Translate this page into:
Exploring the health benefits of bhramari pranayama (humming bee breathing): A comprehensive literature review
*Corresponding author: Dipak Chetry, Department of Yoga Science, University of Patanjali, Haridwar, Uttarakhand, India. dipakchetry4u@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chetry D, Chhetri A, Rajak DK, Rathore V. Gupta A. Exploring the health benefits of bhramari pranayama (humming bee breathing): A comprehensive literature review. Indian J Physiol Pharmacol. 2024;68:71-85. doi: 10.25259/IJPP_325_2023
Abstract
Bhramari pranayama is a popular, widely practiced and researched pranayama in yoga that is described in many ancient Indian yoga texts. Several experiments have been conducted on bhramari pranayama to investigate its potential health benefits. The present review aimed to explore all currently available experimental research on bhramari pranayama and its health benefits. We investigate Scopus, PubMed, Cochrane Library and Google Scholar to conduct our literature review. The databases mentioned above were searched in April 2023, and 46 experimental studies between 2006 and 2023 – including 18 single-arm clinical trials, 22 clinically controlled trials (CCTs) and six randomised control trials (RCTs) – were considered in the final evaluation for qualitative synthesis. Bhramari pranayama has been found in RCTs and CCTs to have a positive effect on psychological, cardiovascular and pulmonary health; it may also help those with hypertension and tinnitus lessen the associated symptoms of their conditions. Bhramari pranayama practice is found to be associated with higher levels of attention, quality of sleep, parasympathetic activity and pulmonary functioning and lower levels of stress, anxiety, depression, sympathetic activity and blood pressure across the included studies. This comprehensive review of the literature looked at each experimental trial of bhramari pranayama that examined people’s general health as well as specific medical conditions. To fill in the gaps in the currently available literature, researchers can organise their investigations to address these gaps and carry out more extensive research on bhramari pranayama in the future with the aid of this review.
Keywords
Bee breathing
Bee humming breathing
Bumblebee breathing
Yogic breathing
Yoga breathing
Breathing exercise
INTRODUCTION
The yogic breathing techniques known as Pranayamas, which focus on the breath, are described in several ancient Indian yogic texts written in Sanskrit. In Sanskrit, ‘prana’ refers to the essential life force, while ‘yama’ refers to gain control.[1] Pranayams are one of the most important aspects of yoga, which has been shown to have several positive effects on human physiology.[2-4] Bhramari is one such pranayama, which is popular, widely practiced and researched in yoga.[5] The practice instructions and benefits of bhramari pranayama are described in traditional yoga texts. Traditional texts advised practice instructions for bhramari pranayama, which involves inhaling quickly, producing a sound such as a male bee and exhaling slowly, producing a sound like a female bee. During the practice, one should listen to the inner sounds by closing the ears with the hands. The benefits of this bhramari pranayama are also mentioned in traditional texts, which claim that it enhances mental bliss and aids in Samadhi perfection.[6,7]
Bhramari pranayama has been the subject of many experimental researches that have looked into its potential health benefits. These experimental studies were summarised in reviews of bhramari pranayama with descriptions of their unique review goals. Previously published reviews covered the effects of bhramari pranayama on various health issues (such as tinnitus, stress, deafness and generalised anxiety disorder) and general health, along with instructions for the practice.[5,8-16] Those reviews did not cover the entirety of the available literature on bhramari pranayama, and some of the reviews covering holistic health had few databases to identify available studies, also necessitating the need for an updated version of this review (which was last updated in 2016).[16] Therefore, this review aimed to explore all experimental research on the effects of bhramari pranayama on general health that were currently accessible. To create more thorough experiments on bhramari pranayama for future research, researchers can use this literature review on the practise to identify gaps in the existing knowledge.
METHODS
Sources and search strategy of literature
Our investigation of the literature was based on Scopus, PubMed, Cochrane Library and Google Scholar. In April 2023, the mentioned databases were searched using the search strategy ‘Keywords in title, abstract and keyword’ methodology. The search strategy was adapted to include terms relating to or describing a bhramari pranayama practice (i.e. Bhramari, Bhramari, Bee humming breath, Humming bee breath, Pranayama and Yoga breathing) as search words in the title or abstract or keywords. The electronic search strategy for PubMed was ‘(Bhramari[Title/Abstract]) OR (Bhramari[Title/Abstract]) OR (Bee humming breath*[Title/Abstract]) OR (Humming bee breath*[Title/Abstract]) OR (Pranayama[Title/Abstract]) OR (Yoga breathing[Title/Abstract])’. A similar searching strategy was adopted for Scopus, Cochrane Library and Google Scholar the first hundred results were identified based on the relevance. No limitations of years and restrictions of languages in the database were enforced during the search. In addition, reference lists of included papers were screened for additional eligible papers.
Eligibility criteria of literature
Studies had to meet the following eligibility criteria for study selection: (1) Study types: All experimental studies (which includes single-arm clinical trials, clinically controlled trials and randomised control trials [RCTs]) were considered eligible. On the other hand, conference abstracts, review papers, website articles, case studies, research protocols and publications without peered review were excluded. (2) Intervention types: Studies that included the individual effect of bhramari pranayama practice as an intervention were considered eligible. Studies were excluded if bhramari pranayama was not the intervention or it was combined with other practices. (3) Participant types: Studies conducted on healthy as well as unhealthy human patients with any age groups are eligible. (4) Outcomes types: Studies were eligible if they assessed any health-related outcomes related to any body system were considered eligible. Studies with no related results were excluded from the study.
Data extraction and management
The required pieces of information were extracted and verified. From each included study, the researchers have extracted the design of the study, country of affiliation, year of publications, characteristics of participants (sample size and demographic details of participants, age, gender, etc.), details of interventions, assessments and outcomes. The outcome variables assessed in each study were classified based on the health outcomes observed in the studies (i.e. psychological, cardiovascular, pulmonary variables or if any other health-related variables were found) and those extracted data were used in the required fields.
RESULTS
Following the searched keywords in the mentioned databases, 4704 results were identified; after removing the duplication records, 507 studies were screened and 75 papers were assessed for full-text reading. Twenty-eight studies were excluded with the following reasons: (i) ten studies were review papers,[5,8-16] (ii) six studies assessed different outcome variables,[17-22] (iii) five studies were on bhramari pranayama combined with other practices,[23-27] (iv) four were thesis on bhramari pranayama,[28-31] (v) two studies were not published in the peer-reviewed journals,[32,33] and (vi) two were case studies.[34,35] Forty-six studies were included in the final review for qualitative synthesis.[36-81] The flow diagram of the identified studies is presented in Figure 1.
