Translate this page into:
An echocardiographic study of the effect of obesity on systolic and diastolic functions of the left ventricle in hypertensive adults
*Corresponding author: C Mamatha Shree, Assistant professor, Department of Physiology, Sri Devaraj Urs Medical College, Kolar, Karnataka, India. mamtha.shree15@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shree CM, Prashanth KS, Girija B. An echocardiographic study of the effect of obesity on systolic and diastolic functions of the left ventricle in hypertensive adults. Indian J Physiol Pharmacol 2021;65:237-41.
Abstract
Objectives:
The objectives of the study were to examine the effect of obesity on echocardiographic parameters of systolic and diastolic functions of the left ventricle (LV) in asymptomatic hypertensive adults.
Materials and Methods:
A cross-sectional study was conducted with 100 individuals (65 males and 35 females). Their blood pressure and body mass index were recorded following which they were divided into obese hypertensives and non-obese hypertensives. Echocardiographic examination was done, and parameters indicating LV geometry and function were recorded. Data were statistically analysed for differences. An unpaired t-test was used considering P < 0.05 as a significant value.
Results:
Echocardiographic parameters of LV diastolic function were significantly altered in obese hypertensives compared to non-obese hypertensives (P < 0.05). About 58% of non-obese hypertensives and 78% of obese-hypertensives had LV diastolic dysfunction. About 6% of non-obese hypertensives and 8% of obese-hypertensives had LV systolic dysfunction.
Conclusion:
Obesity in hypertensive individuals adds risk for diastolic dysfunction. The number of subjects falling into categories of mild-to-moderate diastolic dysfunction was considerably higher in the obese hypertensives compared to the non-obese hypertensives.
Keywords
Blood pressure
Body mass index
Obese hypertensives
Obesity
Non-obese hypertensives
Echocardiography
Left ventricular geometry
Left ventricular systolic function
Left ventricular diastolic function
INTRODUCTION
Obesity means excess fat deposition in the body.[1] It tremendously increases metabolic and haemodynamic demand, leading to adaptive alterations in cardiac structure and function. Excessive epicardial fat, adipose tissue, increased free fat mass, increased intravascular volume and greater sympathetic drive are a few of the several factors related to obesity that have been implicated in the left ventricle (LV) wall stress that predisposes to changes such as eccentric left ventricular hypertrophy and diastolic dysfunction.[2,3]
Obesity and hypertension are often coexistent.[4] Obesity is thus an additional risk factor, besides playing a role in adding to or increasing the effect of hypertension with respect to cardiac hypertrophy.[3] They have several overlapping mechanisms which significantly influence LV wall thickness, LV geometry, and LV functions. Compounding the problem is the fact that changes in LV function have been reported not only in clinically asymptomatic patients but even also in those with normal ejection fraction and preserved global LV systolic function.
The above factors emphasise the importance of early detection of changes in the LV structure and function in the high-risk population, and also the need for a non-invasive tool to achieve this end.[5] Echocardiography is considered a validated and sensitive technique for measuring and classifying changes in the LV structure and functions.[6]
Hence, the present study was taken up to examine the effect of obesity on systolic and diastolic functions of the LV in asymptomatic hypertensive adults so that the early detection of any dysfunction in asymptomatic individuals through non-invasive echocardiography can help them to get the condition treated at the earliest. We hypothesised that obesity significantly alters the left ventricular functions in hypertensives, even in the absence of clinically evident cardiovascular disease.
Objective
The objective of the study was to examine the effect of obesity on echocardiographic parameters of systolic and diastolic functions of the LV in asymptomatic hypertensive adults.
MATERIALS AND METHODS
A cross-sectional study was conducted between May 2018 and July 2018 at the Department of Physiology, Bangalore Medical College and Research Institute, and Department of cardiology, PMSSY Super Specialty Hospital, attached to the college. Ethical clearance was obtained from the Institutional Ethics Committee.
The sample size required was calculated as 100, based on the previous studies, in consultation with a statistician, using the formula:
n = 2(Zα+ Z1-β)2σ2/d2 where,
Zα = Alpha error
Z (1–β) = Beta error
σ= Standard deviation
d = Effect size
One of the parameters used was IVSd where,
σ= 1.5, Zα = 1.96, Z (1-β) = 0.84 and d= 0.8
Subjects would then be divided into two groups, based on blood pressure and body mass index (BMI) measurements. The two groups were hypertensive subjects without obesity and hypertensive subjects with obesity.
Subjects were chosen by simple random sampling method from the general population of the city and from among the relatives accompanying the patients of the hospital. Participation was enlisted on a voluntary basis. Enrolment in the study was based on the eligibility criteria mentioned below.
