of shilajit were concentration dependent. Shilajit in higher concentration provided greater protection against free radicals.[17] Few clinical studies have also reported a favourable modulation in oxidative stress and antioxidant status by shilajit treatment in diabetic patients[23,38] and healthy individuals.[22] Saxena et al., studied the effect of shilajit on 61 diabetic subjects aged between 31 and 70 years, who were on unchanged dosages of glibenclamide. They administered two capsules of shilajit (500 mg) twice daily for 30 days. They found a significant reduction in oxidative stress and increase in antioxidant (catalase) values.[23] Another randomised controlled study has also exhibited a beneficial modulation in oxidative stress and antioxidants after the treatment with shilajit (500 mg/day) for 1 year in patients with type 2 diabetes.[38]
Growing evidence suggests that preventing vascular oxidative stress and incrementing the bioavailability of NO may mitigate the CV burden and reduce associated risk factors.[34] In our present study, although, there was a reduction in the oxidative stress, shilajit treatment does not exhibit any favourable change in the NOx and other markers of endothelial function in older patients with hypertension. Further, shilajit did not show any benefit on stiffening of arteries. One clinical study[38] has reported an improvement in endothelial function and reduction in arterial stiffness by a treatment with shilajit (250 mg twice in a day) for 1 year in patients with type 2 diabetes. Although the patient population was different, the differences in the outcomes (vascular function) of our study and Niranjan et al.,[38] may be due to the variation in the dosage and duration of shilajit treatment. In our study, 500 mg shilajit was administered twice in a day for 30 days, while Niranjan et al.[38] prescribed 250 mg twice a day for 1 year. We did not follow the patients for longer period after a shilajit administration for 1 month, which might be a limitation of our study. A treatment with shilajit for longer duration may induce beneficial modulation in the endothelial function and arterial stiffness in older patients with hypertension, which needs to be evaluated in future clinical trials.
CONCLUSION
There was significant reduction in oxidative stress and enhancement in antioxidant defence in elderly patients with hypertension after treatment with a combination of shilajit and antihypertensive drugs when compared to only antihypertensive therapy. Shilajit does not induce any favourable change in the arterial stiffness and endothelial function. No adverse effect of shilajit was reported. Thus, shilajit may be of value as a safe and potent natural antioxidant that can be prescribed to reduce oxidative stress and associated complications in elderly hypertension patients. However, there is a need of clinical studies to determine whether long-term treatment with shilajit would induce beneficial modulation in endothelial function, arterial stiffness and other complications associated with hypertension in elderly patients.
Acknowledgement
We sincerely thanks to Dr. Sanjay Kadlimathi (Professor, Department of Medicine, BLDEA’S AVS Ayurveda Mahavidyalaya, India) for clinical examination of the subjects and Govindanagouda Naregal (Department of Biochemistry, Shri B M Patil Medical College, Hospital and Research Centre, India) for assisting in biochemical investigations, and all the participants for their contribution to the study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Rajiv Gandhi University of Health Sciences (RGUHS), Karnataka, India (RGUHS: Adv.Res.:Proposal-AY-255:2015-16).
References
- Hypertension In: Halter JB, Ouslander JG, Tinetti ME, Studenski S, High KP, Asthana S, eds. Hazard’s Geriatric Medicine and Gerontology (6th ed). New York: McGraw Hill Medical Publishers; 2009. p. :975-82.
- [Google Scholar]
- Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension. 1999;33:1111-7.
- [CrossRef] [PubMed] [Google Scholar]
- Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension. 2001;37:1236-41.
- [CrossRef] [PubMed] [Google Scholar]
- Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation. 2005;111:3384-90.
- [CrossRef] [PubMed] [Google Scholar]
- Possible role of oxidative stress in the pathogenesis of hypertension. Diabetes Care. 2008;31(Suppl 2):S181-4.
- [CrossRef] [PubMed] [Google Scholar]
- New and old mechanism associated with hypertension in the elderly. Int J Hypertens. 2012;2012:150107.
- [CrossRef] [PubMed] [Google Scholar]
- Elevation of oxidative stress and decline in endogenous antioxidant defense in elderly individuals with hypertension. J Clin Diag Res. 2017;11:BC09-12.