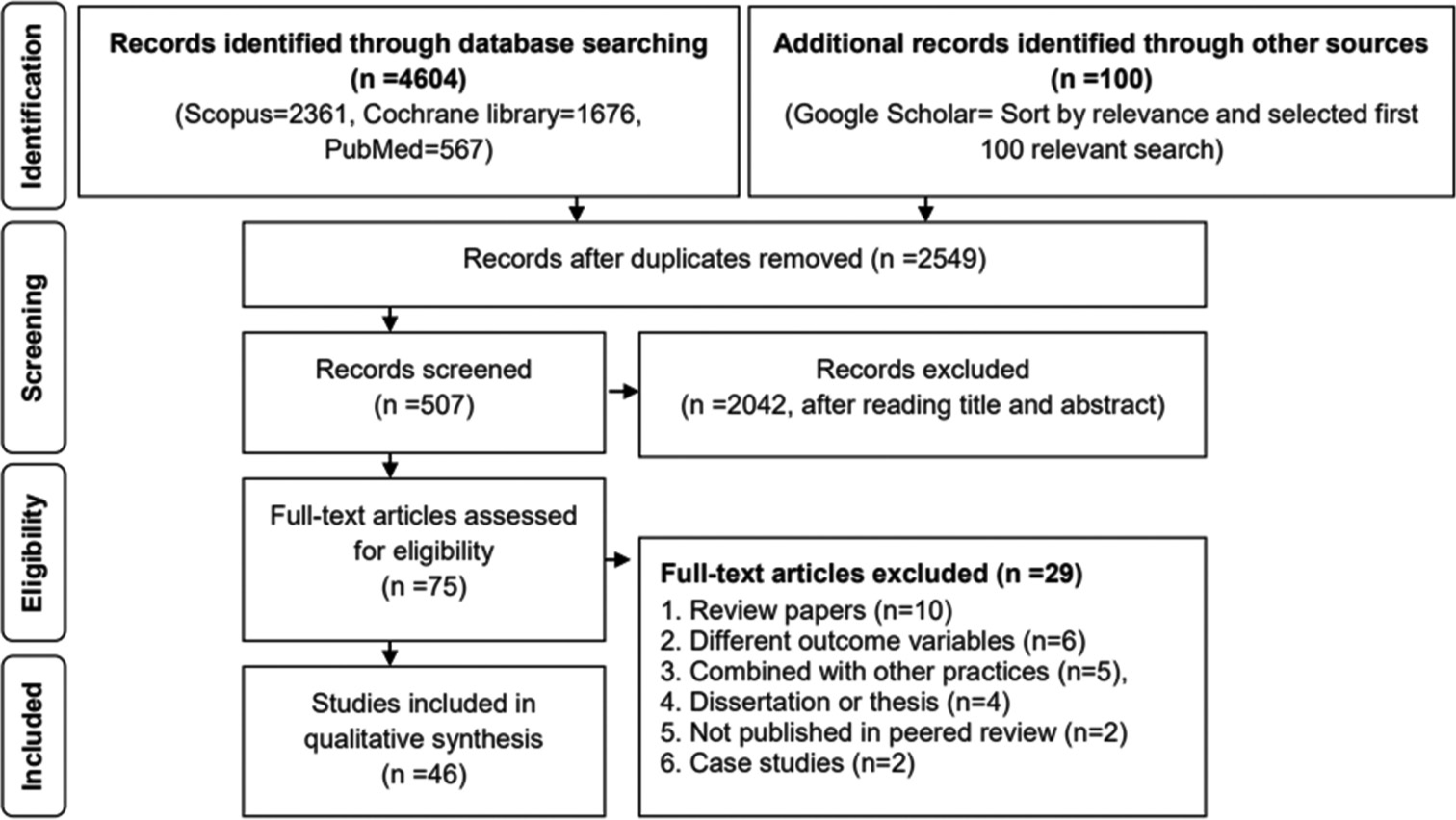
- The flow diagram of the identified literature.
Characteristics of the included literature
The total number of studies included in this review was 46, including 18 single-arm clinical trials, 20 two clinically controlled trials (CCTs) and six RCTs that took place between 2006 and 2023. These 46 trials included a total of 3097 participants: six studies conducted only on males, three studies conducted only on females, 20 eight studies on both sexes and nine studies that did not specify the gender of the participants. The categorised age group of the participants showed that five studies were on adolescents (10–18 years), 31 studies were on adults (19–59 years), three studies were on senior adults (60 years and older), and seven studies did not mention the age group of the participants. The classified geographical regions showed that 38 studies were conducted from India, four studies were from Japan and one study each from Egypt, Nepal, Singapore and Spain. The mean total duration of intervention of the included studies was 10.04 ± 6.63 weeks as well as the mean duration of bhramari practice per day was 16.56 ± 12.88 min.
Twenty-four included studies conducted on bhramari pranayama were on psychological variables [37,41,42,44,45,47,50,54-58,62,63,65,67,70,72,74,76,78-81] followed by 22 studies were on cardiovascular variables[36-40,45,46,48,49,51,52,58,60,61,64,66-69,73,75,77] and five studies were on pulmonary variables.[43,53,57,59,71] The follow-up duration of bhramari pranayama was classified as very short-term (i.e. ≤1 week), short-term (i.e. one week to 3 months), intermediate-term (i.e. ≥ three months to 1 year) and long term (i.e. ≥12 months) showed 22 studies as very short term, 21 studies as short term, three studies as an intermediate-term and no studies showed it for long term. The graded health status of the participants showed that 31 studies were conducted on healthy populations and 15 studies were on patient population {i.e. four studies on hypertension,[48,49,51,52] three studies on tinnitus[40,55,76] and one study each on chronic rhinosinusitis,[53] insomnia,[56] visual impairment,[54] menopausal syndrome,[42] pregnancy,[73] chronic obstructive pulmonary disease,[43] asymptomatic COVID-19[41] and dental patient).[63] The details of each individual included study were presented in Table 1.
| Citation | Study characteristics | Interventions and variables measured | Results |
|---|---|---|---|
| Trivedi et al., 2023[36] | Participants: 23 functional individuals with normal health or with chronic disease, aged between 18 and 60 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 15 min. Assessments were taken during the practice. Variables: Heart rate variability. |
Bhramari pranayama generates the significantly lowest stress index compared to all three other activities (physical activity, emotional stress and sleep). Several additional HRV parameters also supported the positive impact of bhramari pranayamaon the autonomic nervous system (i.e. significant increase in SDNN, Total power and LF/HF ratio), equivalent to stress reduction. |
| Kala et al., 2022[37] | Participants: 38 healthy participants, aged between 20 and 37 years, all males. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 15 min. Assessments were taken at baseline and after 15 min. Variables: P300, Heart rate variability. |
The P300 peak amplitude recorded at Pz was significantly increased after bhramari pranayamacompared to before. No significant changes were noted in heart rate variability. |
| Latha and Lakshmi, 2022[38] | Participants: 110 healthy students, aged between 18 and 22 years, both genders. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama training was given for 15 min (9 cycles) a day for 3 weeks. Assessments were taken at baseline and after 3 weeks. Variables: Blood pressure, heart rate variability. |
There was a significant decrease in Systolic blood pressure, Diastolic blood pressure, PNN50, LFnu and LF/HF ratio. |
| Nirupama et al., 2022[39] |
Participants: 60 healthy volunteers (30 in bhramari group and 30 in the control group), aged between 18 and 30 years, both genders. Study design and country: RCT, India. |
Interventions: Bhramari pranayama was performed for 10 min for 3 months. Assessments were taken before and after 3 months. Variables: Blood pressure, heart rate variability. |
There was a significant decrease in heart rate, LF (n.u), and LF/HF Ratio as well as a significant increase in RR interval, SDNN, RMSDD, NN 50, pNN 50 and HF (n.u) after 3 months. |
| Ismail et al., 2022[40] | Participants: 56 patients of bilateral chronic subjective tinnitus (28 in the bhramari group and 28 in control group), aged ≥65 years, both genders. Study design and country: CCT, Egypt. |
Interventions: Bhramari pranayama was practiced for 30 min a day over 4 weeks. Assessments were taken at baseline and after 4 weeks. Variables: Tinnitus annoyance, tinnitus loudness, tinnitus handicap, systolic pressure, diastolic pressure, pulse rate and respiratory rate. |
Bhramari pranayama practice group has shown a significant reduction in tinnitus annoyance, tinnitus loudness, tinnitus handicap, systolic pressure, diastolic pressure, pulse rate and respiratory rate, whereas no significant changes were observed in the control group after 4 weeks. |
| Jagadeesan et al., 2022[41] |
Participants: 40 asymptomatic COVID-19 patients, aged ≥18 and ≤60 years, both genders. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced for 20 min a day over 15 days. Assessments were taken at baseline and after 15 days. Variables: Depression, anxiety, stress, sleep quality and quality of life. |
Bhramari pranayama practice has shown a significant reduction in scores of depression, anxiety and stress. In addition, the group has also shown a significant improvement in quality of sleep and quality of life after 15 days. |
| Beldar and Bhati, 2021[42] | Participants: 30 patients with menopausal syndrome, aged between 45 to 55 years, females. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced for 10 to 15 repetitions a day over 30 days. Assessments were taken at baseline and after 30 days. Variables: Subjective and clinical symptoms of menopausal syndrome. |
The results showed that after 30 days of bhramari pranayama, there was a significant improvement in the feeling of well-being physical and mental fitness. The results also showed a significant improvement in the clinical symptoms of menopausal syndrome (mainly somatic and psychological complaints) after 30 days. |
| Jayasheela, 2021[43] | Participants: 60 patients with chronic obstructive pulmonary disease (30 in the bhramari group and 30 in the control group), aged over 35 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 25 min 3 times a day over 12 weeks. Assessments were taken at baseline and after 12 weeks. Variables: Dyspnoea scores. |
The results showed that after 12 weeks, there was a significant reduction in dyspnoea scores in the bhramari group. |
| Kumar et al., 2021[44] | Participants: 60 healthy school students, aged between 45 and 55 years, both genders. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced for 45 min a day over 6 weeks. Assessments were taken at baseline and after 6 weeks. Variables: Sleep quality and perceived stress. |
The results showed that after 6 weeks of bhramari pranayama, there was an improvement in sleep quality and perceived stress. |
| Maheshkumar et al., 2021[45] | Participants: 26 healthy participants (13 in the bhramari group and 13 in the control group), aged between 11 and 19 years, both genders. Study design and country: RCT, India. |
Interventions: Bhramari pranayama was practiced for 25 min a day over 6 months. Assessments were taken at baseline and after 6 months. Saliva samples were collected at 4 time points: at baseline, at 20 min, at 40 min and 60 min after the intervention. Variables: Salivary cortisol response to the cold pressor test. |
The results showed that after 6 months of bhramari pranayama, there were significantly higher salivary cortisol levels at 20 min as well as significantly lower salivary cortisol levels at 60 min compared to the control group. |
| Nivethitha et al., 2021[46] |