Inclusion criteria
Individuals of either gender, in the age group of 40– 75 years
Non-smokers
Subjects who were previously diagnosed with hypertension, with or without treatment and BMI <25 kg/m2 were included in the non-obese hypertensive group[7,8]
Subjects who were previously diagnosed with hypertension, with or without treatment and BMI ≥25 kg/ m2 were included in the obese hypertensive group.
Exclusion criteria
The following criteria were excluded from the study: Subjects with a history suggestive of or diagnosed cardiovascular disorders
Subjects with a history of diabetes mellitus
Smokers and alcoholics
Subjects with a history of neuromuscular disorders
Subjects with a history of chronic respiratory disorders
Subjects with a history suggestive of or diagnosed endocrinal disorders
Subjects with complications of prolonged hypertension such as nephropathy, neuropathy, and peripheral vascular disorders
Subjects on medication that may affect body weight or have cardiotoxic potential
Subjects with a history of chronic renal disorders
Subjects with suspected or established secondary hypertension
Subjects who would be diagnosed with valvular lesions and impaired global/segmental wall motion during the echocardiographic examination.
Informed written consent was taken from subjects who met the above criteria and were willing to participate in the study. A detailed general and medical history was taken using a pre-structured questionnaire after which they were examined clinically and the data were recorded.
Blood pressure measurement
Subjects were asked to rest for 5 min in the supine position and their blood pressure was recorded with a sphygmomanometer and stethoscope by standard procedure. Two readings each of systolic and diastolic blood pressure were taken 10 min apart, and an average of the two readings was considered for tabulation.
BMI
Height was measured with a wall-mounted stadiometer. MCP wall-mounted stature metre 200 cm was used. The subject was made to stand barefoot, in the erect posture, with heels, gluteus, and occiput touching the wall, and height was recorded in centimetres, then converted to metres. Weight was measured using the weighing scale in kilograms with the subject wearing light clothes without footwear. Using these values, BMI was calculated in kg/m2 using the formula BMI = Weight in kgs/square of height in metres.[7,8]
Echocardiography
After recording the above-mentioned parameters, subjects underwent echocardiography. The procedure was done by experienced technicians in the cardiology department of PMSSY Super Specialty Hospital. GE Vivid E9 ultrasound machine was used. All subjects underwent a standard echocardiographic examination in the left lateral position. The echo/Doppler examination included parasternal long- and short- axis views and apical four chamber and five chamber views and subcostal view or suprasternal view in selected cases. For each view, at least three consecutive cardiac cycles were recorded during quiet respiration. The following parameters were obtained from echocardiography.[8]
Parameters measuring LV geometry:
Systolic interventricular septal thickness (IVSs in cm)
LV internal diameter at end systole (LVIDs in cm)
Diastolic interventricular septal thickness (IVSd in cm)
LV internal diameter at end diastole (LVIDd in cm).
Parameters measured to assess systolic function:
Ejection systolic volume (ESV in ml)
Systolic interventricular septal thickness (IVSs in cm)
Ejection fraction (EF in %)
LV internal diameter at end systole (LVIDs in cm)
Parameters measured to assess diastolic function:
LV internal diameter at end diastole (LVIDd in cm)
Diastolic interventricular septal thickness (IVSd in cm)
Ejection diastolic volume (EDV in ml)
Deceleration time (DT in ms)
E/A ratio (E – early diastolic filling velocity and A – late diastolic filling
velocity)
E/é (é – mitral annular velocity)
Iso-volumetric relaxation time (IVRT in ms).
Group values were converted to mean and standard deviation. An unpaired t-test was used to compare the echocardiographic parameters between the two study groups. P < 0.05 was considered statistically significant.
RESULTS
The study was conducted on 100 subjects who were subdivided into two groups. There were 50 subjects in each group. The mean age (in years) of obese hypertensives was 59.3 ± 10.8 of which 29 were male and 21 were female. The mean age (in years) of non-obese hypertensives was 57.12 ± 11.5 of which 36 were male and 14 were female. Age comparison between groups had P = 0.33.
From [Graph 1], 58% of non-obese hypertensives had LV diastolic dysfunction (LVDD) and 78% of obese hypertensives had LVDD.

- Prevalence of the left ventricle diastolic dysfunction among the two study groups.
From [Graph 2], 6% of non-obese hypertensives had LV systolic dysfunction (LVSD) and 8% of obese hypertensives had LVSD.