- [CrossRef] [PubMed] [Google Scholar]
- Oxidative stress and hypertension: Current concepts. Curr Hypertens Rep. 2010;12:135-42.
- [CrossRef] [PubMed] [Google Scholar]
- Oxidative stress and endothelial dysfunction in hypertension. Hypertens Res. 2011;34:665-73.
- [CrossRef] [PubMed] [Google Scholar]
- Why antioxidant therapies have failed in clinical trials. J Theor Biol. 2018;457:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Why have antioxidants failed in clinical trials? Am J Cardiol. 2008;101:14D-9.
- [CrossRef] [PubMed] [Google Scholar]
- Why do antioxidants fail to provide clinical benefit? Curr Control Trials Cardiovasc Med. 2000;1:38-40.
- [CrossRef] [PubMed] [Google Scholar]
- The core structure of Shilajit humus. Soil Biol Biochem. 1992;23:673-80.
- [CrossRef] [Google Scholar]
- Review on shilajit used in traditional Indian medicine. J Ethnopharmacol. 2011;136:1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Interaction of Shilajit with biogenic free radicals. Indian J Chem. 1995;34:596-602.
- [Google Scholar]
- Effects of Shilajit on biogenic free radicals. Phytother Res. 1995;9:56-9.
- [CrossRef] [Google Scholar]
- Rasatarangini of Sadanand Sharma Virchit (11th ed). Delhi, India: Motilal Banarisidas Publications; 2004. p. :591. Ch. 87
- [Google Scholar]
- Sharangadhar Samhita of Adhamalla In: Madhyamkhanda. Varanasi: Choukambhasur Bharati Publications; 2018. p. :144. Ch. 1. Ver. 1
- [Google Scholar]
- Evaluation of safety profile of black shilajit after 91 days repeated administration in rats. Asian Pac J Trop Biomed. 2012;2:210-14.
- [CrossRef] [PubMed] [Google Scholar]
- Shilajit: Evalution of its effects on blood chemistry of normal human subjects. Anc Sci Life. 2003;23:114-9.
- [Google Scholar]
- Modulation of oxidative and antioxidative status in diabetes by Asphaltum panjabinum. Diabetes Care. 2003;26:2469-70.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma lipid peroxide in cerebrovascular disorders determined by a new colorimetric method. Clin Chim Acta. 1978;90:37-43.
- [CrossRef] [PubMed] [Google Scholar]
- Improved method for the determination of blood glutathione. J Lab Clin Med. 1963;61:882-8.
- [Google Scholar]
- Validity and reproducibility of arterial pulse wave velocity measurement using new device with Oscillometric technique: A pilot study. Biomed Eng Online. 2005;4:49.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of arterial stiffness in elderly with prehypertension. Indian J Physiol Pharmacol. 2015;59:16-22.
- [Google Scholar]
- Asymmetric dimethylarginine (ADMA) and endothelial dysfunction: Implications for atherogenesis. Clinics (Sao Paulo). 2009;64:471-8.
- [CrossRef] [PubMed] [Google Scholar]
- Determination of inorganic nitrate in serum and urine by a kinetic cadmium-reduction method. Clin Chem. 1990;36:1440-3.
- [CrossRef] [Google Scholar]
- Arterial stiffness and hypertension-which comes first? Maedica (Buchar). 2017;12:184-90.
- [Google Scholar]
- Arterial stiffness and hypertension: A two-way street? Hypertension. 2005;45:349-51.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period. Circulation. 2002;105:1202-7.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanisms of oxidative stress and vascular dysfunction. Postgrad Med J. 2003;79:195-200.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular oxidative stress: Impact and therapeutic approaches. Front Physiol. 2018;9:1668.
- [CrossRef] [PubMed] [Google Scholar]
- Complement-fixing activity of fulvic acid from Shilajit and other natural sources. Phytother Res. 2009;23:373-84.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of fulvic and humic acids on performance, immune response and thyroid function in rats. J Anim Physiol Anim Nutr (Berl). 2010;94:721-8.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of the effect of purified aqueous extract of shilajit in modifying cardiovascular risk with special reference to endothelial dysfunction in patients with Type 2 diabetes mellitus. Int J Ayurveda Pharma Res. 2016;4:1-7.
- [Google Scholar]