Participants: 20 healthy participants, mean age 23.40 years, both genders. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced for 5 min. Assessments were taken at baseline, during and after 5 min. Variables: Cardiovascular variables (i.e. systolic blood pressure, diastolic blood pressure, mean arterial pressure, heart rate, stroke volume, cardiac output, pulse interval and total peripheral resistance). |
The results showed that during bhramari pranayama, there was a significant increase in diastolic blood pressure, mean arterial pressure, heart rate and total peripheral resistance with a significant reduction in stroke volume, cardiac output and pulse interval compared to baseline. |
| Sharma et al., 2021[47] | Participants: 38 healthy participants, mean age 24.08 years, all males. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced for 18 min. Assessments were taken at baseline and after 18 min. Variables: State anxiety and sustained attention. |
The result showed a significant decrease in state trait anxiety after 18 min of bhramari practice compared to baseline. |
| Ghati et al., 2020[48] | Participants: 70 hypertensive patients (35 in the bhramari group and 35 in the control group), aged between 30 and 70 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 5 min. Assessments were taken at baseline, during and after 5 min. Variables: Cardiovascular variables (i.e. frequency and time domain components of heart rate variability, systolic blood pressure, diastolic blood pressure, mean arterial pressure, heart rate, stroke volume, arterial stiffness and total peripheral resistance). |
The result showed a significant increase in the HF power (ms2) and a decrease in the LF power (ms2) after the bhramari practice in comparison to the control group. |
| Kuppusamy et al., 2020[49] |
Participants: 520 healthy secondary school students (260 in bhramari group and 260 in the control group), aged between 13 and 18 years, both genders. Study design and country: RCT, India. |
Interventions: Bhramari pranayama was practiced for 25 min a day over 6 months. Assessments were taken at baseline and after 6 months. Variables: Heart rate variability (frequency and time domain components). |
The result showed a significant increase in the time domain variable (i.e. RR, SDNN, RMSSD, NN 50 count, pNN 50) after 6 months of bhramari practice. The result also showed a significant increase in the HF (n.u) and a decrease in the LF (n.u) as well as the LF/HF ratio after 6 months. |
| Kuppusamy et al., 2020[50] |
Participants: 520 healthy secondary school students (260 in bhramari group and 260 in the control group), aged between 13 and 18 years, both genders. Study design and country: RCT, India. |
Interventions: Bhramari pranayama was practiced for 25 min a day over 6 months. Assessments were taken at baseline and after 6 months. Variables: Reaction time (auditory and visual reaction time). |
The result showed a significant decrease in both auditory and visual response time after 6 months of bhramari pranayamapractice. |
| Sathe et al., 2020[51] | Participants: 42 hypertensive participants (21 in bhramari pranayamaand 21 in buteyko breathing), aged above 40 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 5 min. Assessments were taken at baseline and after 5 min. Variables: Blood pressure, pulse rate, oxygen saturation. |
The result showed a significant decrease in systolic blood pressure after bhramari pranayama. |
| Sathe et al., 2020[52] | Participants: 40 hypertensive patients (20 in bhramari group and 20 in the control group), aged >40 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 5 min. Assessments were taken at baseline and after 5 min. Variables: Systolic blood pressure, diastolic blood pressure, heart rate and oxygen saturation. |
The result showed a significant decrease in systolic blood pressure after bhramari pranayama. |
| Abishek et al., 2019[53] | Participants: 60 chronic rhinosinusitis (30 in bhramari group and 30 in conventional treatment), >18 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 15 min twice a day over 12 weeks. Assessments were taken at baseline, after 1 week, after 4 weeks and after 12 weeks. Variables: Sinonasal outcome test. |
The result showed a significant reduction in the sinonasal outcome scores in both groups. The magnitude of change was higher in bhramari group compared to the conventional treatment group. |
| Pradhan et al., 2018[54] | Participants: 19 visual impairment students, aged between 15 and 19 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 10 min. Assessments were taken at baseline and after 10 min. Variables: Attention performance. |
The results showed significant improvement in attention performance after bhramari pranayama. |
| Taneja, 2018[55] | Participants: 80 tinnitus patients (40 in bhramari group and 40 in placebo group), aged ranged between 30 and 70 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced 3 times a day over 3 months. Assessments were taken at baseline and after 3 months. Variables: Associated symptoms and improvement of tinnitus, impact of tinnitus on quality of life, tinnitus frequency. |
The results showed improvement in associated symptoms and quality of life in tinnitus patients after 3 months of Bhramari pranayama. |
| Bhati et al., 2017[56] | Participants: 93 insomnia patients (31 in bhramari group, 31 sleep hygiene group and 31 in bhramari+ sleep hygiene group), ages ranged between 16 and 60 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced over a period of 3 months. Assessments were taken at baseline and after 3 months. Variables: Sleep quality. |
The results showed significant improvement in sleep quality in insomnia patients after three months. |
| Bhushan et al., 2017[57] | Participants: 90 healthy cricket players (45 in bhramari group and 45 in the control group), ages ranged between 18 and 24 years, males. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced 5 min a day for 6 days a week over 12 weeks. Assessments were taken at baseline and after 12 weeks. Variables: Vital capacity, prakriti (psycho-somatic constitution). |
The results showed a significant increase in vital capacity, vata, pitta and kapha after Bhramari pranayama. |
| Bhushan et al., 2017[58] | Participants: 90 healthy cricket players (45 in bhramari group and 45 in the control group), ages ranged between 18 and 24 years, males. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced 5 min a day for 6 days a week over twelve weeks. Assessments were taken at baseline and after 12 weeks. Variables: Cardiorespiratory endurance, prakriti (psycho-somatic constitution). |
The results showed a significant increase in cardiorespiratory endurance after 12 weeks of bhramari pranayamain cricket players. The results also showed that cricketers having pitta prakriti have significantly higher cardio-respiratory endurance after bhramari pranayama. |
| Kuppusamy et al., 2017[59] |
Participants: 90 healthy adolescents (45 in bhramari group and 45 in the control group), age ranged between 11 and 18 years, both genders. Study design and country: RCT, India. |
Interventions: Bhramari pranayama was practiced for 45 min 5 days a week over 12 weeks. Assessments were taken at baseline and after 12 weeks. Variables: Pulmonary function test. |
The results showed a significant increase in all pulmonary function parameters (forced vital capacity, forced expiratory volume in 1 s, ratio of forced expiratory volume in 1 s and forced vital capacity, forced expiratory flow 25-75% and peak expiratory flow rate) compared to the control group. The bhramari group also showed a significant increase in slow vital capacity and maximum voluntary volume compared to baseline. |
| Nivethitha et al., 2017[60] |
Participants: 16 healthy volunteers, aged between 18 and 27 years, both genders. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced for 5 min. Assessments were taken at baseline during, and immediately after 5 min of bhramari pranayama. Variables: Heart rate variability. |
The results showed a significant increase in heart rate and low-frequency spectrum (LF n.u) of heart rate variability as well as a significant reduction in the high-frequency spectrum (HF n.u) of heart rate variability during the practice of bhramari pranayamawhich reverted to normal after the practice. |
| Nivethitha et al., 2017[61] |