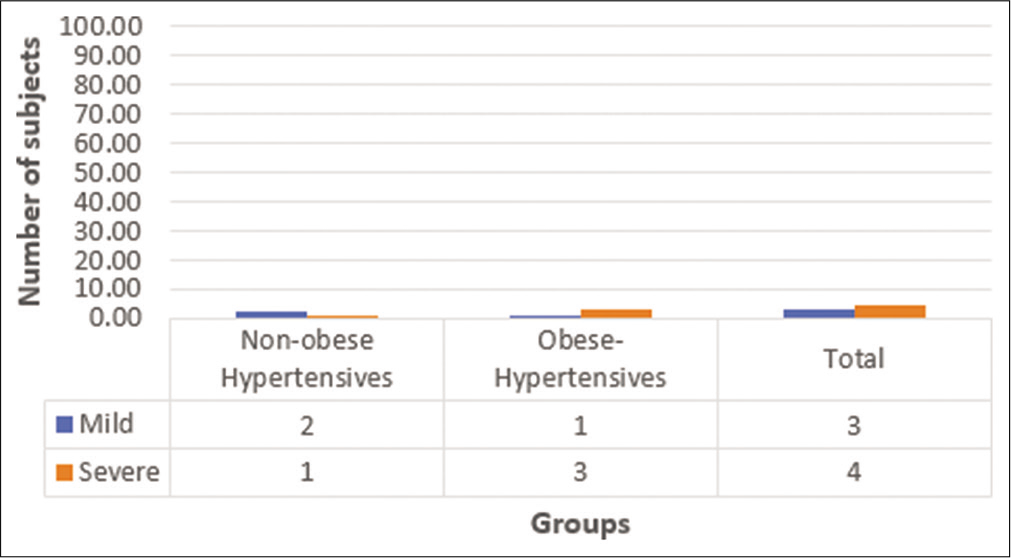
- Prevalence of the left ventricle systolic dysfunction among the two study groups.
DISCUSSION
Obesity and hypertension are the leading independent risk factors for cardiovascular morbidity and are known to cause changes in cardiac structure and function. These changes may, however, remain subclinical for a long time. Early detection of the said changes in apparently asymptomatic individuals may help the timely initiation of corrective measures. Echocardiography, besides being a non-invasive and convenient technique, is a reliable tool for the assessment of cardiac structure and function. Hence, can it be applied for such assessment in the population at risk?
Independent variables in our study were blood pressure and BMI. Based on these, the subjects were grouped into hypertensive individuals with obesity and hypertensive individuals without obesity, as per standard defining values quoted earlier. Between the two groups, values of blood pressure were similar, but the latter group had significantly higher weight and BMI, as confirmed from [Tables 1 and 2]. Hypertension being common to both, presence or absence of obesity was the differentiating feature between them. Intergroup comparison of ECHO parameters in these subjects made it possible to assess the changes in the left ventricular geometry and function in hypertensive individuals with and without obesity.
| Obese hypertensives | Non-obese hypertensives | P-value | |
|---|---|---|---|
| Weight (kg) | 72.68±11.1 | 56±9.5 | <0.001 |
| BMI (kg/m2) | 28.5±2.93 | 21.58±2.9 | <0.001 |
| Obese hypertensives | Non-obese hypertensives | P-value | |
|---|---|---|---|
| SBP (mmHg) | 135±13.1 | 137.96±17.8 | 0.22 |
| DBP (mmHg) | 83.2±7.94 | 85.64±10.1 | 0.09 |
DBP: Diastolic blood pressure, SBP: Systolic blood pressure
Key findings when obese hypertensives were compared with non-obese hypertensives were as follows:
IVSs, IVSd, LVIDs, and LVIDd were not significantly different between the groups. EF and ESV were also similar in the two groups. However, in obese hypertensives, DT and IVRT were significantly prolonged, E/A and E/é were decreased compared to the obese normotensive group from [Table 3]. This indicates that diastolic function parameters were significantly worse among obese hypertensives, even in the absence of evident systolic or global dysfunction.
| Obese hypertensives | Non-obese hypertensives | P-value | |
|---|---|---|---|
| ESV (ml) | 45.6±32.6 | 41.31±18.36 | 0.21 |
| IVSs (cm) | 1.25±0.16 | 1.27±0.16 | 0.24 |
| EF (%) | 58.3±9.3 | 58.7±6.41 | 0.39 |
| LVIDs (cm) | 3.2±0.74 | 3.13±0.51 | 0.28 |
| LVIDd (cm) | 4.64±0.71 | 4.57±0.5 | 0.3 |
| IVSd (cm) | 0.95±0.12 | 0.98±0.15 | 0.14 |
| EDV (m) | 104±41.5 | 99.3±26.67 | 0.26 |
| DT (ms) | 243±54.1 | 225.6±47.3 | 0.04 |
| E/A ratio | 0.84±0.31 | 1.01±0.41 | 0.009 |
| E/é | 6.88±1.8 | 7.85±2.89 | 0.02 |
| IVRT (ms) | 106±16.6 | 93.4±13.4 | <0.001 |
[Graph 1] shows the prevalence of LVDD among the two study groups. About 58% of non-obese hypertensives had LVDD and 78% of obese-hypertensives had LVDD which is significantly higher compared to the other group. It favours the supposition that obesity in hypertensive individuals adds risk for diastolic dysfunction.