Participants: 18 healthy volunteers, aged between 18 and 27 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 5 min. Assessments were taken at baseline during, and immediately after 5 min of bhramari pranayama. Variables: Cerebral blood flow velocity. |
The results showed no significant changes were observed in any of the variables of cerebral blood flow velocity in bhramari pranayama. |
| Srivastava et al., 2017[62] | Participants: 60 college students, ages ranging between 16 and 20 years, gender not specified. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced for 15 min over 20 days. Assessments were taken at baseline and after 20 days of bhramari pranayama. Variables: Mental health. |
The results showed a significant improvement in mental health scores after bhramari pranayamacompared to baseline. |
| Kakodhar et al., 2016[63] | Participants: 34 dental patients (17 in bhramari group and 17 in the control group), age ranged between 25 and 50 years, gender not specified. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 10 min. Assessments were taken at baseline, during and after 10 min of bhramari pranayama. Variables: Anxiety and comfort level. |
The results showed a significantly lower anxiety and higher comfort level after bhramari pranayamapractice compared to baseline. |
| Kuppusamy et al., 2016[64] |
Participants: 60healthy adolescents (30 in bhramari group and 30 in the control group), aged between 12 and 18 years, both genders. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 45 minutes. Assessments were taken at baseline, and after 45 min of bhramari pranayama. Variables: Cardiovascular parameters (systolic blood pressure, diastolic blood pressure, heart rate, mean arterial pressure, pulse pressure, rate pressure product, double product). |
The results showed a significant reduction in systolic blood pressure, diastolic blood pressure, heart rate, mean arterial pressure, rate pressure product and double product after 45 min of bhramari pranayama. |
| Malhotra et al., 2016[65] | Participants: 31 healthy participants, age not specified, both genders. Study design and country: Single group CT, India. |
Interventions: The duration of bhramari pranayamais not mentioned. Assessments were taken at baseline and after bhramari pranayama. Variables: Visual reaction time. |
The results showed a significant reduction in reaction time after Bhramari pranayama. |
| Bajpai et al., 2015[66] | Participants: 94 medical students, ages ranged between 17 and 27 years, both genders. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced over 3 months. Assessments were taken at baseline and after 3 months of bhramari pranayama. Variables: Cardiovascular hyper-reactivity to cold pressor test. |
The results showed a reduction in hyper-reactivity to the cold pressor test. Systolic rise of blood pressure, diastolic rise, mean systolic blood pressure and mean diastolic blood pressure were reduced after 3 months of bhramari pranayama. |
| Sahu and Kishore, 2015[67] | Participants: 50 college students, ages ranging between 20 and 24 years, females. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced for 40 min in a day over 1 month. Assessments were taken at baseline and after 1 month of bhramari pranayama. Variables: Haemoglobin, alpha-EEG. |
The results showed a significant increase in haemoglobin and alpha-EEG after the practice. |
| Sujan et al., 2015[68] | Participants: 20 healthy volunteers, ages ranged between 18 and 35 years, both genders. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced for 5 min. Assessments were taken at baseline, during and after 5 min of bhramari pranayama. Variables: Heart rate variability, heart rate and blood pressure. |
The results showed a significant increase in LF/HF ratio during bhramari pranayamacompared to base line. But, following pranayama practise, there is a shift towards parasympathetic activity and decreased LF/HF ratio compared to during practise and baseline. There was also a significant reduction in systolic blood pressure diastolic blood pressure, and heart rate. |
| Patapanchala, 2014[69] | Participants: 90 healthy subjects (30 in Bhasthrika group, 30 in Bhramari group and 30 in the Breath Awareness group), aged between 18 and 25 years, Study design and country: CCT, India. |
Interventions: Bhramari pranayama was performed for 5 min. Assessments were taken at baseline, during and immediately after 5 min. Variables: Heart rate variability. |
There was a significant reduction in Mean RR, VLF and HF, as well as an increase in HR, RMSSD, LF and LF/HF during the practice of Bhramari pranayama. However, a significant increase was seen in Mean RR immediately after practicing Bhramari pranayama. There was also a significant decrease in VLF as well as a significant increase in LF/HF after the practice of Bhramari pranayama compared to Bhasthrika and Breath Awareness. |
| Jin et al., 2014[70] | Participants: 3 subjects with different levels of expertise in bhramari pranayama(i.e. beginner, intermediate and expert level); age and gender were not specified. Study design and country: CCT, Singapore. | Interventions: Bhramari pranayama was practiced for 20 times. Assessments were taken during the practice of bhramari pranayama. Variables: Synchrony of paroxysmal gamma waves. |
The results showed strong synchrony in the temporal lobes for all three subjects. Interestingly, the synchrony increases gradually along the time during bhramari pranayama. Moreover, the distribution of synchrony values depends on the level of expertise in practicing bhramari pranayama; the higher the expertise, the more concentrated the synchrony values. |
| Mooventhan and Khode, 2014[71] | Participants: 82 healthy participants (41 in bhramari group and 41 in the control group), age ranged between 18 and 27 years, both genders. Study design and country: RCT, India. |
Interventions: Bhramari pranayama was practiced for 5 min a day over 2 weeks. Assessments were taken at baseline and after two weeks of bhramari pranayama. Variables: Pulmonary function test. |
The result showed a significant increase in peak expiratory flow, forced expiratory flow 25% and maximal voluntary ventilation, slow vital capacity and forced expired volume in 1 s. |
| Rajesh et al., 2014[72] | Participants: 31 healthy students, ages ranged between 19 and 31 years, males. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 10 min. Assessments were taken at baseline and after bhramari pranayama. Variables: Stop signal reaction time. |
The result showed a significant decrease in stop signal reaction time after bhramari pranayamasession. The Go reaction time increased significantly after bhramari pranayama. |
| Rampalliwar et al., 2013[73] |
Participants: 28 pregnant women, ages ranged between 20 and 28 years, females. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced for 20 min a day over 2 months. Assessments were taken at baseline and after 2 months of bhramari pranayama. Variables: Cardiovascular reactivity to cold pressor test. |
The result showed that practice of bhramari pranayamareduced cardiovascular hyper-reactivity to cold stress after 2 months in pregnant women. |
| Vázquez et al., 2013[74] | Participants: 3 subjects with different levels of expertise in bhramari pranayama(i.e. beginner, intermediate and expert level); age and gender were not specified. Study design and country: CCT, Spain. |
Interventions: Bhramari pranayama was practiced for 20 times. Assessments were taken during the practice of bhramari pranayama. Variables: Paroxysmal gamma waves. |
The result showed an increase in gamma activity in the left temporal lobe during bhramari pranayama. |
| Jain and Rampalliwar, 2011[75] | Participants: 54 healthy medical students, ages ranged between 18 and 24 years, both genders. Study design and country: Single group CT, India. |
Interventions: Bhramari pranayama was practiced 30 times a day over 3 months. Assessments were taken at baseline and after 3 months. Variables: Hyper reactivity to cold pressor. |
The result showed that bhramari pranayamasignificantly reduced the hyper reactivity to cold pressor and diastolic blood pressure. |
| Pandey et al., 2010[76] | Participants: 84 patients with tinnitus; age and gender were not specified. Study design and country: CCT, India. |
Interventions: Bhramari pranayama was practiced for 25 min a day over 8 weeks. Assessments were taken at baseline and after 8 weeks. Variables: Loudness level, tinnitus handicap inventory scores, anxiety and depression scale. |
The result showed that bhramari pranayamasignificantly reduced the loudness level, handicap, depression and anxiety associated with tinnitus. |
| Pramanik et al., 2010[77] | Participants: 50 medical students or staff, ages ranged between 25 and 35 years, both genders. Study design and country: Single group CT, Nepal. |
Interventions: Bhramari pranayama was practiced for 5 min. Assessments were taken at baseline and after 5 min. Variables: Blood pressure and heart rate. |
The result showed a significant decrease in diastolic and mean blood pressure after the practice of bhramari pranayam. |
| Vázquez et al., 2009[78] | Participants: 8 participants, age not specified, males. Study design and country: CCT, Japan. |
Interventions: Bhramari pranayama was practiced for two sessions per day for 31–34 days before the recording session. Assessments were taken during the practice of bhramari pranayama. Variables: EEG paroxysmal gamma waves. |
The result showed generated non-epileptic paroxysmal gamma waves during the practice of Bhramari pranayama. |
| Prasad et al., 2007[79] | Participants: Two subjects, aged 26 years and 35 years, gender not specified. Study design and country: Single group CT, Japan. |
Interventions: Bhramari pranayama was practiced for 10 rounds for each subject. Assessments were taken at baseline, during and after the practice of bhramari pranayama. Variables: Detrended fluctuation analysis on raw EEG. |
The result showed that bhramari pranayamachanges scaling exponents for the raw EEG data in the frontal and temporal regions of the brain. |
| Prasad et al., 2007[80] | Participants: Two subjects, age and gender not specified. Study design and country: Single group CT, Japan. |
Interventions: Bhramari pranayama was practiced for 10–20 rounds for each subject. Assessments were taken at baseline, during and after the practice of bhramari pranayama. Variables: Dipole source localisation in the human cortex for EEG data. |
The result showed symmetric activation in the prefrontal areas during bhramari pranayama, which is largely due to self-humming sound. |
| Prasad et al., 2006[81] | Participants: Two subjects with different levels of expertise in bhramari pranayama, age and gender not specified. Study design and country: Single group CT, Japan. |
Interventions: Bhramari pranayama was practiced for 15–20 rounds for each subject. Assessments were taken at baseline and after the practice of bhramari pranayama. Variables: EEG changes. |
The result observed increased gamma wave pattern in the expertise practitioner immediately after practicing bhramari pranayama. |
CT: Clinical trial, CCT: Clinical controlled trial, RCT: Randomised controlled trial, SDNN: Standard deviation of the N-N intervals, RMSSD: Root mean square of successive differences, NN50: The number of adjacent NN intervals that differ from each other by more than 50 ms, pNN50: Percentage of successive RR intervals that differ by more than 50 ms, LF: Low frequency, HF: High frequency, VLF: Very low frequency, RR: R-wave peak to R-wave peak in electrocardiogram, HR: Heart rate, HRV: Heart rate variability, EEG: Electroencephalography, n.u: Normalized unit
Effect of bhramari pranayama on psychological functions
This review included 24 trials on bhramari pranayama and psychological variables.[37,41,42,44,45,47,50,54-58,62,63,65,67,70,72,74,76,78-81] There were ten single-arm clinical trials, 12 CCTs and two RCTs. Eleven studies were undertaken to examine the very short-term impacts of bhramari pranayama on psychological variables, while another 11 studies investigations were to observe the short-term impacts and two studies to examine the intermediate-term effects of the practise.
Gamma wave patterns were shown to be elevated during the practice of bhramari pranayama in a single-group clinical trial and in two clinical control trials of very short- and short-term duration.[74,78,81] The findings also revealed that bhramari pranayama altered the scaling exponent for raw EEG data in frontal and temporal regions of the brain, symmetric activation in prefrontal regions and stronger temporal lobe synchrony.[70,79,80] Bhramari pranayama practised for a short term resulted in a considerable rise in alpha-EEG after the practice, according to a single-group clinical investigation.[67] Clinical controlled trials’ findings revealed significant improvement in attention performance following bhramari pranayama in a very short duration.[37,47,54] Following the practise of bhramari pranayama, reaction time was also significantly shortened in the very short and intermediate intervals according to three studies, comprising a single-group clinical trial, a clinical control trial and an RCT.[50,65,72] Bhramari pranayama practise was associated with lower levels of stress,[41,44,45] anxiety[41,47,63,76] and depression,[41,76] according to single group clinical trials, clinically controlled trials and an RCT conducted for very short to intermediate periods. Following the practise of bhramari pranayama, single-group clinical trials and clinical controlled trials have shown a significant improvement in sleep quality,[41,44,56] comfort levels,[63] quality of life[41,55] and overall mental health.[42,62] Bhramari pranayama also had a considerable impact on the body’s prakriti (i.e. vata, pitta and kapha), according to two short-term clinical controlled trials.[57,58]
Effect of bhramari pranayama on cardiovascular functions
This review included 22 trials on bhramari pranayama and cardiovascular variables.[36-40,45,46,48,49,51,52,58,60,61,64,66-69,73,75,77] There were nine single-arm clinical trials, ten CCTs and three RCTs. Twelve studies were undertaken to examine the very short-term impacts of bhramari pranayama on cardiovascular variables, while another eight studies investigations were to observe the short-term impacts and two studies to examine the intermediate-term effects of the practise.
Single-group clinical trials, as well as clinical control trials with very short- to short-term follow-up periods, revealed increased heart rate, total peripheral resistant, diastolic blood pressure, and mean arterial pressure with a significant reduction in pulse interval, stroke volume and cardiac output during bhramari pranayama. Following the practice, there were significant drops in heart rate, pulse rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure, rate-pressure product and double product.[38,39,40,46,51,52,64,68,77] Four studies of short-term to intermediate-term duration, including three single group clinical trials and one RCT, showed a reduction in hyper-reactivity to cold pressor test after practicing bhramari pranayama.[45,66,73,75] Short-term results from a clinical controlled trial indicated that bhramari pranayama increased cardiorespiratory endurance.[58] In a short-term period, a single-group clinical trial revealed an increase in haemoglobin.[67] The very short-term effects of bhramari pranayama on cerebral blood flow did not show any significant changes in the middle cerebral artery in the brain.[61]
Single-group clinical trials, clinically controlled trials, and RCTs on heart rate variability performed for very short- to intermediate-term durations revealed a decrease in the RR interval, very low frequency (VLF) and high frequency (HF) as well as an increase in low frequency (LF) and LF to HF ratio during the practise of bhramari pranayama.[36,60,68,69] Following the practise of bhramari pranayama, there was an increase in the RR interval, standard deviation of the N-N intervals (SDNN), root mean square of successive differences (RMSSD) and the number of adjacent NN intervals that differ from each other by more than 50 ms (NN50), percentage of successive RR intervals that differ by more than 50 ms (pNN50) and HF as well as decrease in the LF and LF to HF ratio.[37,38,39,48,49,69]
Effect of bhramari pranayama on pulmonary functions
This review included five trials on bhramari pranayama and pulmonary variables.[43,53,57,59,71] There were three CCTs and two RCTs. All five studies were undertaken to examine the short-term impacts of bhramari pranayama on pulmonary variables.