[Graph 2] shows the prevalence of LVSD among the two study groups. About 6% of non-obese hypertensives had LVSD and 8% of obese hypertensives had LVSD. No significant difference in the prevalence of systolic dysfunction was noted between the groups.
Obesity and LV functions
Garg et al., in their study, found diastolic dysfunction with normal ejection fraction in 53% of overweight subjects and in 35% of obese subjects.[8] Zarich et al. observed a significant decrease in the maximum velocity of the passive mitral filling (E) among obese patients, whereas the values for active mitral filling (A) were not significantly affected, resulting in a decrease in the E/A ratio. Conversely, Chakko et al. did not find significant differences in the values of E, but values of A were increased, resulting in a decreased E/A ratio. Stoddard et al. found a significant increase in both E and A values, which were positively correlated with the percentage of body weight in excess of the ideal so that the E/A ratio was not altered.[9]
Evrim et al. and several other studies have found that LV ejection fraction is normal to increase in the majority of obese subjects.[10]
Combined effect of hypertension and obesity on LV functions
Gottdiener et al. studied a hospital-based population of at 14 VA medical centres nationwide and found a significant association between both obesity and hypertension and cardiac structure and function. In 2010, Wang et al. reported statistically significant interactions between systolic BP, diastolic BP, and BMI in relation to CVD. Adebiyi et al. found that there was a significant synergistic interaction between BP and BMI on cardiac geometry and left ventricular mass (LVM) index.[7]
Garg et al. in their study observed that when hypertension coexisted with obesity, there was a significant increase in left ventricular posterior wall thickness during diastole, relative wall thickness, and LVM/height. It was also noted that a higher number of obese hypertensive subjects had concentric hypertrophy.[8]
The present study reiterates that in hypertensives with obesity, the left ventricular diastolic functions are worse off than in those without. The changes in the left ventricular function parameters are present in clinically asymptomatic individuals. Furthermore, diastolic functions can be altered even when systolic and global measures were apparently preserved. These changes can be detected by a simple imaging technique.
Implications
The study emphasises the indication for cardiac evaluation aimed at early detection of changes in structure and function before they produce symptoms. Echocardiography is a noninvasive and reliable tool for the assessment of LV geometry and function and may be productively employed in the population at risk of cardiovascular morbidity.
As hypertension and obesity are both modifiable risk factors, suitable and early steps taken to control these will go a long way in preserving and promoting cardiovascular health.
CONCLUSION
Obesity significantly affects LV geometry and diastolic functions of the LV in hypertensives
In the presence of both obesity and hypertension, the prevalence of LVDD is significantly increased
These changes can be detected by echocardiography even in individuals with preserved systolic function.
Acknowledgement
The authors would like to thank Dr. Manjunath, Cardiologist, PMSSY, Bangalore Medical College, and Research Institute, for guiding us throughout the study period. Dr. Manjunath expired in 2020 due to multiple health issues.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Textbook of Medical Physiology (12th ed). Ch. 68. Philadelphia, PA: Saunders; 2011. p. :125.
- [Google Scholar]
- Left ventricular morphology and diastolic function in severe obesity: Current views 1288. Rev Esp Cardiol. 2012;65:1-3.
- [CrossRef] [Google Scholar]
- Left ventricular hypertrophy evaluation in obese hypertensive patients: Effect of left ventricular mass index criteria. Arq Bras Cardiol. 2002;78:341-51.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of hypertension on systolic and diastolic left ventricular function. A tissue doppler echocardiographic study. Am Heart J. 2006;151:1323.e7-11.
- [CrossRef] [PubMed] [Google Scholar]
- Left ventricular diastolic function in hypertension: Relation to left ventricular mass and systolic function. J Am Coll Cardiol. 1984;3:1500-6.
- [CrossRef] [Google Scholar]
- Prevalence of generalized and abdominal obesity in urban and rural India: The ICMR-INDIAB study. Indian J Med Res. 2015;142:139-50.
- [CrossRef] [PubMed] [Google Scholar]
- Echocardiographic partition values and prevalence of left ventricular hypertrophy in hypertensive Nigerians. BMC Med Imaging. 2006;6:10.
- [CrossRef] [PubMed] [Google Scholar]
- Asymptomatic obese hypertensives and need of routine echocardiography for left ventricular mass assessment and treatment. J Clin Diagn Res. 2013;7:1599-603.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of isolated obesity on left ventricular function: A longitudinal strain imaging study. Menoufia Med J. 2014;27:130-5.
- [CrossRef] [Google Scholar]
- The impact of obesity on the left ventricle. JACC Cardiovasc Imaging. 2011;3:266-74.
- [CrossRef] [PubMed] [Google Scholar]