All lung function metrics increased significantly in a clinical controlled trial and RCTs conducted for short-term duration (i.e. increased in forced vital capacity, forced expiratory volume in 1 s, ratio of forced expiratory volume in 1 s and forced vital capacity, slow vital capacity, forced expiratory flow 25–75% and peak expiratory flow rate).[57,59,71] A reduction in dyspnoea scores and sinonasal outcome scores was observed in short-term clinical controlled trials following the practice of bhramari pranayama in chronic rhinosinusitis and chronic obstructive pulmonary disease patients.[43,53]
Effect of bhramari pranayama on patient population
This review included 15 trials on bhramari pranayama and patient population, including four studies on hypertension,[48,49,51,52] three studies on tinnitus[40,55,76] and one study each on chronic rhinosinusitis,[53] insomnia,[56] visual impairment,[54] menopausal syndrome,[42] pregnancy,[73] chronic obstructive pulmonary disease,[43] asymptomatic COVID-19[41] and dental patient.[63] Three studies were single-arm clinical trials, 11 studies were clinically controlled trials, and one study was RCT. Five studies were undertaken to examine the very short-term impacts, while another nine studies investigations were to observe the short-term impacts and one study to examine the intermediate-term effects of bhramari pranayama.
Clinical controlled trials and an RCT on hypertensive patients observed a significant decrease in systolic blood pressure, LF, and LF to HF ratio as well as an increase in RR interval, standard deviation of the N-N intervals (SDNN), root mean square of successive differences (RMSSD) and the number of adjacent NN intervals that differ from each other by more than 50 ms (NN50), percentage of successive RR intervals that differ by more than 50 ms (pNN50) and HF after the practice of bhramari pranayama in very short-term and intermediate-term period.[48,49,51,52] The results of short-term clinical controlled trials on tinnitus patients showed that practising bhramari pranayama significantly reduced tinnitus annoyance, tinnitus loudness, tinnitus handicap, depression and anxiety associated with tinnitus and improved quality of life in tinnitus patients.[40,55,76] Single-arm clinical trials and clinical controlled trials revealed improvement in sleep quality in insomnia patients,[56] attention performance in visual impairment students[54] and clinical symptoms in patients with menopausal syndrome.[42] In asymptomatic COVID-19 patients and dental patients, bhramari pranayama practise reduced depression, anxiety and stress and improved sleep quality, comfort level and quality of life.[41,63] Short-term single-arm clinical trials and clinical controlled trials have shown a reduction in the sinonasal outcome scores in patients with chronic rhinosinusitis,[53] a reduction in dyspnoea scores in patients with the chronic obstructive pulmonary disease[43] and a reduction in the cardiovascular hyper-reactivity to cold stress in pregnant women after practicing bhramari pranayama.[73]
Adverse events
No adverse events or harmful effects were noted in any of the studies of bhramari pranayama included in our review.
DISCUSSION
Bhramari Pranayama, often known in English as ‘bumblebee breathing’ (because the word ‘bhramara’ means ‘bee’ in Sanskrit), is an ancient yoga technique discussed and practiced according to the two classical yoga texts Hatha Yoga Pradipika and Gheranda Samhita.[6,7] The majority of the included studies used these two popular yoga manuals as practice instructions rather than providing descriptions of any intensive practices performed by participants with a detailed specific approach. Studies discussing the techniques of bhramari pranayama state that the practice involved deep inhalation followed by a prolonged exhalation (the I/E ratio was 1:3, meaning that the inhalation lasted about 5 s and exhalation lasted approximately 15 s), the breath rate was approximately 3–6 breaths/min and, during exhalation, participants produced a specific sound (such as the sound of bee humming, OM or Mmmm). During the practice, participants also covered both of their ears with their thumbs or index fingers. In the included studies, the average daily practice of bhramari pranayama was 16.56 ± 12.88 min. Most studies (n = 43, or 93.48%) focused on the short term (up to 3 months), with a lesser number of studies (n = 3, or 6.52%) focused on the intermediate term (up to 12 months) and no studies were conducted with long-term follow-up (i.e. >12 months).[36-81]
In comparison to the number of RCTs (n = 6, or 13.04%), the number of single-arm clinical trials (n = 18, or 39.19%) and CCTs (n = 22, or 47.83%) was significantly higher among the included studies. RCTs are often considered the most effective type of study when establishing efficacy in a research context since they limit confounders and reduce selection bias. One of the many problems with the single-arm clinical trial design is that it might be challenging to determine the intervention’s effects. While CCT designs can lead to variability within and between participants, they are attractive because they allow for dependable treatment group comparisons.[82,83] The discussion of the results was therefore limited to reviews of RCTs and CCTs to assess the efficacy of the included studies.
The included RCTs provided the most reliable evidence of the effects of bhramari pranayama on alterations in heart rate variability, stress, reaction time and pulmonary functioning. The results of bhramari pranayama practice indicate a decrease in sympathetic activity and an increase in parasympathetic and vagal activity. These changes can be seen in the time domain and frequency domain metrics of heart rate variability (i.e. an increase in RR interval, SDNN, RMSSD, NN50, PNN50 and HF, while a decrease in LF and LF/HF ratio).[39,49] This suggests practicing bhramari pranayama results in a beneficial shift in cardiac autonomic regulation toward parasympathetic dominance. The application of bhramari pranayama in enhancing cardiac-autonomic function was demonstrated by its ability to improve sympathetic balance. This benefit was reinforced by both frequency domain and time domain parameter indices.[84] The results were confirmed by the reduction in stress through a drop in salivary cortisol levels.[45] Improvements in attention performance and reaction time are indicative of the beneficial effects of bhramari pranayama on cognitive functions, particularly the ability to control limited computational resources flexibly.[85] This is demonstrated by improvements in reaction time in both auditory and visual reaction times.[50] The practice of bhramari pranayama can increase the air space in the lungs, strengthen the muscles of the respiratory system, increase the elastic properties of the lungs and improve its ventilatory capabilities based on improvement in pulmonary function parameters.[59,71] Bhramari pranayama can, therefore, be helpful for improving respiratory fitness and for people who participate in aerobic-based sports (e.g., athletes, swimmers and hikers).[86]
Bhramari pranayama was found to be effective on psychological parameters in the included CCTs, which also showed that it reduced anxiety and depression and increased quality of life, comfort level, sleep quality, attention performance and reaction speed.[37,54-56,63,72,76] Changes in heart rate variability (i.e. increased in RR interval, SDNN, HF and decreased in LF and VLF), as well as decreases in systolic and diastolic blood pressure, provided evidence of a positive shift toward parasympathetic dominance in cardiac autonomic modulation after practicing bhramari pranayama.[36,40,48,51,52,64,69] This suggests that practicing bhramari pranayama regularly can improve cognitive efficiency and help people feel less anxious, worried and depressed. It can be applicable in offices, classrooms and high-pressure environments to reduce work pressure. While practicing bhramari pranayama, higher non-epileptic paroxysmal gamma wave patterns indicated the detection of non-epileptic hypersynchrony, which was supported by the included CCTs.[70,74,78] This increased gamma brain activity is ideally associated with higher information processing, including working memory, attention, learning, consciousness and other cognitive functions.[87,88]
Furthermore, the CCTs also provided evidence that bhramari pranayama would be quite beneficial for individuals with tinnitus and hypertension. Tinnitus patients who practiced bhramari pranayama experienced significant improvements in their quality of life as well as significantly reduced levels of tinnitus-related sadness, anxiety and disability.[40,55,76] In hypertensive patients, this practice was found to be effective in increasing parasympathetic activity and reducing blood pressure.[48,49,51,52] A small number of CCTs provided evidence that this practice could be beneficial for chronic respiratory disorders such as chronic rhinosinusitis and chronic obstructive pulmonary disease. This pranayama has been found to lower dyspnoea scores in patients with chronic obstructive pulmonary disease, lower the sinonasal outcome scores in patients with chronic rhinosinusitis and improve the quality of sleep in patients with insomnia.[43,53,56]
Limitations
A limitation of this review is that the quality of the included studies was not assessed; nevertheless, it covered a wide range of clinical trials on bhramari pranayama and received a large number of citations, making it a valuable resource for individuals interested in research on this topic. To establish efficacy in a research setting, only RCTs and CCTs were considered robust study designs that minimise selection bias and distribute confounders. However, depending on the quality of the included research, the conclusions may or may not be stronger. It was not studied whether bhramari pranayama has any long-term effects during long-term follow-up, and fewer of the included research were designed as RCTs. A universal standardisation of bhramari pranayama practices throughout the research is necessary, as the practice guidelines and methodologies varied among the included studies.
Thus, more thorough RCTs with long-term follow-up are required in this area to determine whether bhramari pranayama practice will be advantageous in the long run. In addition, more RCTs are required in this field to confirm the practice’s efficacy in clinical conditions (such as tinnitus, hypertension, chronic obstructive pulmonary disease, chronic rhinosinusitis and insomnia). Future research could address these limitations and assess the mechanisms underlying the effects of bhramari pranayama in more clinical settings, especially within the field of experimental and cognitive psychology.
CONCLUSION
The findings indicated that bhramari pranayama has a positive impact on psychological, cardiovascular and pulmonary health; it also helps individuals with tinnitus and hypertension by reducing associated symptoms. It is discovered to be associated with lower levels of stress, anxiety, depression, sympathetic activity and blood pressure, and higher levels of attention, quality of sleep, parasympathetic activity, vagal activity and pulmonary functioning. This thorough assessment of the literature examined every experimental study on the effects of bhramari pranayama on both general health and specific medical disorders. Researchers can identify shortcomings in the current literature and conduct more rigorous experiments on bhramari pranayama for future research that addresses the above shortcomings using this review of literature on bhramari pranayama.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- General features, techniques, and benefits of pranayamas mentioned in traditional hatha yoga texts: A review on pranayama chapters. Yoga Mimamsa. 2022;54:1-7.
- [CrossRef] [Google Scholar]
- Effects of yogic breath regulation: A narrative review of scientific evidence. J Ayurveda Integr Med. 2019;10:50-8.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring the therapeutic benefits of pranayama (yogic breathing): A systematic review. Int J Yoga. 2020;13:99-110.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of various pranayama on cardiovascular and autonomic variables. Anc Sci Life. 2016;36:72-7.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of practice guidelines for yoga breathing from the traditional texts and PubMed indexed research. Int J Yoga Therap. 2022;32:1-16.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of yoga and meditation on tinnitus: A systematic review. J Laryngol Otol. 2021;135:284-7.
- [CrossRef] [PubMed] [Google Scholar]
- Bhramari pranayama (humming bee breath) exercise as an effort to release stress during the covid-19 pandemic. Guna Widya J. 2022;9:64-73.
- [CrossRef] [Google Scholar]
- Role of bhramari pranayama in generalised anxiety disorder. Int J Res Indian Med. 2021;5:1-6.
- [CrossRef] [Google Scholar]
- Bhramari pranayama-A simple lifestyle intervention to reduce heart rate, enhance the lung function and immunity. J Ayurveda Integr Med. 2021;12:562-4.
- [CrossRef] [PubMed] [Google Scholar]
- Nitric oxide, humming and bhramari pranayama. Indian J Sci Technol. 2023;16:377-84.
- [CrossRef] [Google Scholar]
- Bhramari pranayama as an aid to meditation: A review of classical yoga texts. Int J Yoga Philosop Psychol Parapsychol. 2020;8:58.
- [CrossRef] [Google Scholar]
- Effect of bhramari pranayama on dimensions of health: A meta-analysis. Indian J Anc Med Yoga. 2017;10:49.
- [Google Scholar]
- Effects of bhramari pranayama on health-A systematic review. J Tradit Complement Med. 2017;8:11-6.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in auditory threshold of hearing after bhramari pranayama In: SICE annual conference. New Jersey: IEEE; 2007. p. :1819-22.
- [Google Scholar]
- Does humming sound play healing role in bhramari pranayama In: SCIS and ISIS SCIS and ISIS. Japan: Japan Society for Fuzzy Theory and Intelligent Informatics; 2006. p. :1983-8.
- [Google Scholar]
- Acoustic description of bhramari pranayama. Indian J Otolaryngol Head Neck Surg. 2022;74:4738-47.
- [CrossRef] [PubMed] [Google Scholar]
- Short term effects of four-weeks of bhramari pranayama on aerobic fitness of young boys. Int J Yogic Hum Mov Sports Sci. 2019;4:757-60.
- [Google Scholar]
- A preliminary study on the effect of bhramari pranayama on voice of prospective singers. J Voice. 2022;22:143-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of bhramari pranayama on the acoustic and aerodynamic parameters of voice in normophonic females. Evid Based Complement Alternat Med. 2018;18:4176803.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of various breathing exercises (pranayama) in patients with bronchial asthma of mild to moderate severity. Int J Yoga. 2009;2:22-5.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of pranayamic breathing as a positive psychology exercise on foreign language learning anxiety and test anxiety among language learners at tertiary level. Front Psychol. 2021;12:742060.
- [CrossRef] [PubMed] [Google Scholar]
- Healing for baby blues syndrome and post-partum depression via chandra namaskara and brahmari pranayama. J Yoga Dan Kesehatan. 2018;1:1-4.
- [CrossRef] [Google Scholar]
- Cardiovascular reactivity to stress in long-term yoga practitioners. J Family Med Prim Care. 2023;12:383-7.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of short term pranayam practice on breathing rate and ventilatory functions of lung. Indian J Physiol Pharmacol 1992:36105-8.
- [Google Scholar]
- Effect of bhramari pranayama and physical exercises on physical and mental health of undergraduate players. PhD thesis. Banaras Hindu University.
- [Google Scholar]
- Effect of slow deep breathing exercise bhramari pranayama method on blood pressure and mean arterial pressure. Doctoral dissertation. Universitas Jenderal Soedirman.
- [Google Scholar]
- A systematic review of the effects of bhramari pranayama on the central and autonomic nervous system. Bachelor dissertation. Auckland University of Technology.
- [Google Scholar]
- The acute therapeutic effect of bhramari pranayama on autonomic function and self-reported anxiety. Doctoral dissertation. University of Pittsburgh.
- [Google Scholar]
- Humming technique for resident well-being. 2017. Available from: https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=humming+technique+for+resident+well-being%2C+Yadav&btnG=
- [Google Scholar]
- Effect of specialised ayurvedic protocol in stress-induced hypertension: A case series. Asian J Cardio Res. 2023;8:13-7.
- [Google Scholar]
- Effect of yogic breathing techniques on cardio autonomic function in patient with right bundle branch block-A case report. J Cardiovasc Dis Res. 2023;14:389-95.
- [Google Scholar]
- Humming (simple bhramari pranayama) as a stress buster: A holter-based study to analyze heart rate variability (HRV) parameters during bhramari, physical activity, emotional stress, and sleep. Cureus. 2023;15:37527.
- [CrossRef] [PubMed] [Google Scholar]
- P300 following four voluntarily regulated yoga breathing practices and breath awareness. Clin EEG Neurosci. 2023;54:117-29.
- [CrossRef] [PubMed] [Google Scholar]
- A study on immediate and training effect of bhramari pranayama on heart rate variability in healthy adolescents. Biomedicine. 2022;42:784-8.
- [CrossRef] [Google Scholar]
- Effect of deep breathing exercise on heart rate variability in young adults-randomised controlled trial. Int J Pharm Clin Res. 2022;14:539-46.
- [Google Scholar]
- Autonomic functions, tinnitus annoyance and loudness, and quality of life: Randomized-controlled responses to bee-humming (vibrational) respiratory training in tinnitus elderly. Complement Ther Clin Pract. 2022;48:101611.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of bhramari pranayama intervention on stress, anxiety, depression and sleep quality among COVID 19 patients in home isolation. J Ayurveda Integr Med. 2022;13:100596.
- [CrossRef] [PubMed] [Google Scholar]
- Evolution of bhramari pranayam in the management of menopausal syndrome. Ayushdhara. 2020;7:2791-7.
- [CrossRef] [Google Scholar]
- Efficacy of bhramari pranayama on dyspnoea among the patients with chronic obstructive pulmonary disease. Indian J Public Health Res Dev. 2021;12:147-52.
- [CrossRef] [Google Scholar]
- Effect of short-term practice of bhramari pranayama on sleep quality and perceived stress in school students. Int J Physiol. 2021;9:1-6.
- [CrossRef] [Google Scholar]
- Effect of six months pranayama training on stress-induced salivary cortisol response among adolescents-randomized controlled study. Explore (NY). 2022;18:463-6.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of cardiovascular functions during the practice of different types of yogic breathing techniques. Int J Yoga. 2021;14:158-62.
- [CrossRef] [PubMed] [Google Scholar]
- Volitional yoga breathing influences attention and anxiety: An exploratory randomized crossover study. Complement Med Res. 2022;29:120-6.
- [CrossRef] [PubMed] [Google Scholar]
- A randomized trial of the immediate effect of bee-humming breathing exercise on blood pressure and heart rate variability in patients with essential hypertension. Explore (NY). 2021;17:312-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of yoga breathing practice on heart rate variability in healthy adolescents: A randomized controlled trial. Integr Med Res. 2020;9:28-32.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of bhramari pranayama practice on simple reaction time in healthy adolescents-A randomized control trial. Int J Adolesc Med Health. 2020;33:547-50.
- [CrossRef] [PubMed] [Google Scholar]
- Immediate effect of buteyko breathing and bhramari pranayama on blood pressure, heart rate and oxygen saturation in hypertensive patients: A comparative study. Indian J Forensic Med Toxicol. 2020;14:7106.
- [CrossRef] [Google Scholar]
- To find out immediate effect of bhramari pranayama on blood pressure, heart rate and oxygen saturation in hypertensive patients. Int J Curr Res Rev. 2020;12:193-7.
- [CrossRef] [Google Scholar]
- The efficacy of yogic breathing exercise bhramari pranayama in relieving symptoms of chronic rhinosinusitis. Int J Yoga. 2019;12:120-3.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of yogic breathing on accommodate braille version of six-letter cancellation test in students with visual impairment. Int J Yoga. 2018;11:111-5.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency-modulated bhramari pranayam in tinnitus and deafness. Indian J Otol. 2018;24:209-13.
- [Google Scholar]
- Assessment of nidra as adharniya vega and its management with bhramari pranayam. World J Pharm Res. 2017;7:1527-41.
- [Google Scholar]
- Effect of bhramari pranayama on certain physical and physiological parameters among the club level cricket players with special reference to prakriti psycho somatic constitutions. PhD thesis. Banaras Hindu University.
- [Google Scholar]
- Impact of bhramari pranayama on cardio respiratory endurance among the cricket players with special reference to prakriti (psycho-somatic constitution) Int J Phy Edu Sports. 2017;2:8-13.
- [Google Scholar]
- Effect of bhramari pranayama practice on pulmonary function in healthy adolescents: A randomized control study. Anc Sci Life. 2017;36:196-9.
- [CrossRef] [PubMed] [Google Scholar]
- Heart rate variability changes during and after the practice of bhramari pranayama. Int J Yoga. 2017;10:99-102.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebrovascular hemodynamics during the practice of bhramari pranayama, kapalbhati and bahir-kumbhaka: An exploratory study. Appl Psychophysiol Biofeedback. 2018;43:87-92.
- [CrossRef] [PubMed] [Google Scholar]
- Interventional effect of bhramari pranayama on mental health among college students. Int J Ind Psychol. 2017;4:29-33.
- [CrossRef] [Google Scholar]
- The effect of short yoga intervention on the anxiety and comfort level of dental patients reporting for extraction. Int Sci Yoga J Sense. 2016;6:6-13.
- [Google Scholar]
- Immediate effects of bhramari pranayama on resting cardiovascular parameters in healthy adolescents. J Clin Diagn Res. 2016;10:17-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of brahmari pranayama on visual reaction time. J Evol Res Hum Physiol. 2016;2:1-3.
- [Google Scholar]
- Effect of bhramari pranayama and yoga nidra on cardiovascular hyper-reactivity to cold pressor test. Int J Med Sci Res Pract. 2015;2:24-6.
- [Google Scholar]
- The effect of bhramari pranayama and jyoti dhyan effect on alpha EEG and hemoglobin of college going students. Int J Phys Educ Sports Health. 2015;1:40-4.
- [Google Scholar]
- Effect of bhramari pranayama (humming bee breath) on heart rate variability and hemodynamic-A pilot study. Auton Neurosci. 2015;192:82.
- [CrossRef] [Google Scholar]
- Immediate effect of bhasthrika and bhramari pranayamas on autonomic and respiratory variables in healthy individuals-A randomized controlled trial. J Res Educ Indian Med. 2014;26:1.
- [Google Scholar]
- Synchrony analysis of paroxysmal gamma waves in meditation EEG In: IEEE international conference on acoustics, speech and signal processing (ICASSP). New Jersey: IEEE; 2014. p. :4703-7.
- [CrossRef] [Google Scholar]
- Effect of bhramari pranayama and OM chanting on pulmonary function in healthy individuals: A prospective randomized control trial. Int J Yoga. 2014;7:104-10.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of bhramari pranayama on response inhibition: Evidence from the stop signal task. Int J Yoga. 2014;7:138-41.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of bhramari pranayama on pregnant women having cardiovascular hyper-reactivity to cold pressor. Natl J Physiol Pharm Pharmacol. 2013;3:137-41.
- [CrossRef] [Google Scholar]
- Automated detection of paroxysmal gamma waves in meditation EEG In: IEEE international conference on acoustics, speech and signal processing. New Jersey: IEEE; 2013. p. :1192-6.
- [CrossRef] [Google Scholar]
- Effect of bhramari pranayama on volunteers having cardiovascular hyper-reactivity to cold pressor test. J Yoga Phys Ther. 2011;1:1-4.
- [CrossRef] [Google Scholar]
- Role of self-induced sound therapy: Bhramari pranayama in tinnitus. Audiol Med. 2010;8:137-41.
- [CrossRef] [Google Scholar]
- Immediate effect of a slow pace breathing exercise bhramari pranayama on blood pressure and heart rate. Nepal Med Coll J. 2010;12:154-7.
- [Google Scholar]
- EEG paroxysmal gamma waves during bhramari pranayama: A yoga breathing technique. Conscious Cogn. 2009;18:977-88.
- [CrossRef] [PubMed] [Google Scholar]
- Hummgenic changes in large scale temporal correlation of EEG in BP In: SICE annual conference. New Jersey: IEEE; 2007. p. :2068-73.
- [Google Scholar]
- Source localization with EEG data for BP shows major activities in the frontal areas of the brain In: SICE annual conference. New Jersey: IEEE; 2007. p. :774-8.
- [Google Scholar]
- EEG changes after bhramari pranayama In: SCIS and ISIS SCIS and ISIS. Japan: Japan Society for Fuzzy Theory and Intelligent Informatics; 2006. p. :390-5.
- [Google Scholar]
- Clinical trial structures. J Exp Stroke Transl Med. 2010;3:8-18.
- [CrossRef] [PubMed] [Google Scholar]
- Randomised controlled trials-the gold standard for effectiveness research: Study design: Randomised controlled trials. BJOG. 2018;125:1716.
- [CrossRef] [PubMed] [Google Scholar]
- Heart rate variability, health and well-being: A systems perspective. Front Public Health. 2019;7:323.
- [CrossRef] [PubMed] [Google Scholar]
- Attention in psychology, neuroscience, and machine learning. Front Comput Neurosci. 2020;14:29.
- [CrossRef] [PubMed] [Google Scholar]
- Designing EEG experiments for studying the brain: Design code and example datasets. Cambridge, Massachusetts: Academic Press; 2017. p. :1-30.
- [CrossRef] [Google Scholar]
- Introduction to EEG-and speech-based emotion recognition. Cambridge, Massachusetts: Academic Press; 2016. p. :51-79.
- [CrossRef] [Google Scholar]







